Posterior decompression techniques in the thoracolumbar spine
1. Introduction
Preliminary remarks
Decompression is often an important part of the surgery. It should be understood that this is a step that can also result in deterioration of neurology unless very meticulously performed.
While it is commonly accepted that all patients with complete or incomplete neurology require decompression, the role of this procedure in patients with intact neurology is still controversial.
All the decompression techniques described here are illustrated with an exemplary A4 fracture. However, these techniques are equally valid for all other fracture types.
Techniques
Decompression techniques can be broadly classified as direct and indirect.
Indirect decompression is based on the ligamentotaxis principle of fracture reduction, where the retropulsed bone fragments fall back into the fractured vertebral body enabling decompression of the spinal canal indirectly.
In direct techniques, the spinal canal is enlarged by partial laminectomy (laminotomy) or complete laminectomy and removal of compressing bone fragments.
2. Neurological deficit
Neurological evaluation
The neurological assessment must be carried out as described in the neurological evaluation.
Neurological deficit in a patient with spinal cord injury is primarily determined at the time of accident to the spinal cord. Hence, decompression may not have a direct bearing with respect to neurological recovery. But in the presence of cord compression due to retropulsed bone fragments and neurological deficit, decompression is performed to provide the optimal environment for the neural structures to recover.
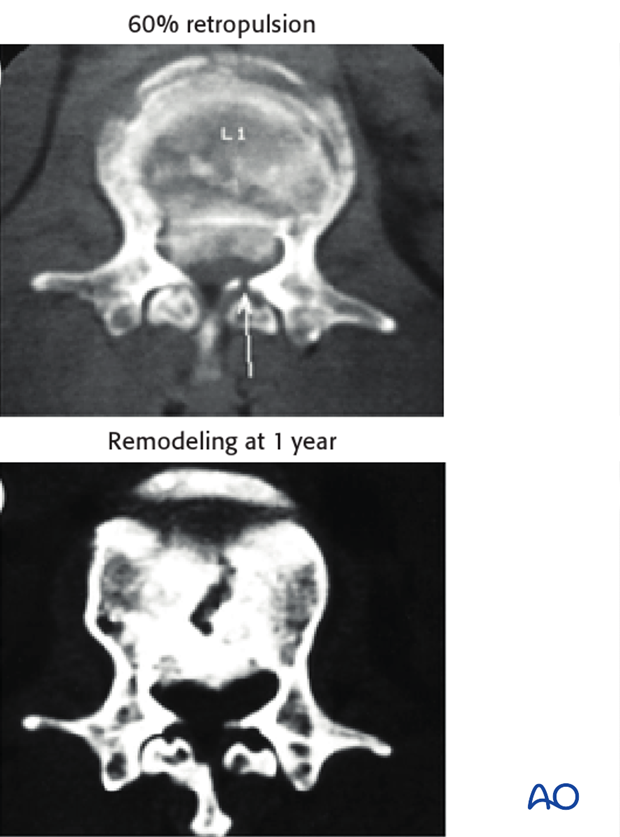
No neurological deficit
Most surgeons agree that whatever the extent of canal compromise, decompression is rarely required when the patient has no neurological deficit. Here, indirect spinal canal decompression through ligamentotaxis achieved by fracture reduction through distraction and lordosis is usually sufficient. Spontaneous absorption and remodeling of the canal have been documented.
Neurological deficit
In patients with complete or incomplete neurological deficit, in the presence of canal compromise, one of the decompression techniques described as follows can be used.
3. Indirect decompression: Ligamentotaxis
Preliminary remarks
Indirect reduction techniques are based on the principle of ‘ligamentotaxis’. Ligamentotaxis refers to the use of intact but buckled posterior longitudinal ligament (PLL) to guide in repositioning the retropulsed fracture fragments by the application of distraction forces.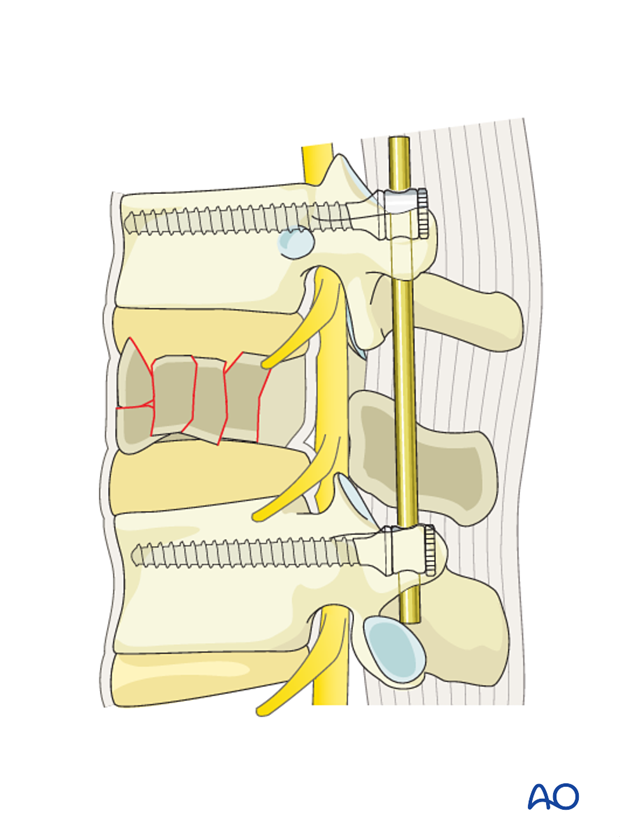
Indications
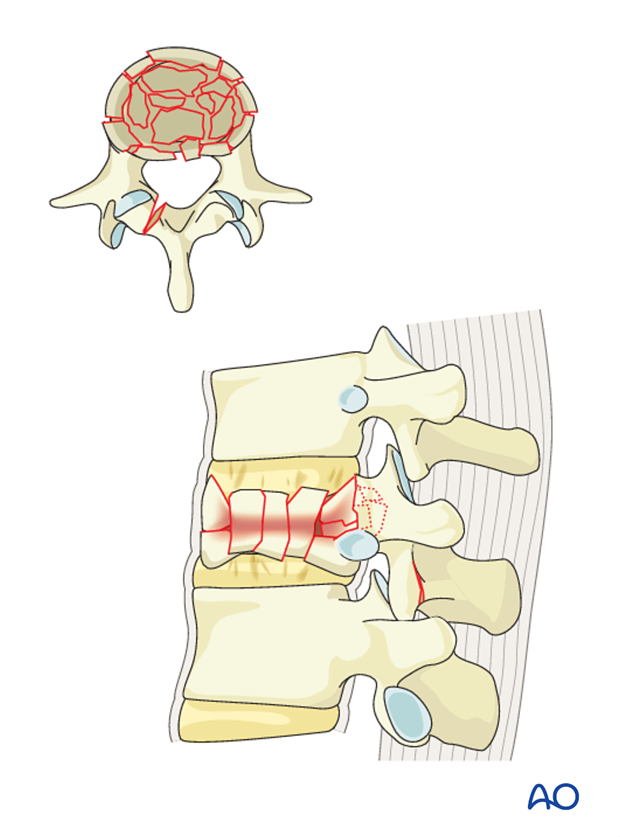
- Only type A fractures
- Fresh fractures
- Retropulsed fragment
Contraindications
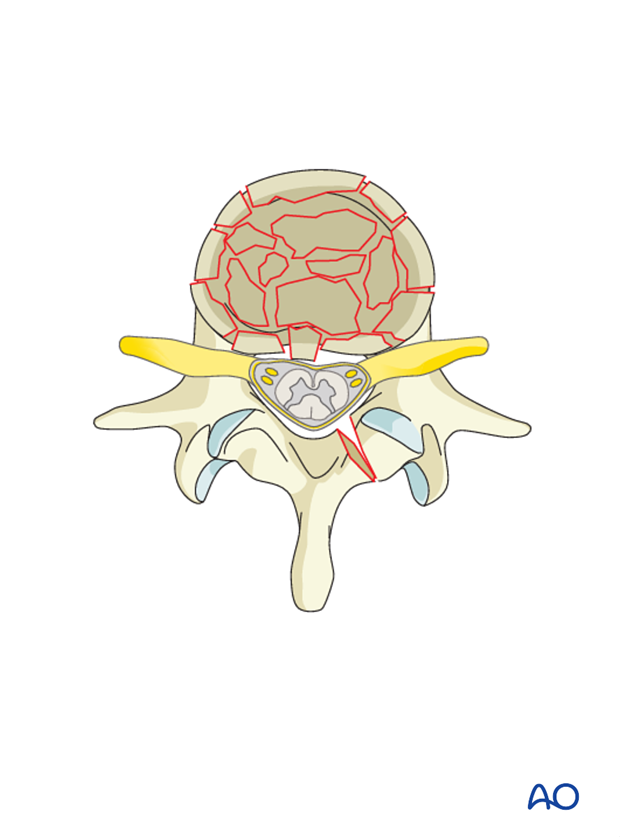
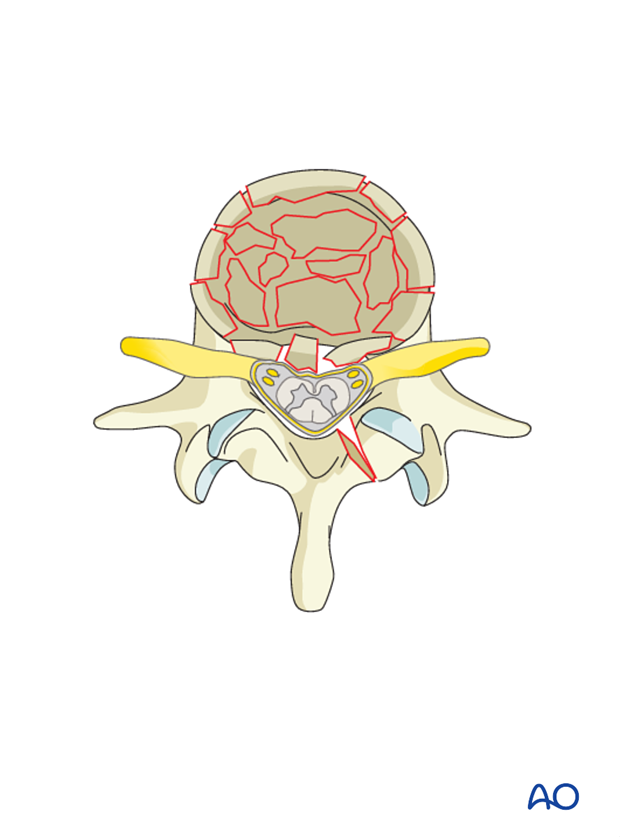
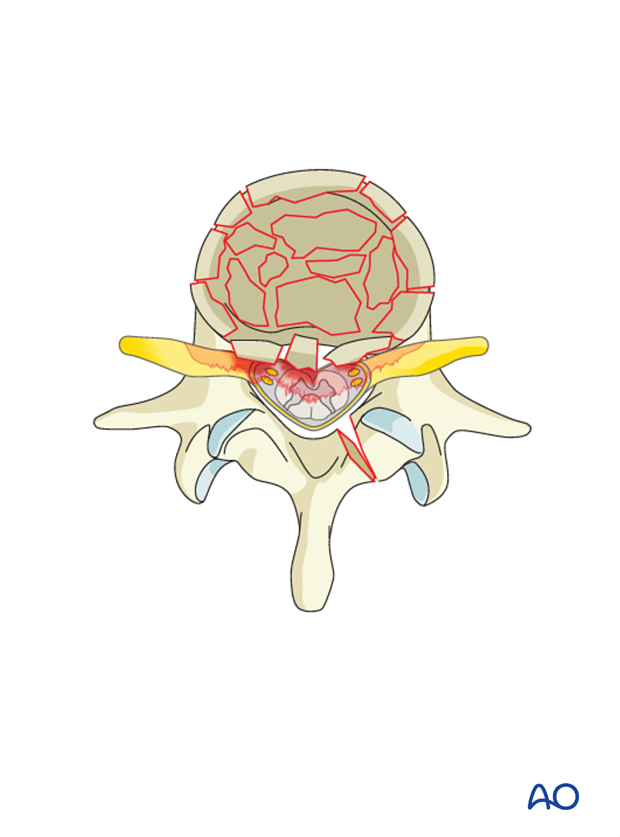
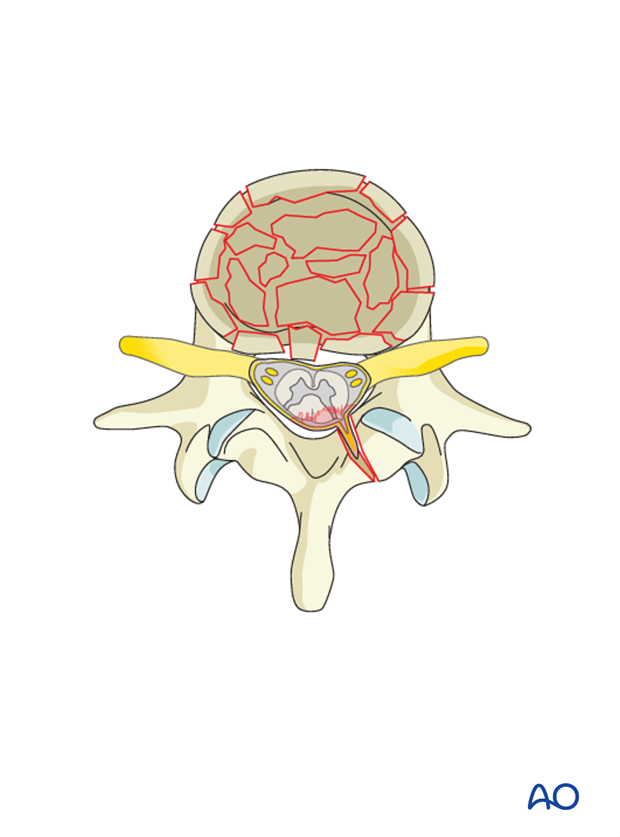
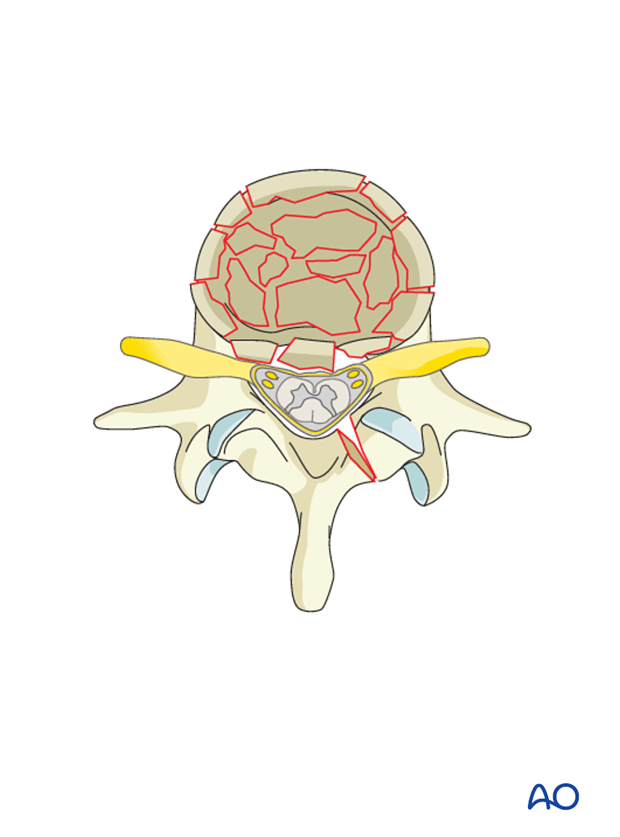
- Reverse cortical sign (retropulsed fragment that has rotated more than 180 degrees so that the cortical surface is opposed to the cancellous surface of the main vertebral body) (shown in the illustration)
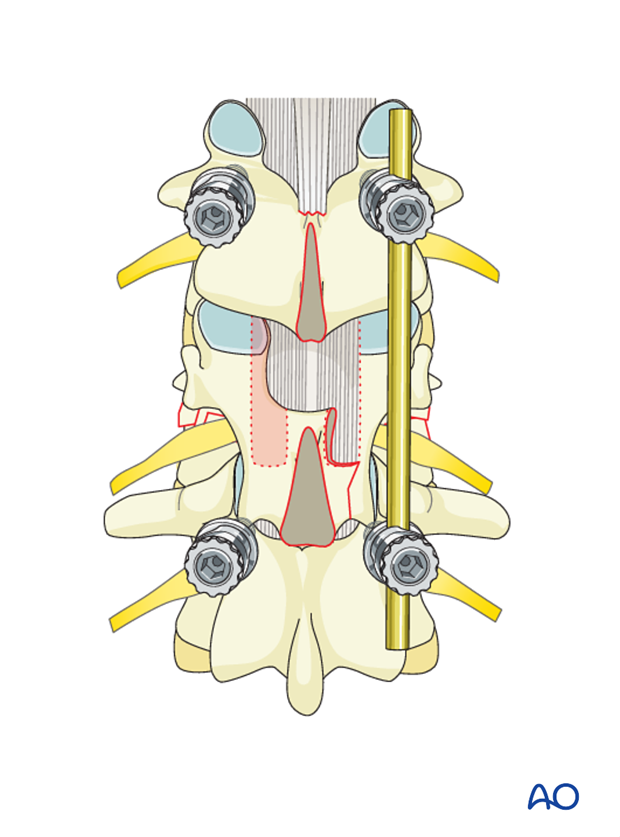
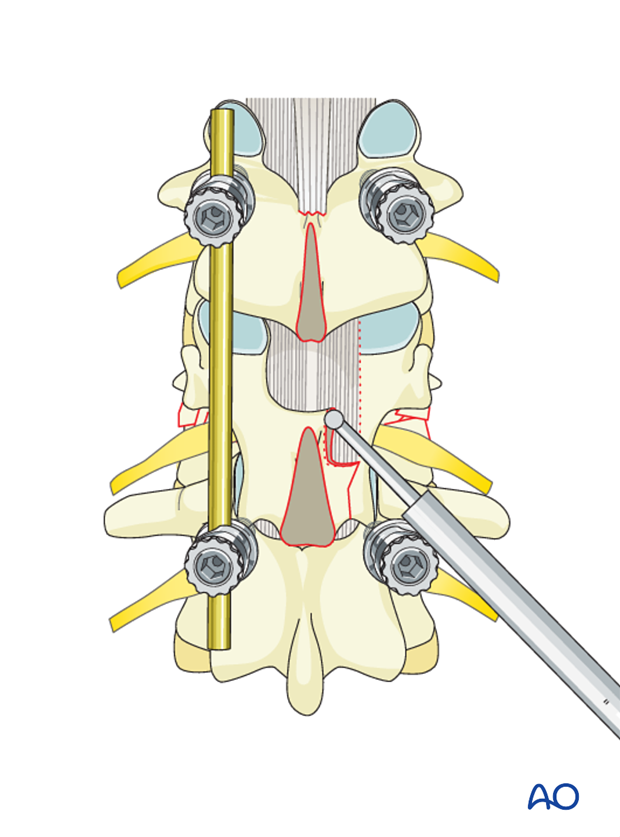
Indirect decompression/ligamentotaxis with pedicle screws
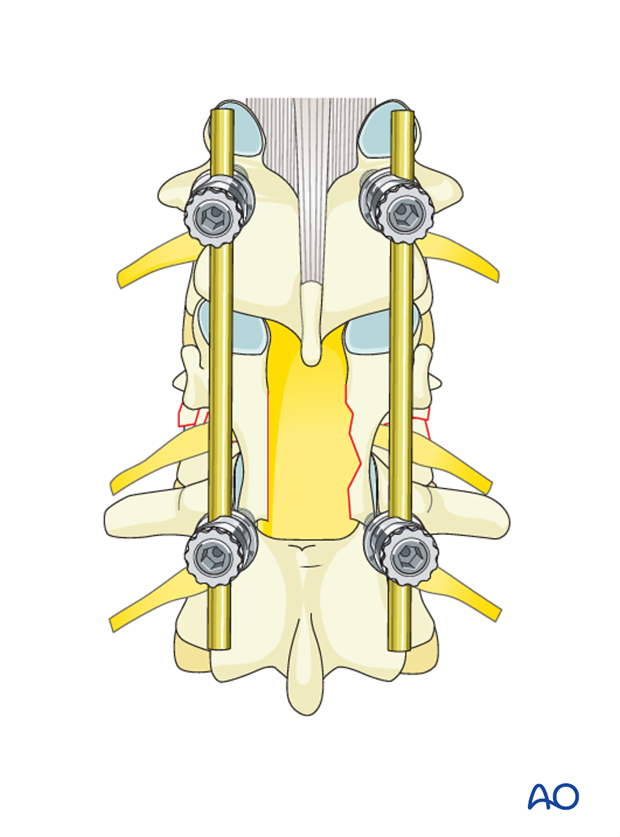
The reduction of the retropulsed fracture fragments achieved through ligamentotaxis enables indirect decompression of the spinal canal.
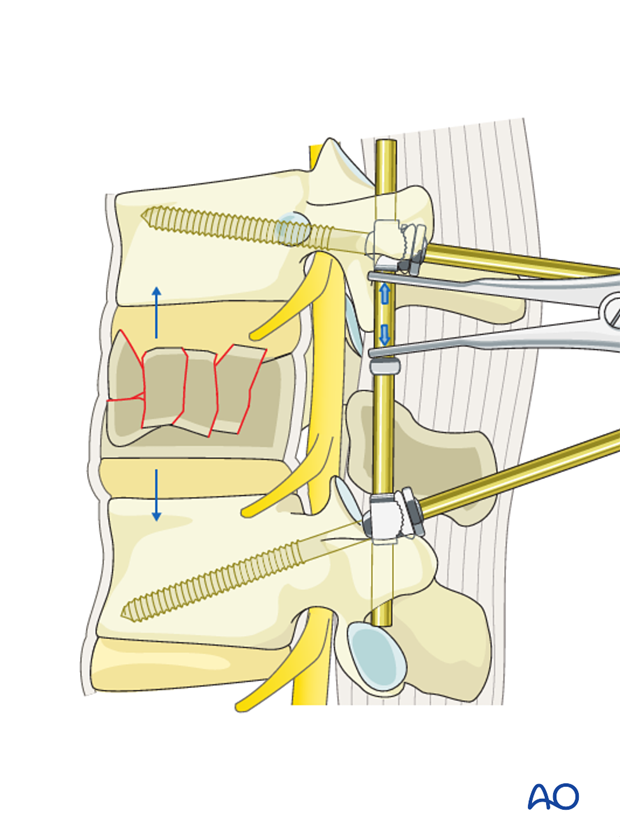
Distraction of the rods should be performed gently and simultaneously on both sides. Sudden and rapid attempts at distraction places significant biomechanical stress on the screws. Asymmetrical distraction can result in unilateral wedging of the vertebral body.

Indirect decompression/ligamentotaxis with schanz screws
With the use of an internal fixator based on Schanz screws, reduction of the fracture achieved through ligamentotaxis enables indirect decompression of the spinal canal.
4. Direct decompression technique: Posterior decompression
Preliminary Remarks
In direct techniques, the spinal canal is enlarged by laminectomy and removal of compressing bone fragments.
This technique can be performed from L1 to L5 levels.
Indications
- Presence of neurological deficit
- Reverse cortical sign (retropulsed fragment that has rotated more than 180 degrees so that the cortical surface is opposed to the cancellous surface of the main vertebral body; ligamentotaxis will not be effective in this instance
Laminectomy: Introduction
Partial or total laminectomy may be performed to approach the spinal canal.
It is also available in cases where there is entrapment of the roots or dural sac by the split laminar fracture.
Pitfall
Laminectomy as an isolated procedure for spinal cord decompression should not be performed as it increases instability and promotes neurological deficit.
Technique
The lamina of the fractured vertebra is removed fully cranio-caudally, leaving 3 mm of bone on either side near the pars.
Laminectomy is started by first detaching the ligamentum flavum from its insertion on the inferior and superior surface of the cephalad lamina with an elevator. The ligamentum flavum is then removed.
The lamina is then removed with the help of bone nibblers and Kerrison rongeurs from below upwards.
Use of an elevator to protect the underlying dura during laminectomy helps in avoiding inadvertent dural injury.
A channel is cut 1 cm into the vertebral body anterior to the medial portion of the pedicle that has been thinned. Reverse-angle curettes can be inserted through this opening, and any bone fragments compressing the anterior neural elements can be impacted into the vertebral body.
Removing the bone fragment is a very delicate procedure and only experienced surgeons should perform it.
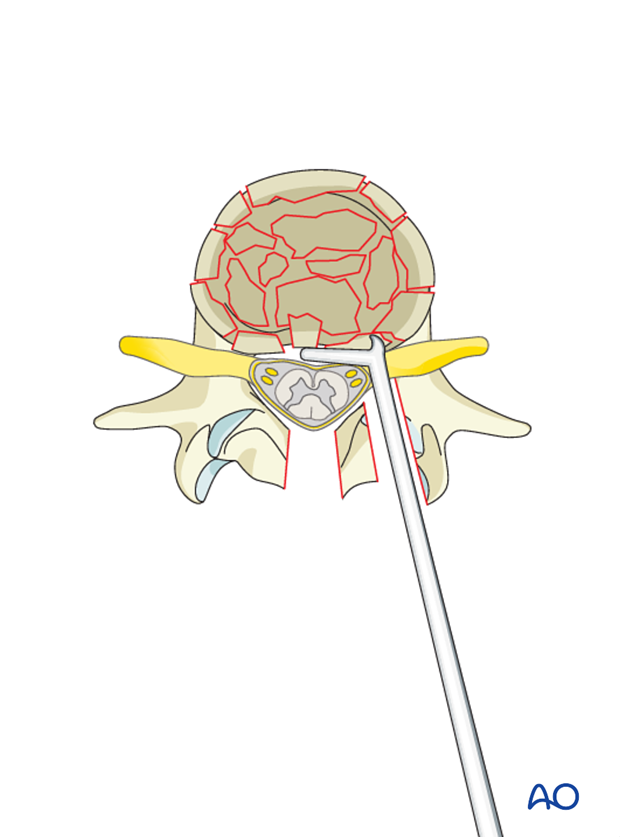
Special tamps/punches can be used to gently push and reposition the fragments back into the broken vertebral body. This helps in constituting the anterior vertebral bone stock and also decompresses the spinal canal.
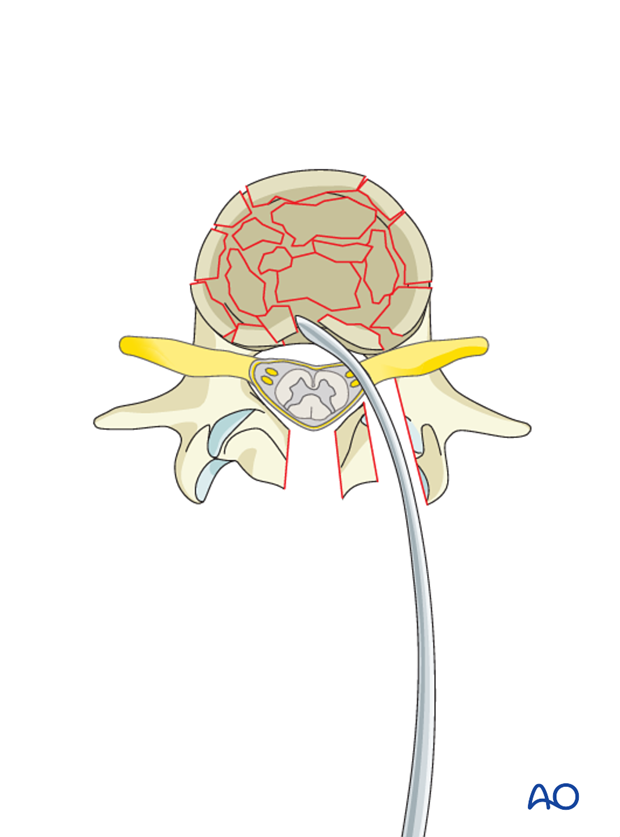
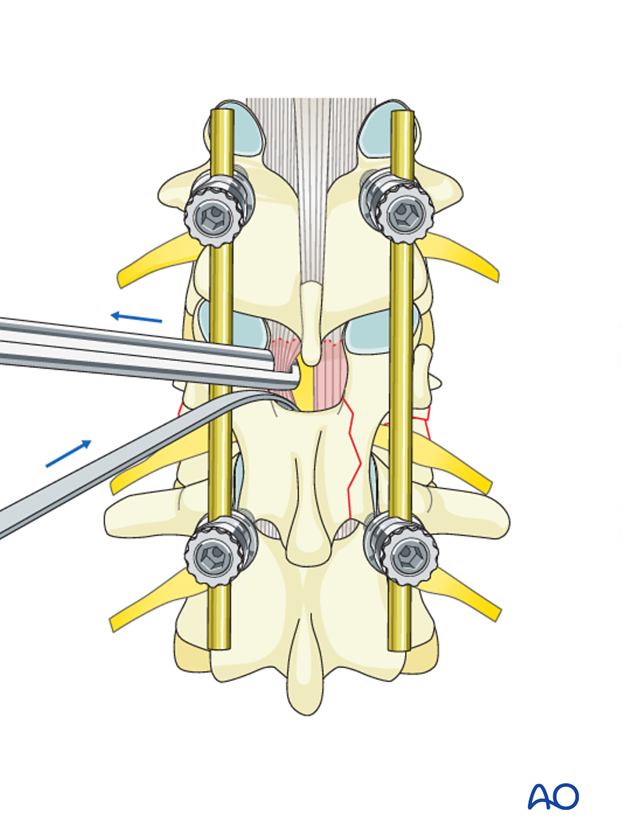
This procedure involves retracting the thecal sac, which has to be done carefully using Penfield elevators.
Pitfall: Use of rongeurs
In patients with canal compromise, especially in the thoracic spine, Kerrison rongeurs must be used with care as they can damage the already compressed neurostructures. It is preferable to use thin rongeurs and to start the decompression from the lateral borders of the lamina, rather than in the middle.
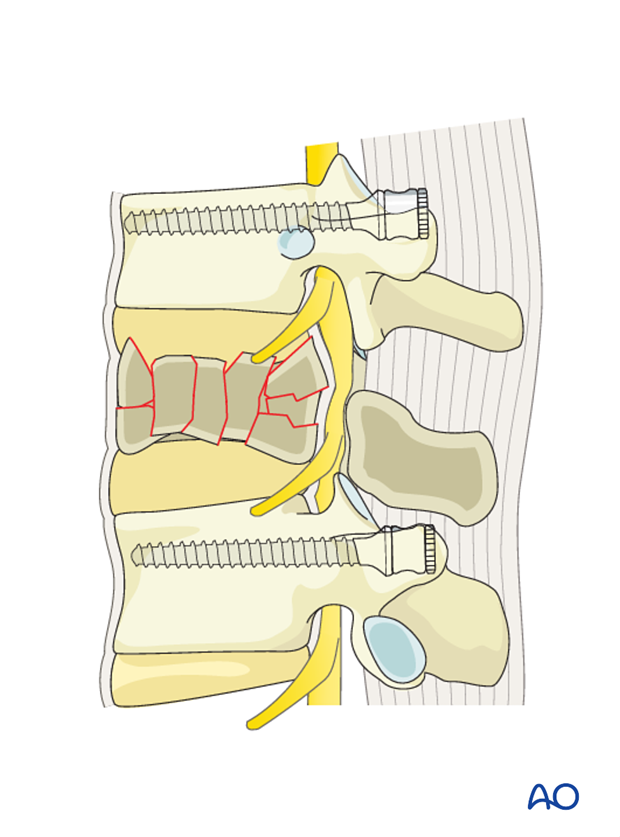
5. Direct decompression technique: Transpedicular decompression
Preliminary remarks
In this technique, instead of a complete laminectomy, decompression is performed through the pedicle. In most burst fractures, maximum canal compromise due to retropulsion of fragments occurs at the level of the pedicle. Hence, posterolateral decompression might be performed transpedicularly.
This technique can be performed from T1 to L5 levels, without the risk of retracting the thecal sac.
Indications
Canal compromise by large retropulsed fragments at the level of the pedicle
Technique
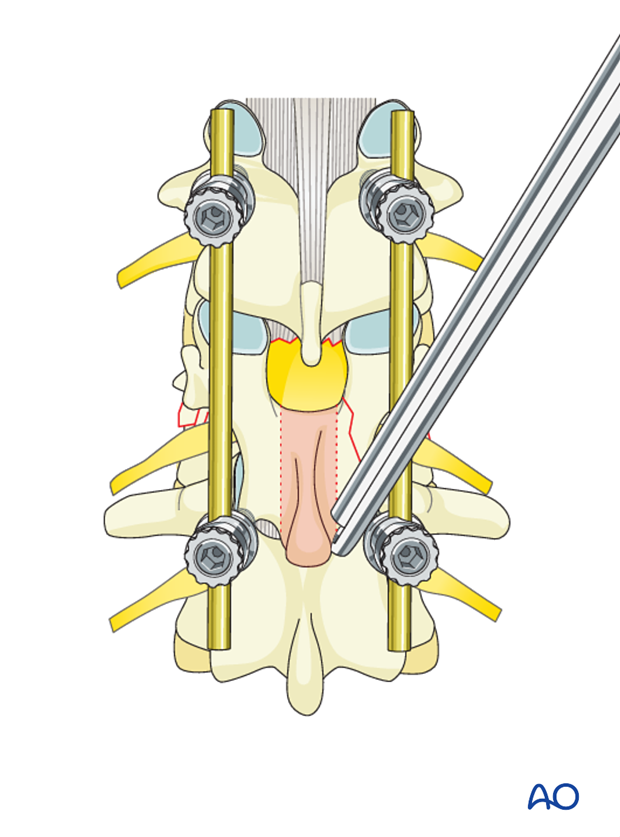
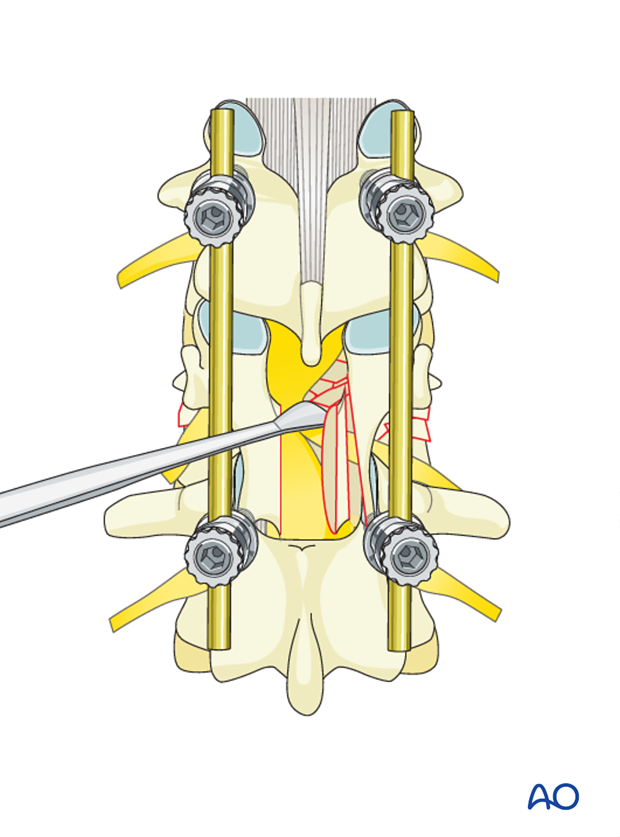
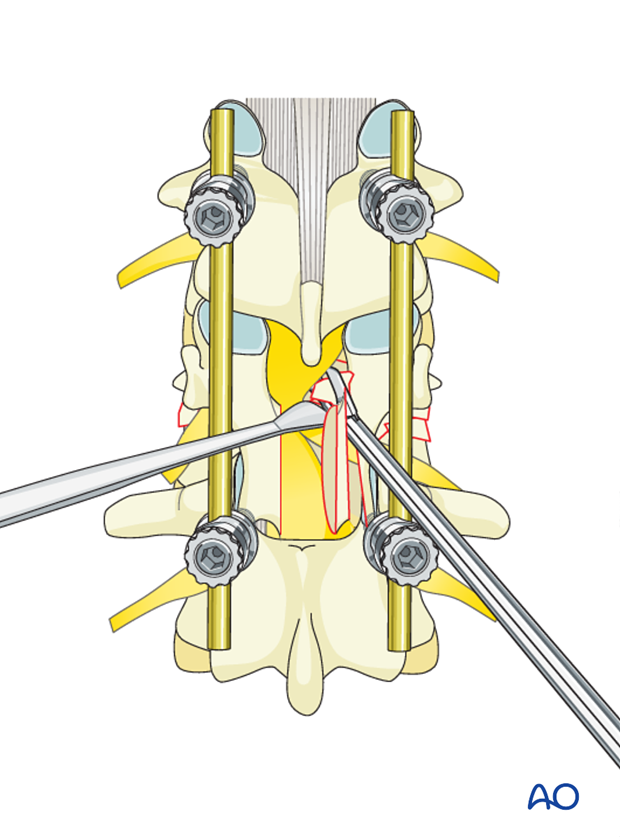
A laminotomy is performed at the area between the pedicles of the fractured vertebra. The adjacent spinous processes and the intervening ligamentum flavum are excised. Portions of the superior and inferior lamina and the medial portion of the facet joint are removed.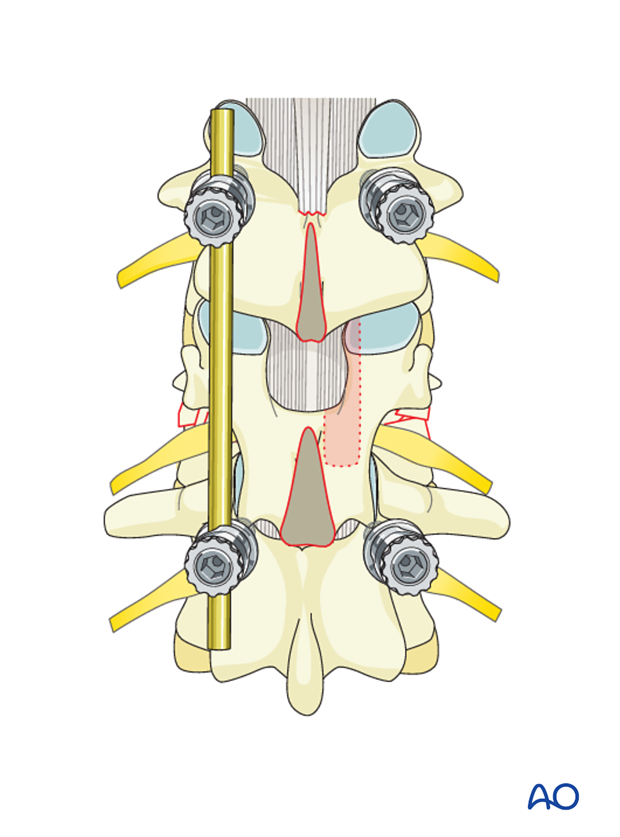
The laminotomy should be extended distally to delineate the pedicle. Once the medial border of the pedicle is identified, a power drill is used to burr the pedicle with care taken to preserve the nerve root exiting below it.
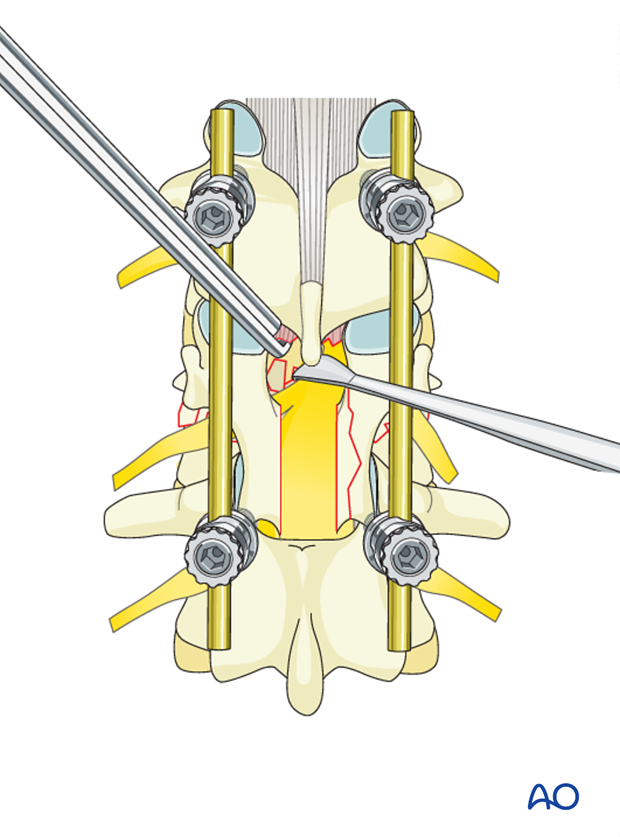
A channel is cut 1 cm into the vertebral body anterior to the medial portion of the pedicle that has been thinned. Reverse-angle curettes can be inserted through this opening, and any bone fragments compressing the anterior neural elements can be impacted into the vertebral body. Removing the bone fragment is a very delicate procedure and only experienced surgeons should perform it.
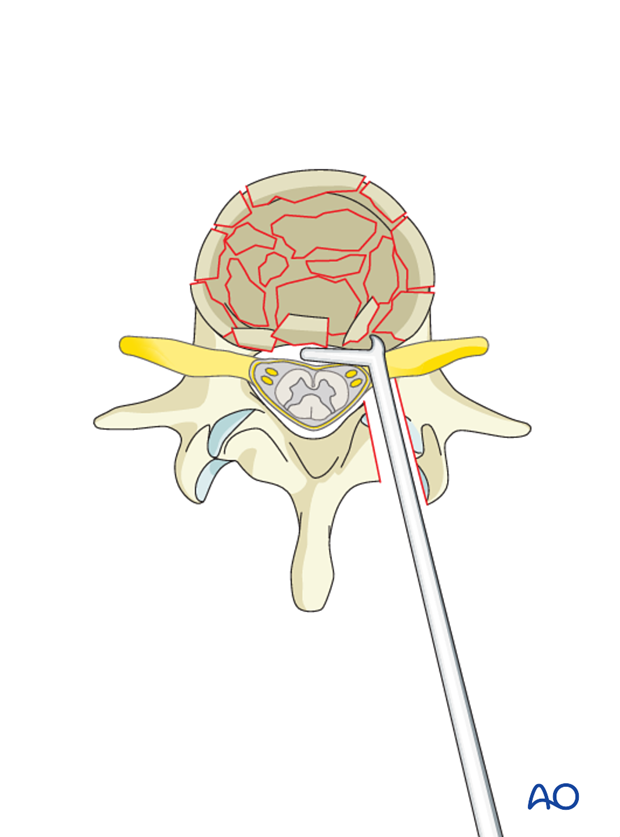
If the decompression is adequate on both sides of the canal, with no further decompression, the instrumentation may be completed. If further decompression is needed, the same technique may be applied on the other side.