Shoulder implant configurations
1. General fixation considerations
The options for treatment of periprosthetic fractures of the humerus associated with a shoulder replacement depend on the method of fixation of the replacement.
Management of periprosthetic fractures associated with implants with short-segment fixation follows the same principles as fractures of the humerus without shoulder replacement.
Management of periprosthetic fractures associated with diaphyseal fixation depends on the following:
- Fracture configuration
- Whether the implant is loose or not
- Quality of bone around the implant
- Available bone distal to the tip of the implant
The management of periprosthetic fractures of the glenoid are dictated by the following:
- Fixation method of the glenoid implant
- Whether the implant is loose or not
- Quality and volume of bone available for fixation

2. Humeral component
Anatomic configuration
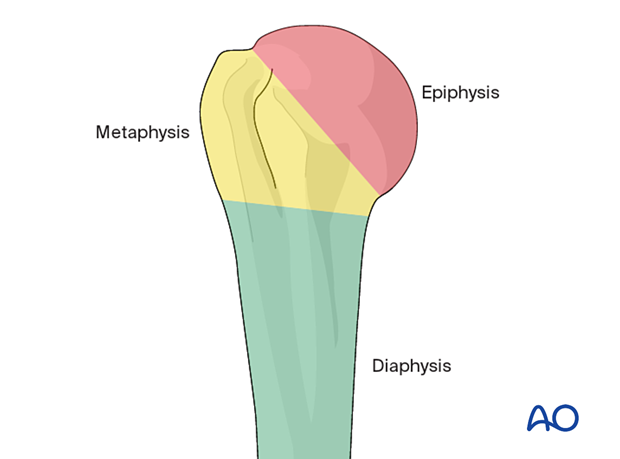
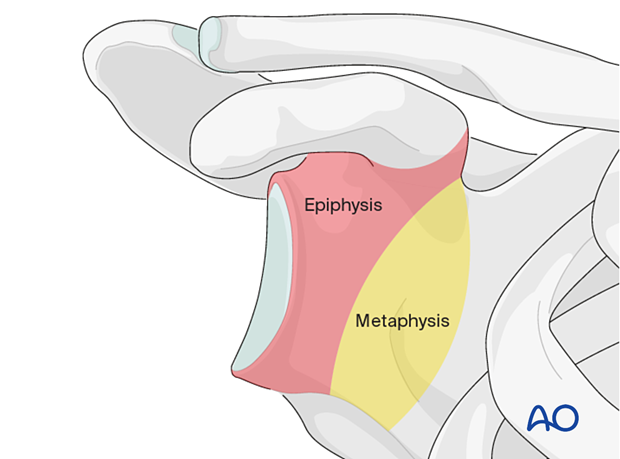
IntroductionThe principle underlying humeral articular replacement is minimal excision of the articular segment (epiphysis) with sufficient fixation for prosthetic mechanical stability.
If the epiphyseal bone quality is considered sufficient, fixation in the epiphysis with a resurfacing replacement is preferred.
If the epiphyseal bone quality is not considered sufficient, fixation in the metaphysis or diaphysis is necessary.
Metaphyseal fixation in sufficient bone quality has been shown to be reliable and is now preferred over diaphyseal fixation.
Diaphyseal fixation is determined by cortical and endosteal bone quality. In good-quality bone, uncemented fixation has been shown to be reliable. In poor-quality bone, cemented fixation remains the preferred option.
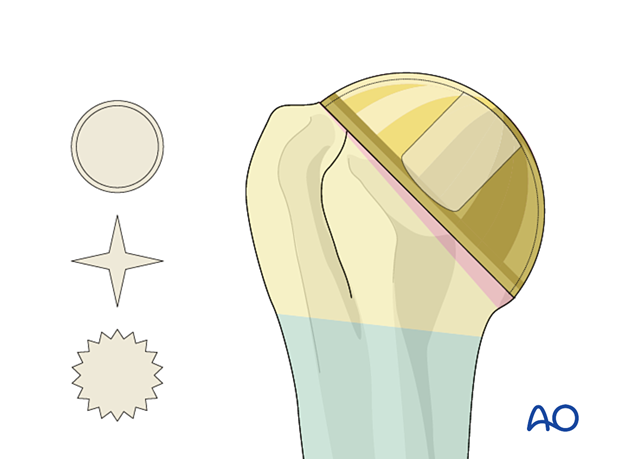
Resurfacing a humeral articular replacement aims to replicate humeral articular geometry. Fixation relies on good quality subchondral bone and peripheral (rim) load-bearing.
Various forms of epiphyseal fixation have been designed: none appear to have a particular advantage.
Advantage:
- The least amount of humeral bone is resected
Disadvantage:
- Access to the glenoid fossa may be restricted
If the humeral articular (epiphyseal) segment is not of sufficient quality to support a resurfacing replacement, then stemless replacement is preferred.
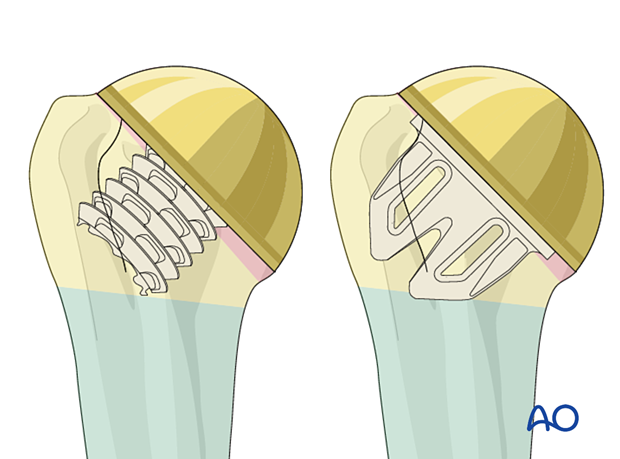
The articular segment is resected and replaced with an anatomic analog of the native humeral head. Fixation is gained in the metaphysis.
Various forms of metaphyseal fixation have been designed: none appear to have a particular advantage.
Advantage:
- Access to the glenoid fossa is improved for glenoid surface prosthetic replacement
Disadvantage:
- Exposure of the shoulder joint by lesser tuberosity osteotomy is not possible
Short stem fixation is preferred for younger patients in whom resurfacing or stemless replacement is not possible due to poor bone quality in the epiphysis or metaphysis.
Fixation can be augmented by cementation if necessary.
Advantage:
- Revision is facilitated by limited diaphyseal fixation
Disadvantage:
- There are no long-term studies of the performance of such prostheses
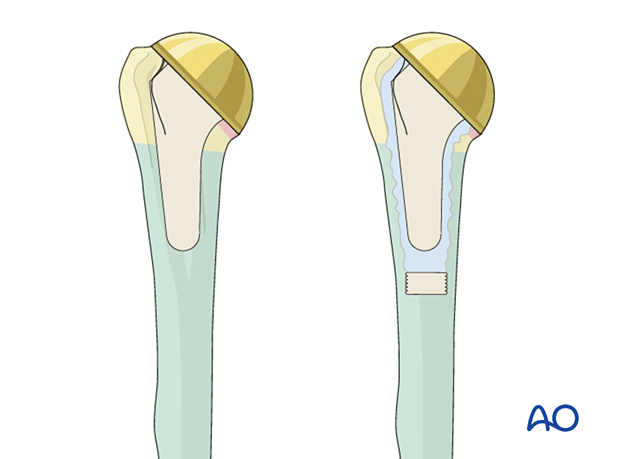
Standard stem humeral replacement is indicated where metaphyseal fixation is considered to be unreliable.
Fixation of the stem may be augmented by cementation.
Advantage:
- Humeral replacement is possible even when proximal (metaphyseal) fixation would be impossible
Disadvantages:
- Revision is complex
- Periprosthetic fracture (diaphyseal) is common during the revision of an uncemented standard stem
- Periprosthetic fracture (metaphyseal) is common during the revision of a cemented standard stem
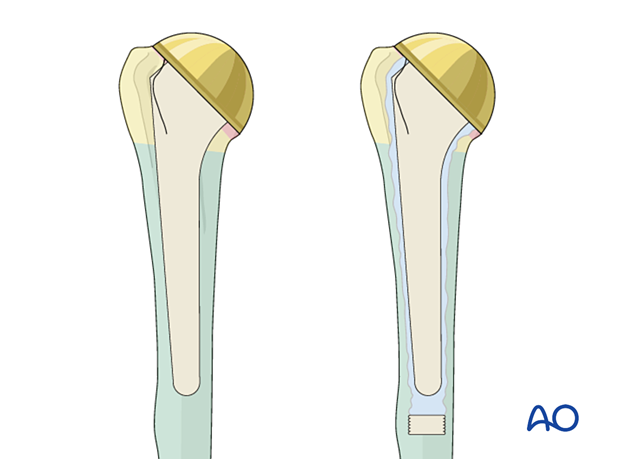
Proximal humeral fractures may be treated with humeral hemiarthroplasty.
A standard stem length is preferred for diaphyseal fixation.
Fixation and healing of associated tuberosity fractures are facilitated by the following:
- Proximal perforation of the stem
- Suture holes
- Additional fins
- Rough surface finish
Reverse (inverse) configuration
IntroductionReverse total shoulder replacement is indicated for the treatment of the following:
- Irreparable rotator cuff tears with arthritis
- Cuff tear arthropathy
- Complex irreparable proximal humeral fractures
- Complex proximal humeral fractures in patients with poor bone quality (ie, the elderly)
The functional outcome of reverse total shoulder replacement depends on the function of the deltoid muscle. If there is a deltoid muscle weakness, other methods of treating these conditions should be considered.
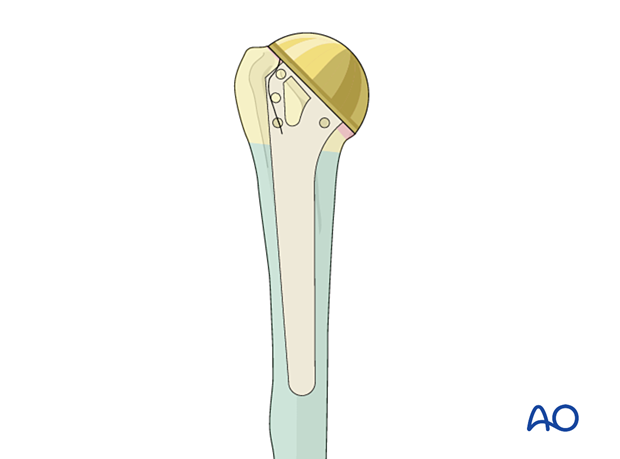
Diaphyseal fixation of a humeral stem is the commonest fixation method in reverse shoulder replacement. Short stem and stemless designs are being evaluated.
Diaphyseal fixation may be augmented by cementation. The indications for the use of cement are the same as for anatomic shoulder replacement.
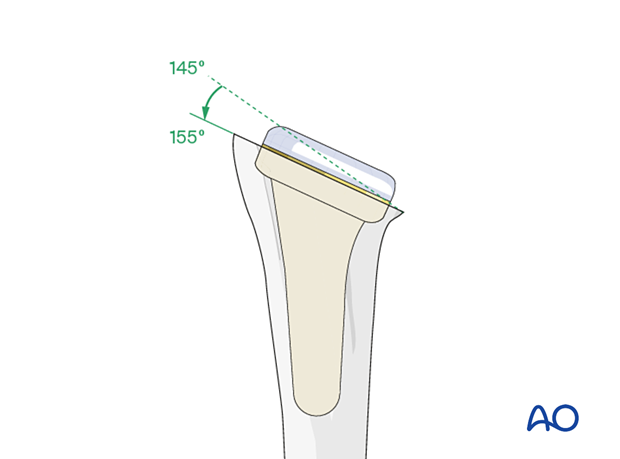
There is debate about the ideal stem-neck angle of resection and the humeral articular bearing surface.
A steep (135°) stem-neck angle creates a more medial and distal center of rotation of the shoulder replacement.
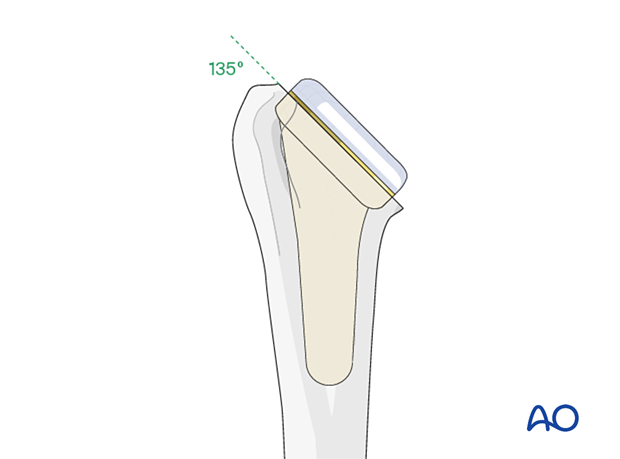
A shallow (155°) stem-neck angle creates a more lateral center of rotation of the shoulder replacement.
Advantages:
- The risk of instability of the reverse shoulder replacement may be reduced
- The effectiveness of external rotation may be increased
3. Glenoid component
Introduction
For a fracture of the proximal humerus treated with humeral hemiarthroplasty, resurfacing the glenoid fossa is not indicated if the surface is intact and healthy.
For an anatomic total shoulder replacement with an intact rotator cuff, resurfacing of the glenoid fossa is preferred for optimal pain relief.
For a reverse total shoulder replacement, use of the glenoid baseplate (metaglene) fixation is determined by the quality of the glenoid fossa and scapular neck bone.
Anatomic configuration
There are two fixation methods. Fixation which relies on a combination of central and peripheral pegs, which may be cemented, is the most common. Fixation using a keeled component depends on cementation into good quality bone in the scapular neck (metaphysis).
The glenoid component commonly has a convex surface that matches the concave prepared surface of the glenoid fossa. Fixation using a variety of pegs secured to the epiphysis of the glenoid with cement is generally preferred over fixation using a fin or keel.
Advantage:
- In cases where revision of the glenoid component is required, the loss of bone stock from the glenoid epiphysis is considered to be less after explantation of a pegged component than after removing a keeled component
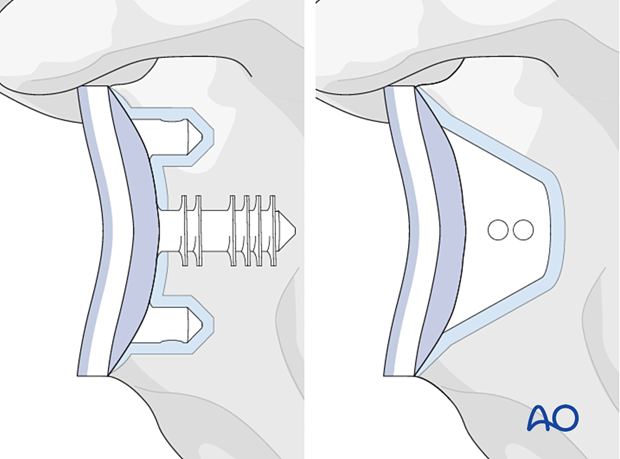
Some glenoid surface replacement components are secured within a metal baseplate secured to the glenoid metaphysis by pegs and/or screws.
Advantages:
- The same baseplate may, in "platform systems", support a glenosphere when a revision to a reverse total shoulder replacement is indicated
- Removal of the baseplate is usually not associated with excessive bone loss
Disadvantages:
- The additional depth of the metal-backed component may add to difficulty with soft-tissue tension and its management
- If the polyethylene insert is relatively thin, earlier polyethylene wear may limit the durability of the replacement
Reverse configuration
Reverse total shoulder replacement is indicated for treatment of the following:
- Irreparable rotator cuff tears with arthritis
- Cuff tear arthropathy
- Complex irreparable proximal humeral fractures
- Complex proximal humeral fractures in patients with poor bone quality (ie, the elderly)
The functional outcome of reverse total shoulder replacement depends on the function of the deltoid muscle. If there is deltoid muscle weakness, other methods of treating these conditions should be considered.
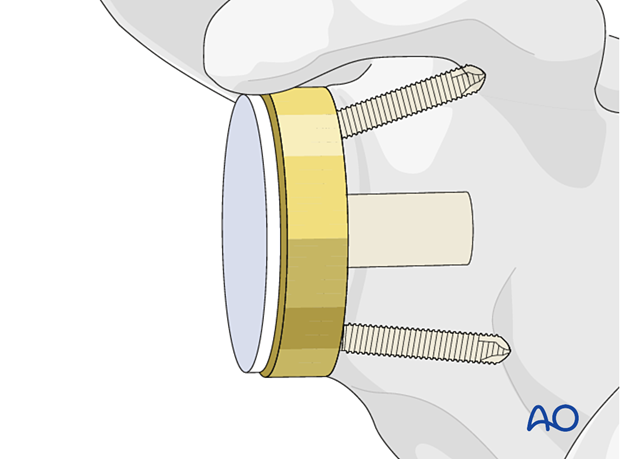
The glenoid component comprises two parts:
- the metaglene or baseplate, which is fixed to the glenoid fossa and scapular neck (metaphysis)
- the glenosphere (the articulating surface)
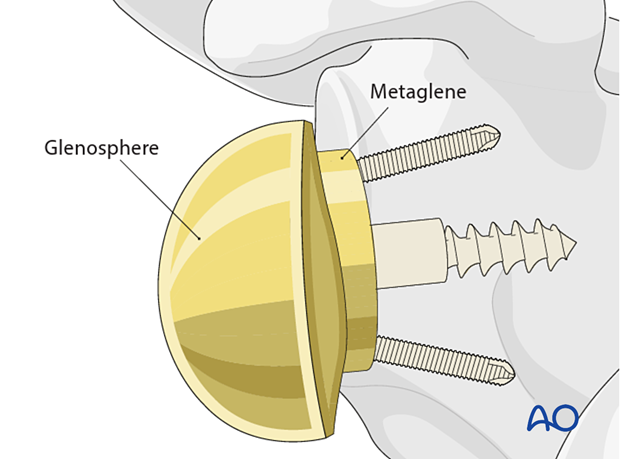
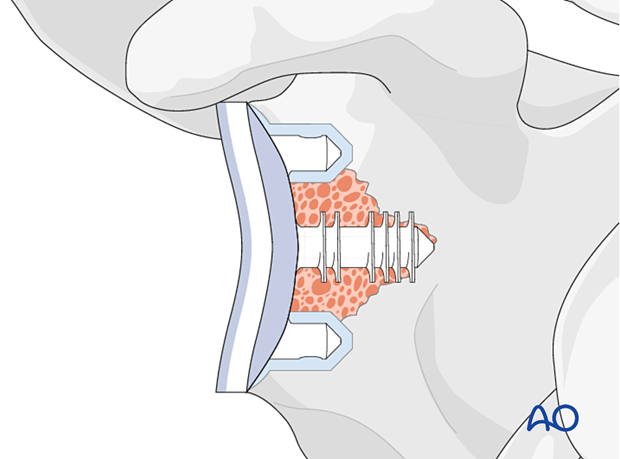
The metaglene has a convex rear surface that matches the prepared surface of the glenoid fossa.
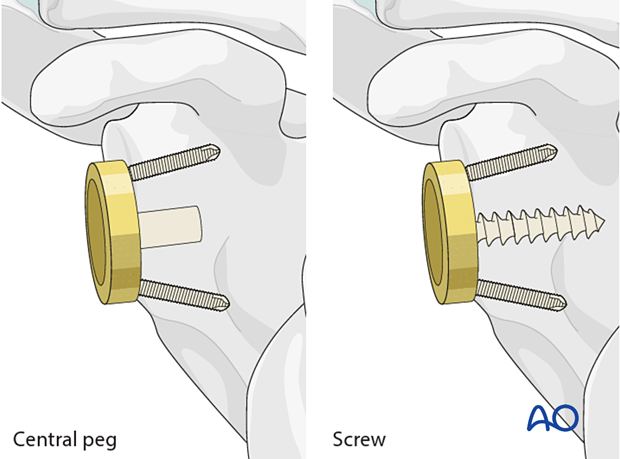
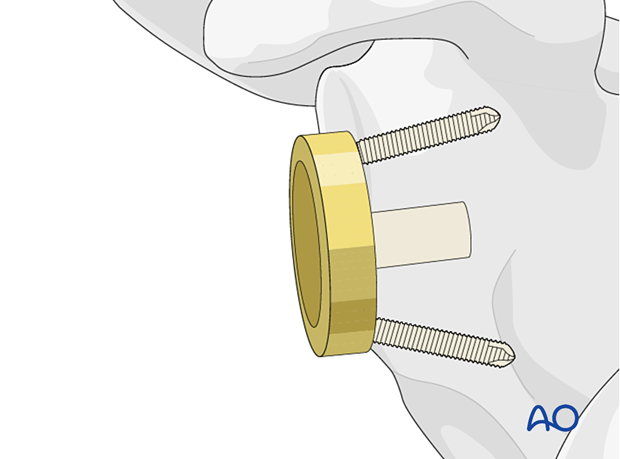
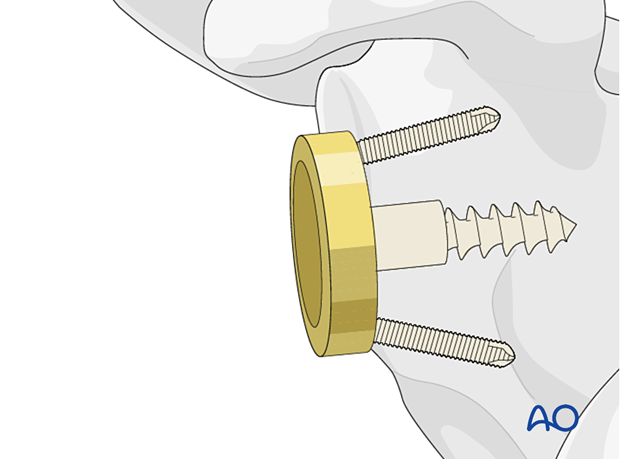
The metaglene is fixed by a central peg or screw. Peripheral screws (either compression or locking screws) are used in combination with the central peg or screw.
Advantage:
- Secure fixation in good quality bone
Disadvantage:
- If loosening occurs, cavitary bone loss may present a problem for revision
Advantage:
- Compression fixation of the metaglene in relatively poor-quality bone
Disadvantage:
- Distal fixation gained in the anterior scapular cortex inferomedial to the coracoid can result in poor loading of the glenoid and, therefore, progressive bone loss
Advantage:
- Ease of revision
Disadvantage:
- Bone loss on explantation