Combined anterior and posterior (360)
1. Introduction
In most clinical situations the fracture can be addressed either by the anterior or the posterior approach.
However, in some case both the anterior and the posterior approach will need to be performed.
The use of a 360 approach is reserved for a limited amount of cases. Uncritical use of a 360 approach may unnecessarily increase the risk of complications.
Anterior vs. posterior vs. 360
The anterior surgery provides direct access to release pressure and to reconstruct the anterior column.
A posterior surgery will permit effective direct reduction maneuvers in fracture patterns otherwise difficult to reduce. Furthermore it is also the best way to restore the posterior tension band.
The 360 approach is indicated for a selected group of patients requiring the advantages of both anterior and posterior surgery.
General guidelines
Usually the anterior approach is performed first to clear the canal.
With the patient placed supine, one of the two following approaches may be used depending on the exposure needed:
If an MRI rule out the presence of a disk herniation, and a complex facet fracture dislocation predict a difficult reduction the posterior surgery should be performed first.
With the patient placed prone, one of the two following approaches may be used depending on the exposure needed:
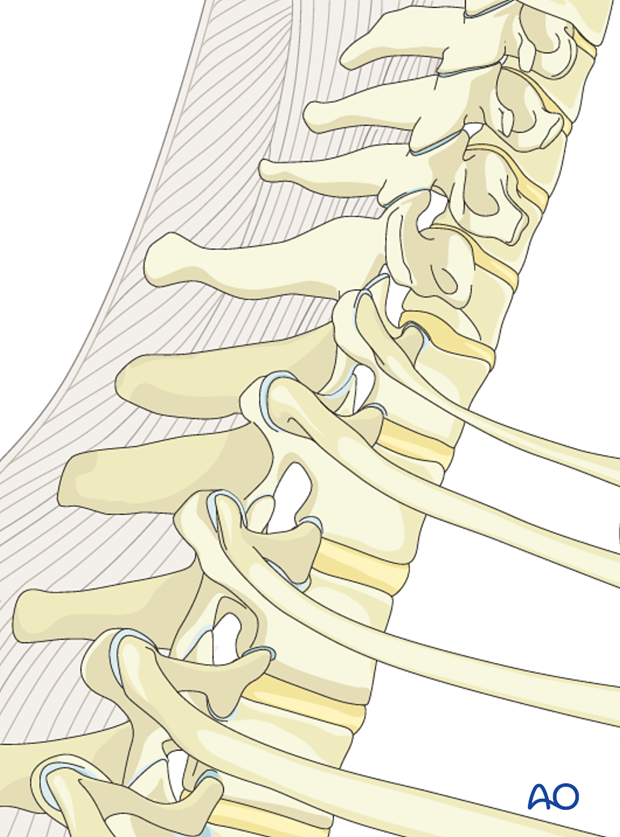
Fractures of the cervicothoracic junction
The cervico thoracic junction has a specific biomechanical behaviour. This is due to the sudden change from the extremely flexible cervical spine, to the more rigid thoracic spine.
The thoracic spine has a shorter elastic zone due to:
- The rigid rib cage
- The coronal orientation of the facet joints
- The overlapping of the spinous processes.
Surgical complications
More details on surgical complications can be found here.
2. Case
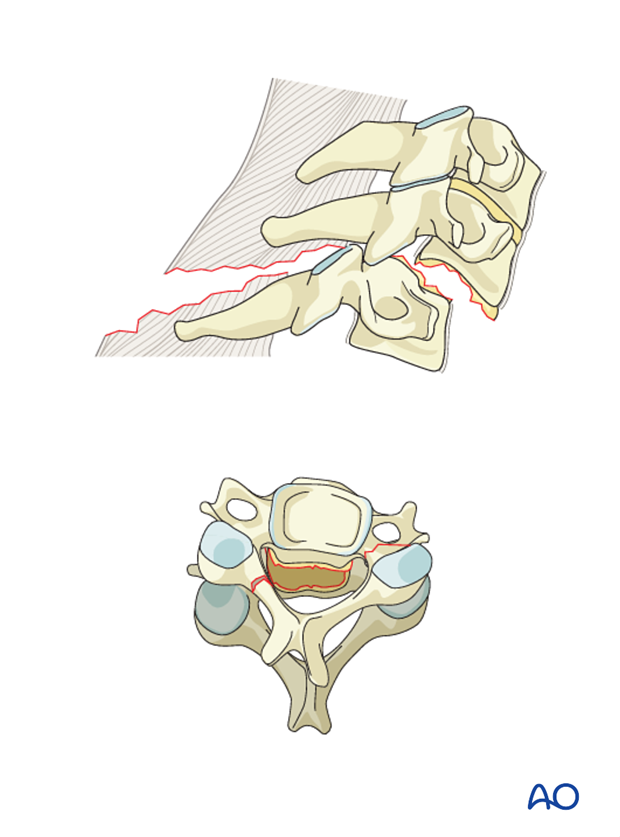
To illustrate the use of a 360 lesion will use the following case which is a type C injury.
- There is a complete rupture of both anterior and posterior longitudinal ligaments.
- The disk is torn with an apparent disk herniation behind the body of C6.
- In the posterior column there is a fracture dislocation on the right side and a pedicle fracture on the left side.
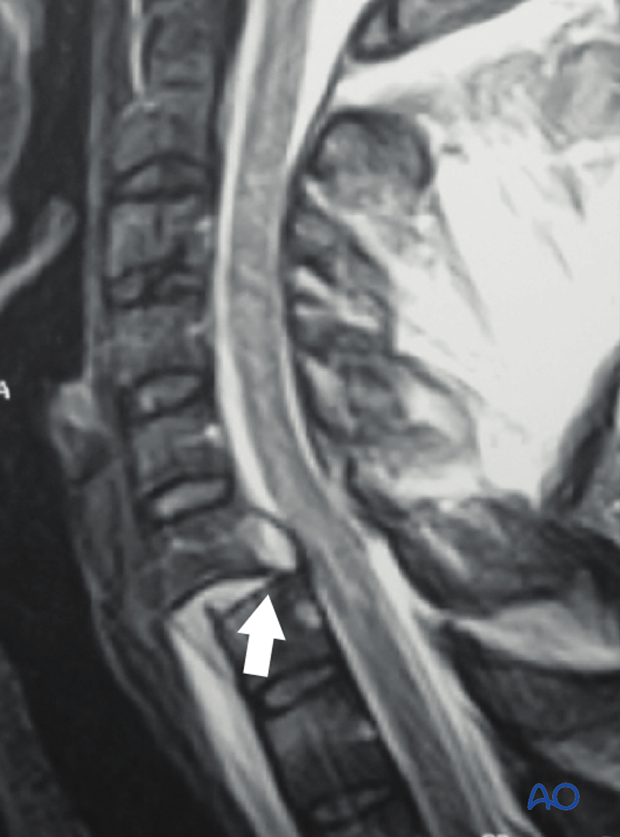
- The posterior tension band is also completely torn as seen on MRI (below).
These injuries result in a severe instability that cannot be controlled by anterior or posterior surgery alone.
Separation of the two columns will require both anterior and posterior instrumentation.
Imaging
Lateral X-ray from a 42 years old male, 24 hours after a car accident. C7 right motor deficit (4/5) is the only neurological finding. Patient is cleared from other lesions.
C6-C7 subluxation with complete disk disruption is clearly seen. A complex fracture type on the posterior column will be better identified on CT.

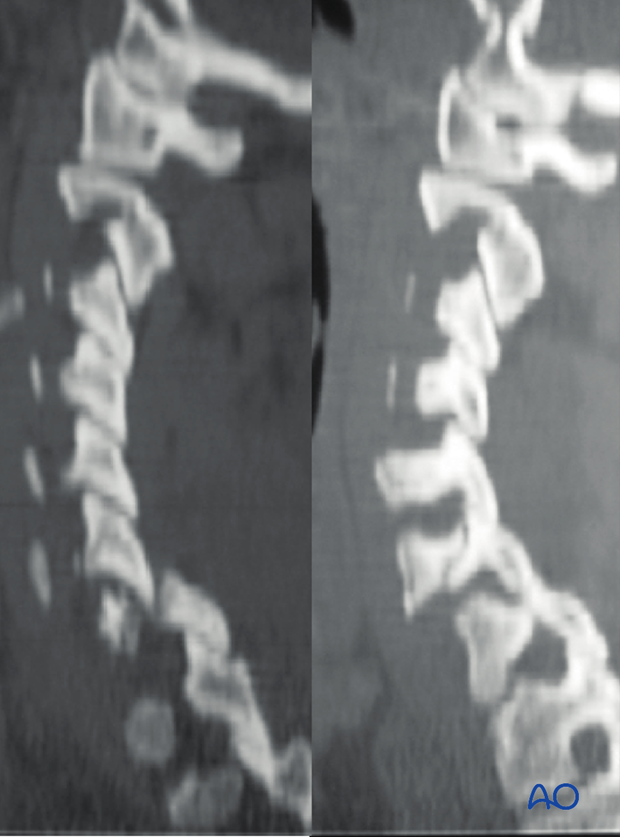
Axial views of C6 clearly show a fracture dislocation on the right and a pedicle fracture on the left. This results in a separation between the two columns and an increase in the AP canal diameter.
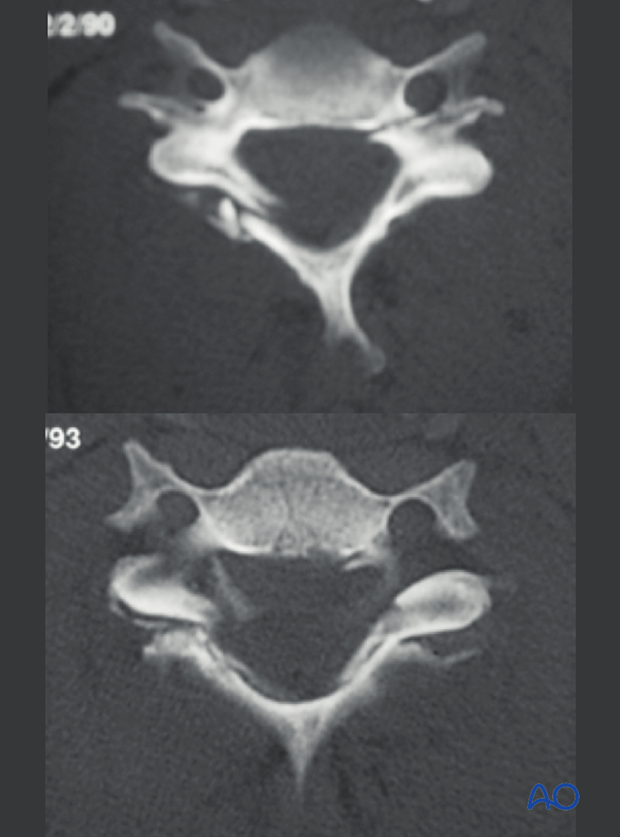
Sagittal reconstructions illustrate the fracture dislocation on the right and the pedicle fracture on the left.
MRI shows the severe soft tissue damage. All ligaments are thorn or stripped and the disrupted disk (arrow) is partially entering the spinal canal.
3. Rationale of treatment
Both columns need to be addressed.
The anterior approach will allow disk removal and enhance anterior fusion.
However, anterior instrumentation alone will not control translation instability due to the separation between the two columns.
The posterior approach will allow to directly decompress the right C7 root and implementation of an adequate posterior instrumentation.
The anterior surgery was performed first for disk removal, reduction, and anterior instrumentation with fusion.
During intraoperative fluoroscopy residual instability was observed (as expected). Finally during the same surgical setting, a posterior approach for C7 root decompression and instrumentation was completed.
7 months postoperative, a solid fusion across C6 and C7 is clearly seen to the left.

4. Aftercare
Patients are made to sit up in bed on the first day after surgery.
A collar is commonly used following surgical stabilization to moderate patient activity.
The purpose of a collar is to prevent ranges of motion outside of limits deemed unfavorable for fracture healing. Collar is optional.
Patients with intact neurological status are made to stand and walk on the second day after surgery. Patients can be discharged when medically stable or sent to a rehabilitation center if further care is necessary. This depends on the comfort levels and presence of other associated injuries.
Patients are generally followed with periodical x-rays at 6 weeks, 3 months, 6 months, and 1 year.