Posterior access to the thoraco cervical junction
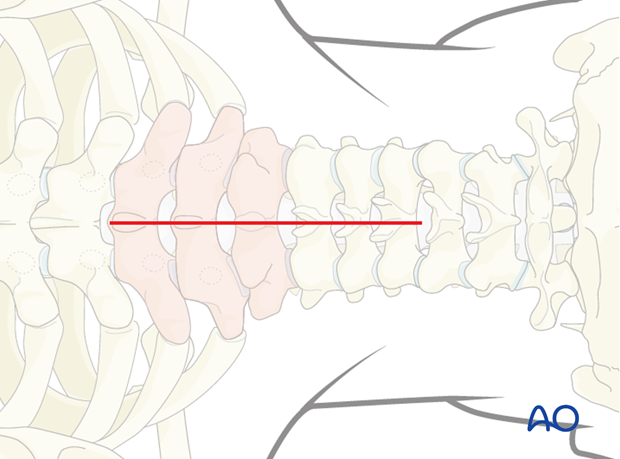
1. Skin incision
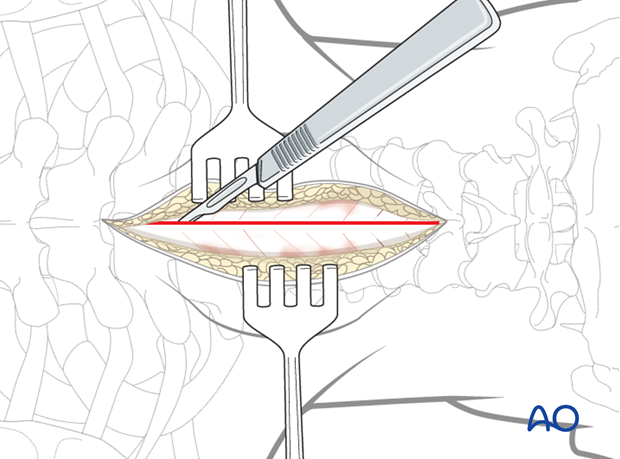
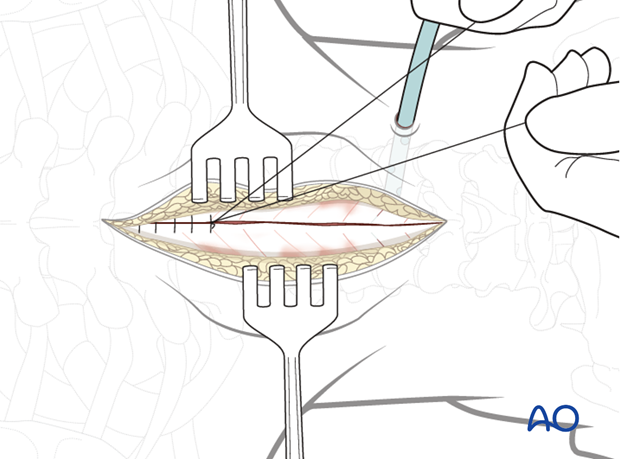
The skin and subcutaneous tissue may be infiltrated with a 1:500,000 epinephrine solution to achieve hemostasis.
The exact location of the incision is identified using a C-arm and marked.
A midline skin incision is made centered over the involved segment.
2. Dissection
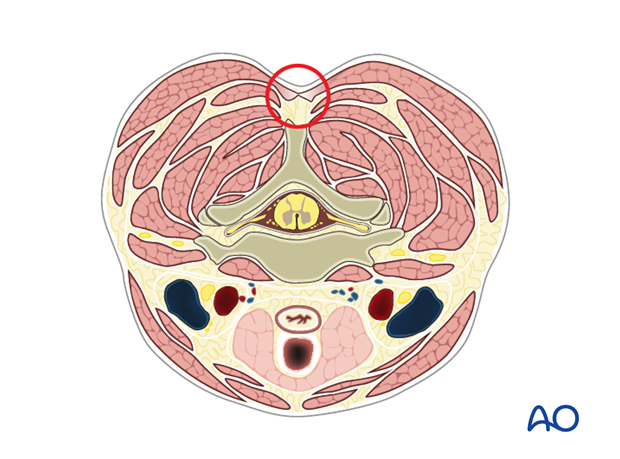
The dissection is carried down in the midline through the subcutaneous tissue and the fascia of the upper back musculature including the trapezius, latissimus dorsi, rhomboids, and paraspinous muscles to the tips of the spinous processes.
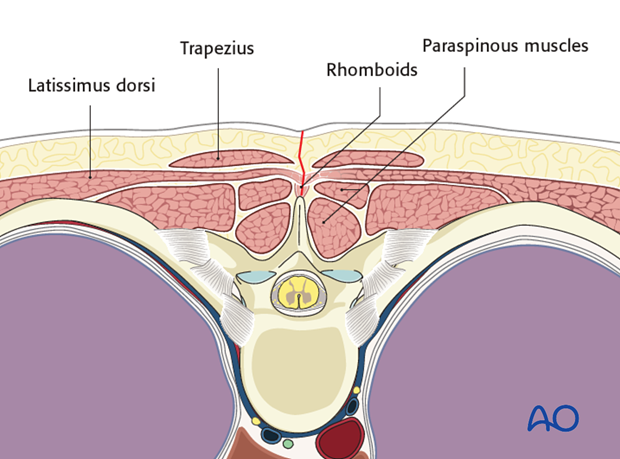
The dissection should be carried down through the midline to decrease bleeding.
It is necessary to confirm the vertebral level with fluoroscopy as soon as bony structures are visible. This is done prior to any further dissection.
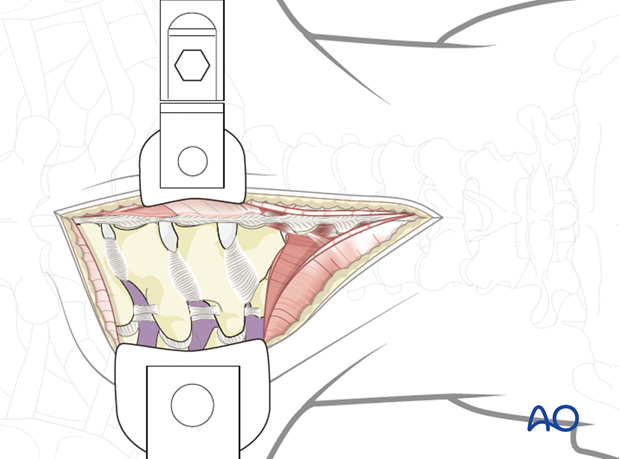
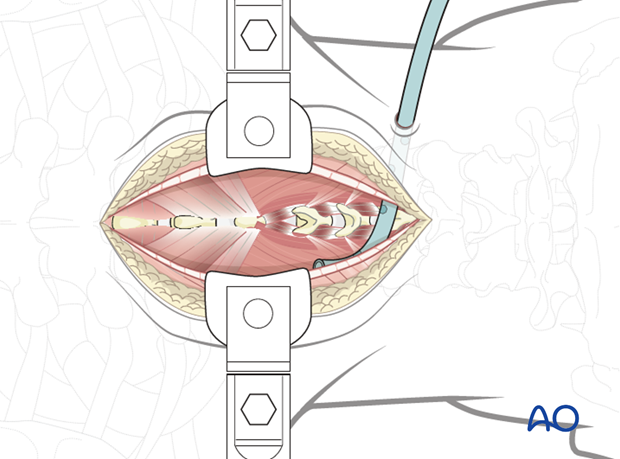
Self-retaining retractors are used to maintain tension on soft tissues during exposure.
The paraspinal muscles are elevated subperiosteally from the underlying laminae, using a Cobb elevator or electrocautery. Dissection is performed along the posterior bony elements bilaterally.
The use of a subperiosteal dissection minimizes bleeding and muscle damage.
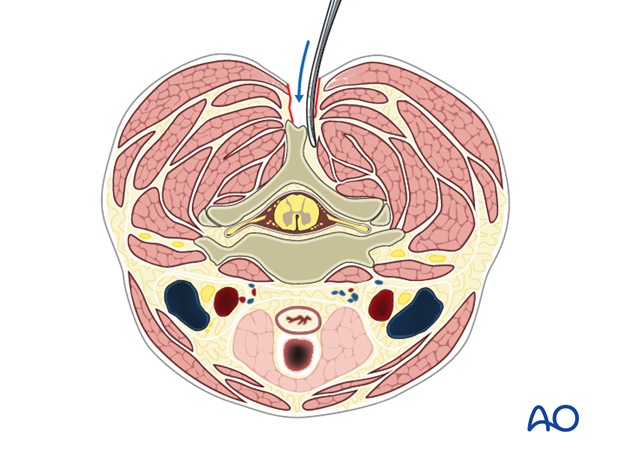
During exposure, care is taken not to injure the facet joint capsule of the levels cranial or caudal to the intended fusion, as this might lead to unintended adjacent level joint fusion or degeneration.
Access to the anterior column can be achieved through a posteriolateral approach. The two options are the posterolateral and far lateral costotransversectomy approaches.
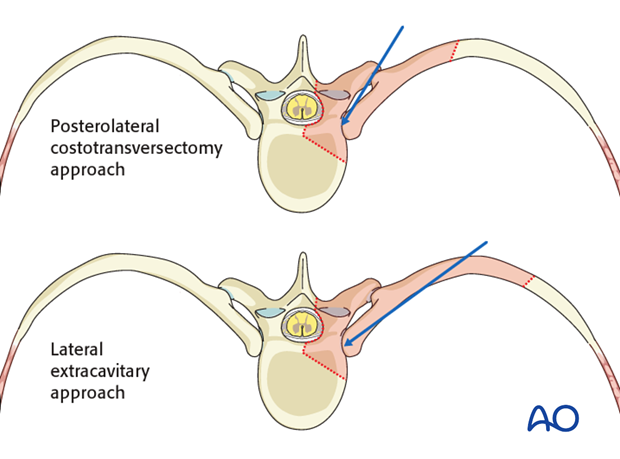
3. Posterolateral costotransversectomy approach
Dissection is carried subperiosteally along the posterior aspect of the ribs corresponding to the anterior vertebral level(s) requiring exposure.
Exposing one rib above and below may decrease soft tissue tension and improve exposure.
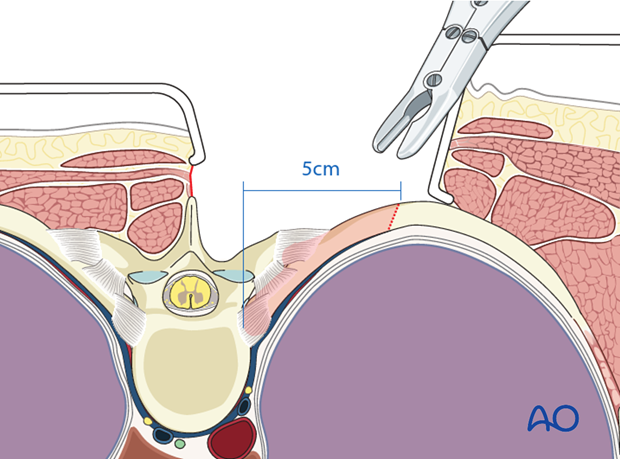
The posterior 5 cm of the rib are exposed subperiosteally in a circumferential manner with a Cobb elevator.
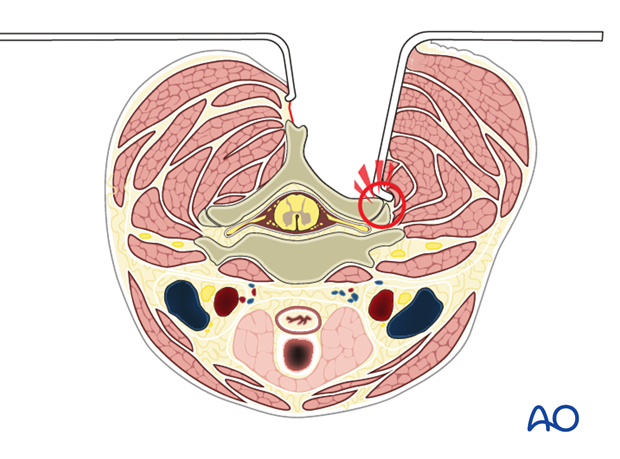
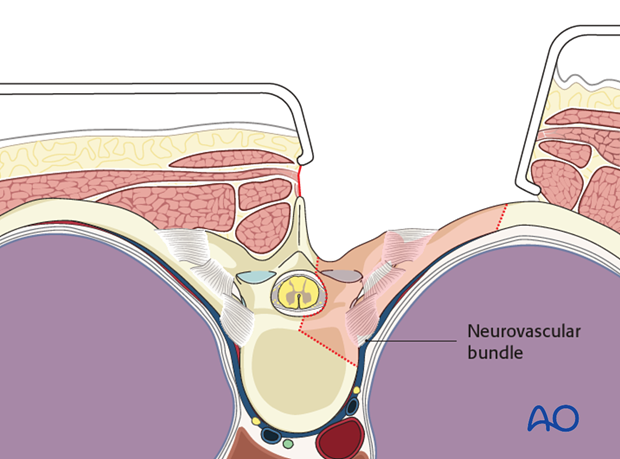
Subperiosteal exposure is essential to avoid injury the underlying pleura and the neurovascular bundle. The neurovascular bundle lies against the anterior inferior aspect of the rib and should be protected.
A bone cutter is used to osteotomize the rib approximately 5cm from the costovertebral joint.
The free rib section is then grasped and gradually released from its surrounding soft tissue tethers including the various costovertebral joint capsule and ligaments.
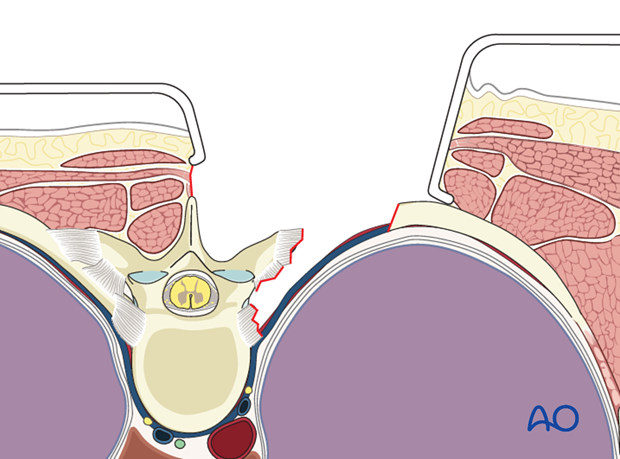
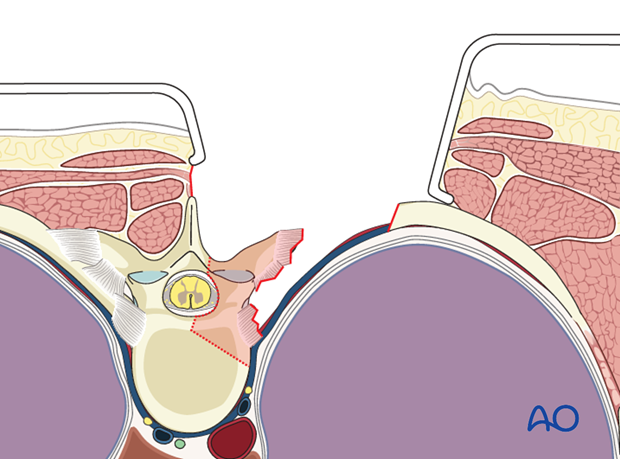
The lateral vertebral body and anulus are exposed subperiosteally. Subperiosteal exposure is essential to minimize blood loss and to avoid injury to the great vessels which lie in close proximity to the anterolateral border of the spine.
A malleable retractor is used to retract soft tissues anterior and lateral to the anterior column of the spine.
4. Lateral extra-cavitary approach
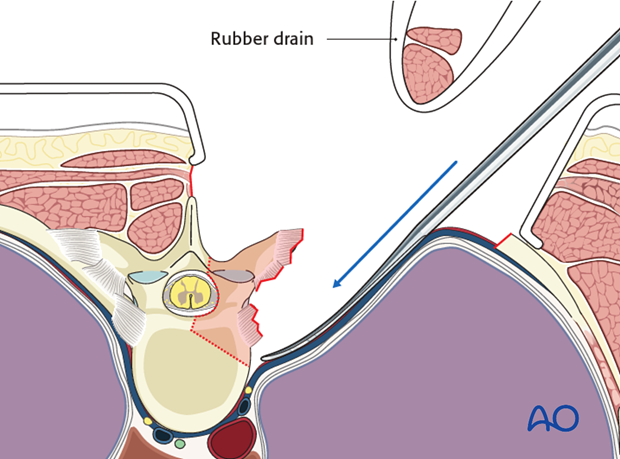
The primary difference in the lateral extra-cavitary approach is the use of a plane of dissection lateral rather than medial to the paraspinal muscles. This more lateral plane of dissection allows a more transverse angle of approach to the spinal canal and the anterior spinal column. It requires approximately 8-10 cm of posterior rib resection. After the paraspinal muscle mass is dissected from the midline, it is released along its lateral border and the entire muscle mass can be mobilized medially and laterally as needed with a Penrose drain.
5. Closure
Drains are usually inserted via a separate stab incision.
Once the surgical fixation and decompression have been performed, the muscles are approximated over a deep suction drain using interrupted sutures.
The fascial layer is then closed with continuous or interrupted sutures.
At the time of writing this text, there are several articles showing that the use of vancomycin powder prior to closure may decrease infection rate.
The approximation of the posterior cervicothoracic muscles is subject to considerable tension and fascial dehiscence. The use of nonabsorbable sutures for fascial closure should be considered.
Note: If the fascia is closed without a previous muscle approximation, a dead space may be created. This should be avoided.
The subcutaneous layers and skin are sutured.
A postoperative upright chest X-ray should be obtained to evaluate for possible pneumothorax.














