Revision of a hybrid glenoid component
1. Introduction
Periprosthetic glenoid fractures in cases of hybrid components occur due to polyethylene wear leading to loosening of the peg, loss of substance of the glenoid, and then finally fatigue fractures.
Traumatic periprosthetic glenoid fractures around hybrid components are very rare. More detail about the treatment of glenoid fractures is provided in the AO Surgery Reference Adult trauma Scapula module.
Preoperative planning
An early sign of hybrid component associated problems is joint space narrowing on x-rays due to polyethylene wear. The amount of glenoid bone loss is of tremendous importance to the revision strategy.
Modern revision planning software makes it possible to quantify the glenoid defect.
Preoperative CT planning is mandatory when deciding on a strategy of metallic (including augmented designs) or bony reconstruction.
Rotator cuff integrity should be carefully evaluated preoperatively.
In addition, low-grade infection influences the decision-making process on whether a revision can be a one-stage or a two-stage procedure.
These principles are applicable for stemless, short, and standard stems.
Further details about prosthesis design can be found here.
The stemless configuration is shown in this description.
2. Preparation
The standard patient position is the beach chair position with inclination of about 30°. An arm holder may be helpful but is not essential.
Intraoperative fluoroscopy can be helpful.
Patient positioning should be discussed with the anesthetist.

Bone graft
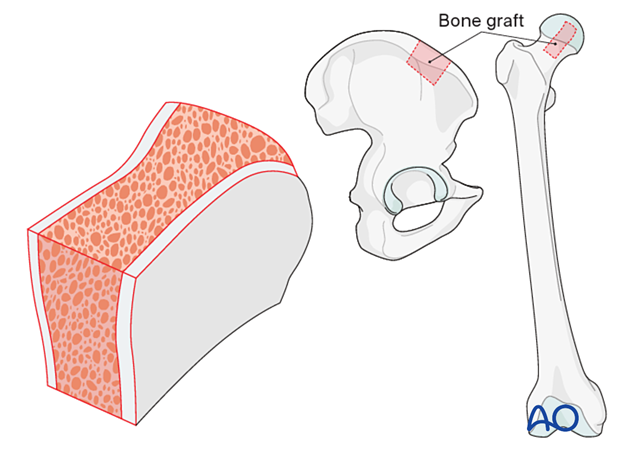
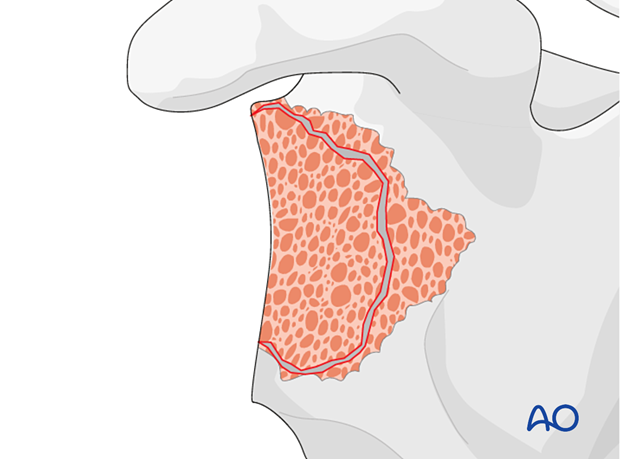
If augmentation or reinforcement of the glenoid fracture or defect is required, bone allograft may be utilized. Structural bulk allograft or morselized allograft are indicated for specific conditions of the glenoid.
If allograft is not available be prepared to take cortico-cancellous or cancellous graft from the iliac crest (autograft) as shown.
The procedure is done under perioperative antibiotics.
3. Approach
The standard approach used is the deltopectoral approach, which can easily be extended proximally and distally.
Previous incisions should be used if this approach was performed correctly during the primary operation. Do not hesitate to perform a new skin incision if the approach used in the primary was inaccurate.
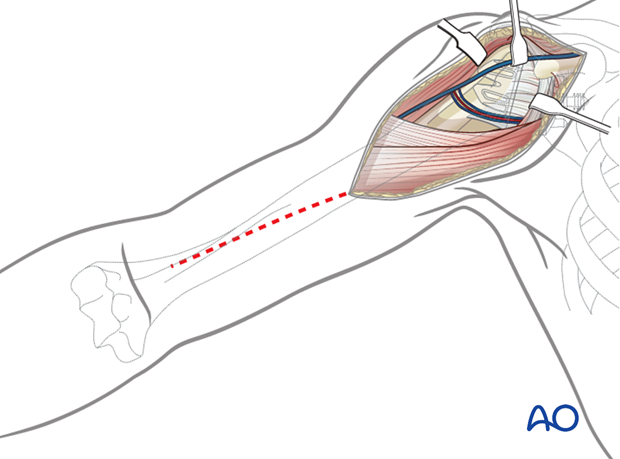
Soft-tissue management
Be prepared for extensive soft-tissue release and a more difficult subscapularis takedown technique before executing the arthrolysis needed to access the glenoid. Take biopsies for cultures.
4. Revision to an anatomic implant
Revision of an anatomic implant to another anatomic implant is very rare in cases of fatigue glenoid fractures with substantial loss of bone substance. In these cases, an intact rotator cuff, in particular the subscapularis, is mandatory for a successful outcome.
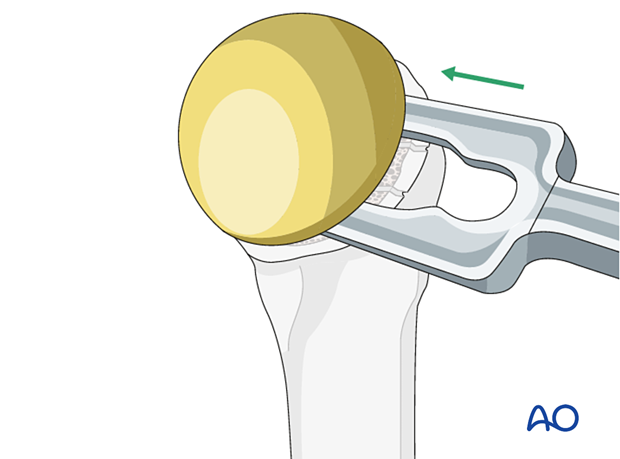
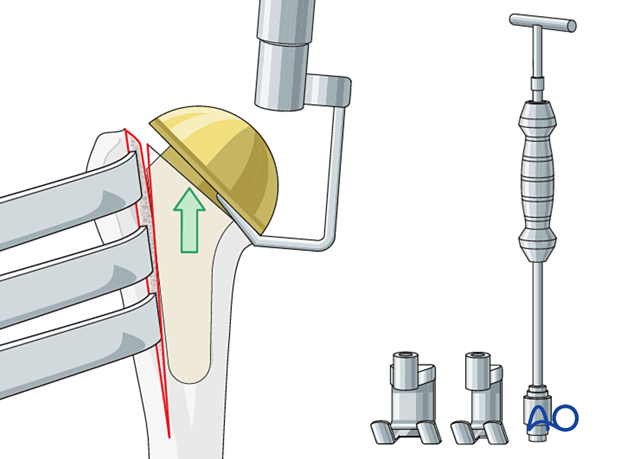
Humeral head removal
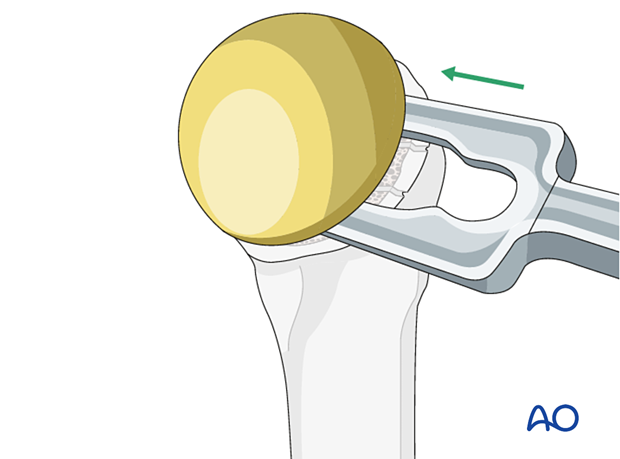
Access and exposure of the glenoid is facilitated by humeral head removal. Remove the humeral head using standard instruments for the specific implant.
Glenoid exposure and exchange
After exposing the glenoid, remove the polyethylene component from the central peg, with an osteotome. If necessary, use a Trephine reamer to remove the peg. Reimplanting an anatomic glenoid component depends on the remaining glenoid bone stock. Augmentation of fixation with bone graft and/or cement may be required.
After placement of the glenoid component, a new humeral head component is inserted.
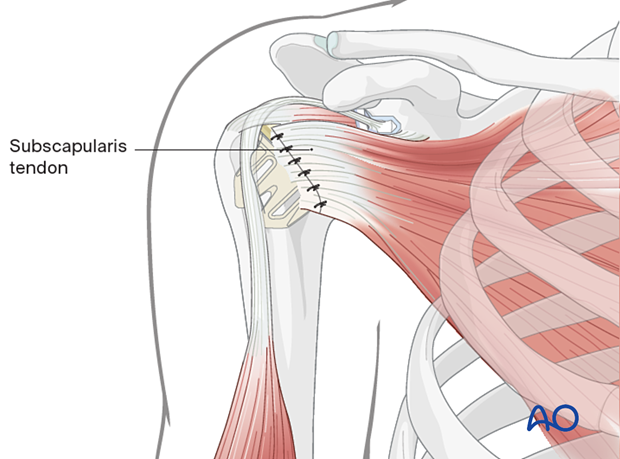
The humerus is reduced, and the subscapularis tendon is reattached.
5. Revision to a reverse arthroplasty
The decision to carry out a revision to a reverse arthroplasty is based on a number of factors including:
- Status of the rotator cuff
- Shoulder function
- Patient age
Soft-tissue management
Be prepared for extensive soft-tissue release and a more difficult subscapularis takedown technique before executing the arthrolysis needed to access the glenoid. Take biopsies for cultures.
Humeral head removal during revision
Access and exposure of the glenoid is facilitated by humeral head removal. Remove the humeral head using standard instruments for the specific implant.
Convertible humeral stems
In this scenario the stem can be retained. The articular component is converted to a reverse after the glenoid is reconstructed.
Non-convertible humeral stems
In this scenario the stem must be removed.
Remove the humeral stem with the specific revision instruments for the arthroplasty.
Humeral component removal during revision
Depending on the humeral component design, different strategies for implant extraction are available. More information on implant extraction is provided here.
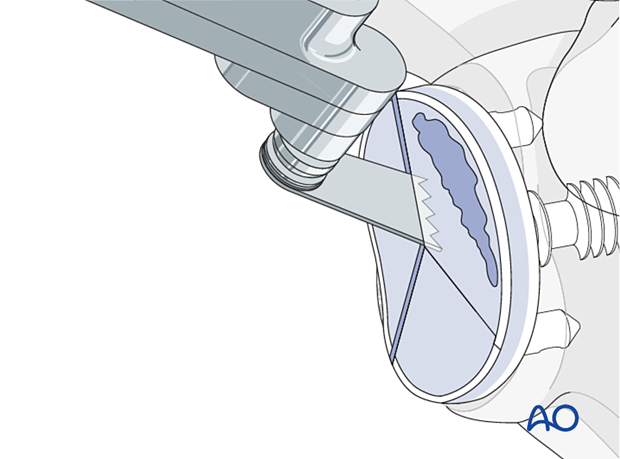
Glenoid exposure and revision of the hybrid component to reverse
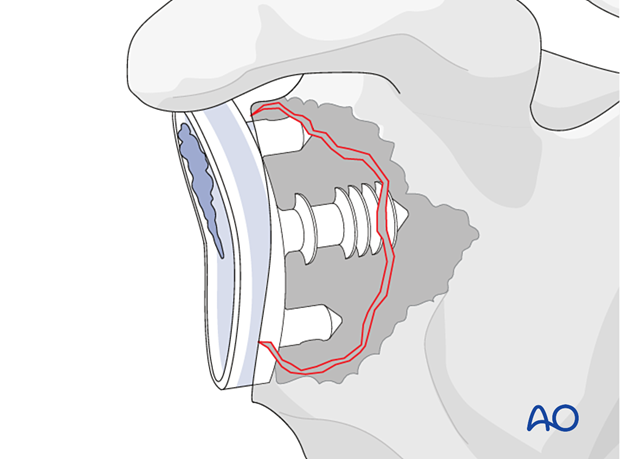
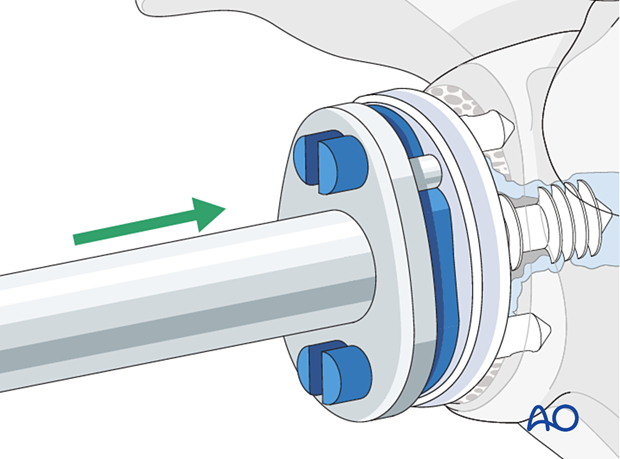
After exposing the glenoid, remove the polyethylene component.
If the central peg is well-fixed and needs removal, then remove with an osteotome and a Trephine reamer.
If the component is loose and/or broken, remove the component and debride the remaining scapula bone and evaluate the glenoid defect.
Management of the glenoid bone loss is closely related to the configuration of the remaining glenoid vault.
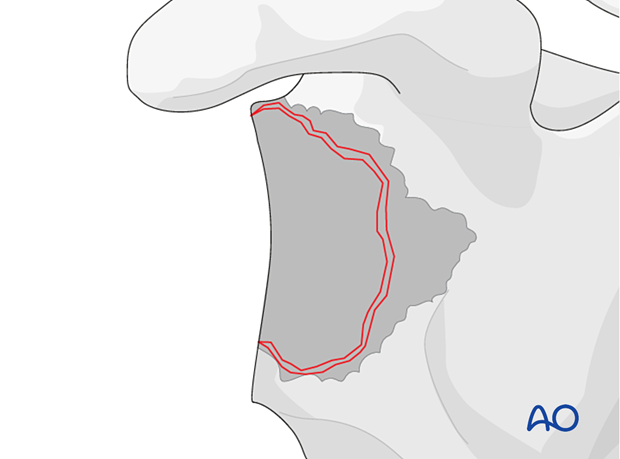
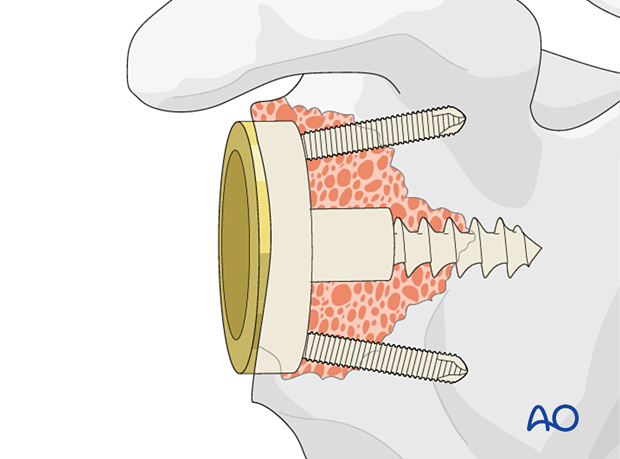
To facilitate stable fixation of a reverse baseplate, it may be necessary to reconstruct the glenoid vault using bone graft.
Glenoid reconstruction
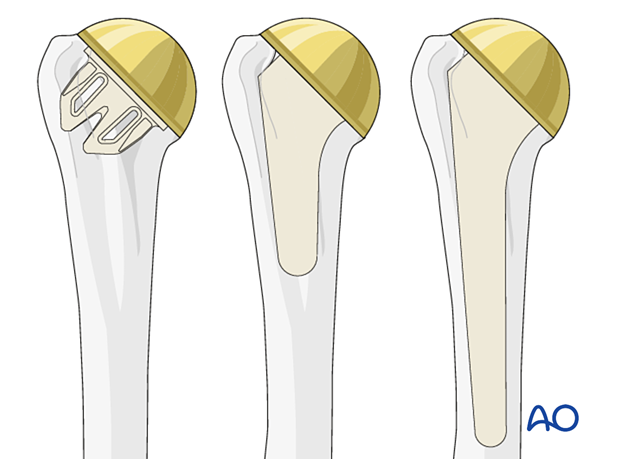
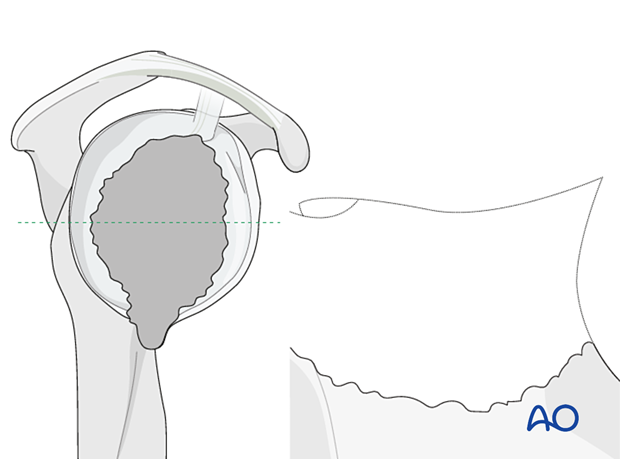
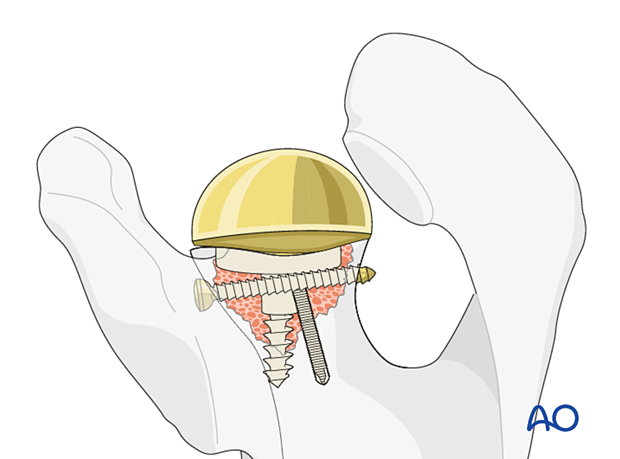
Using bone – contained defectsIn cases of mild glenoid contained defects (Type 1 according to Gohlke) impaction bone grafting is performed and a reverse base plate is implanted.
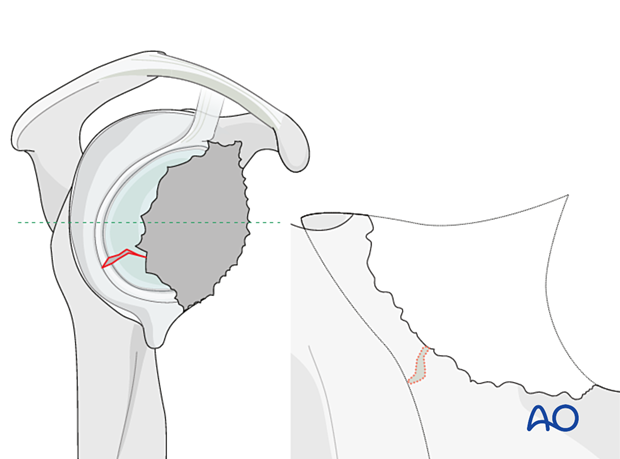
The illustration on the left is a representative cross section of the glenoid vault shown in the right diagram.
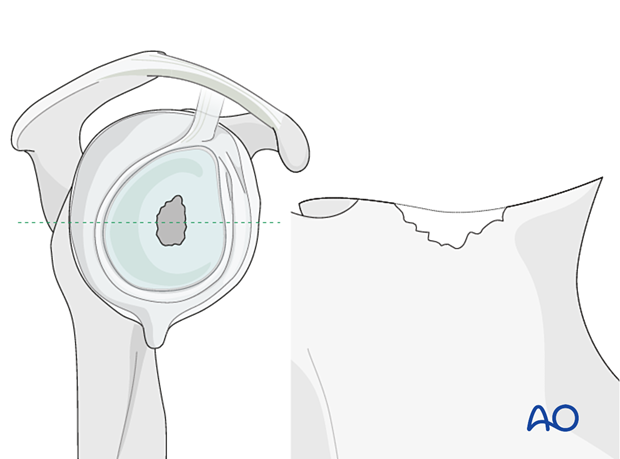
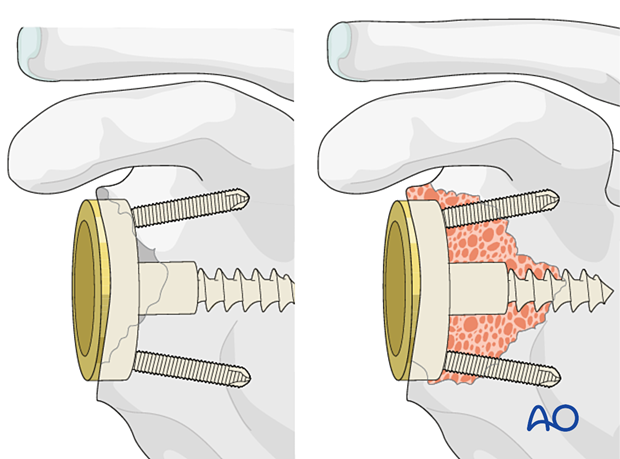
In cases of large, contained defects (Type 2) a structural allograft or autograft is impacted followed by implantation of the base plate.
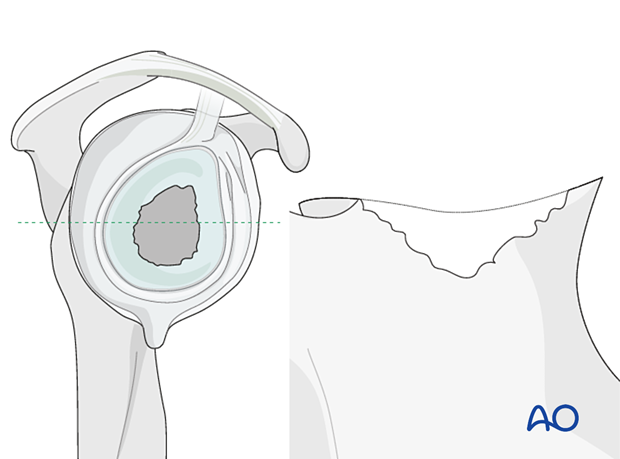
In non-contained defects with either anterior or posterior wall insufficiency (Type 3) a structural allograft or autograft is used and fixed with two or three screws.
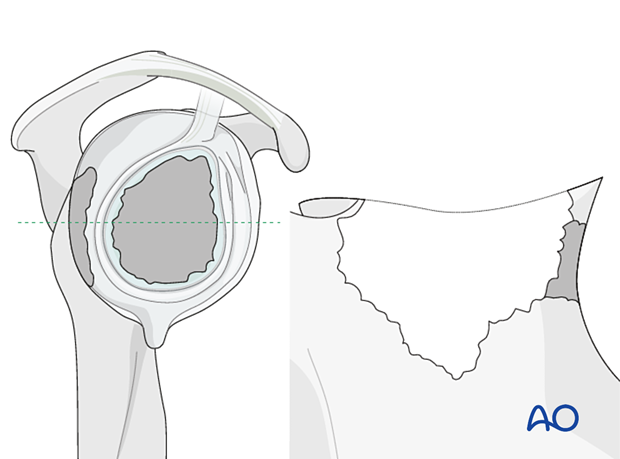
In non-contained defects with severe medialization (Type 4) the same technique is applied.
The decision to perform a one versus two-stage base plate implantation depends on several factors:
- Initial size of the defect
- Primary stability of graft fixation
- Specific implant features
- Surgical experience
In all cases it is important to gain primary fixation in native bone. A reverse baseplate is shown with a central screw fixed into native bone with peripheral anti-rotation screws.
In Type 5 defects with loss of the glenoid vault bony reconstruction should always be performed as a two-stage operation.
Custom implants are often required.
Off-the-shelf augmented base plates may be used in isolation or with bony reconstruction to achieve optimized fixation to the scapula.
Customized implants are not uniformly available and evidence for their role remains to be established.
Advantages include:
- Single-stage procedure
- Personalized to the patient and structural defect
- Optimized function
- Durability
- Time zero structural support
- No risk of graft reabsorption
Disadvantages include
- Lack of availability
- Cost
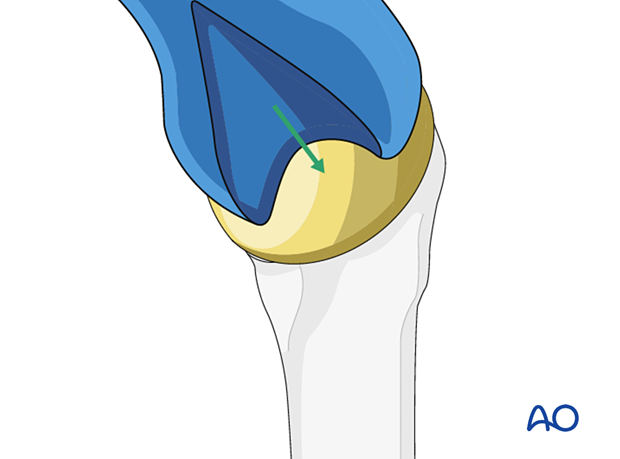
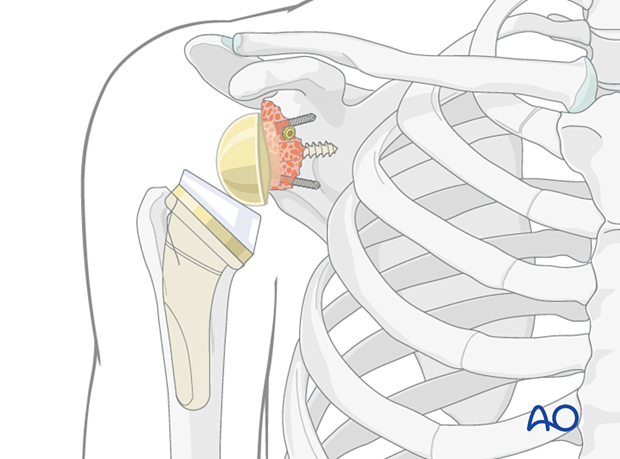
A glenosphere is impacted on the baseplate.
In cases where a convertible stem has been used, the metaphyseal component including the polyethylene liner is impacted. In cases where the stem has had to be removed a new stem is implanted. The shoulder is then reduced.
6. Aftercare
Postoperative phases
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.













