ORIF lag screw
1. Principles
Introduction
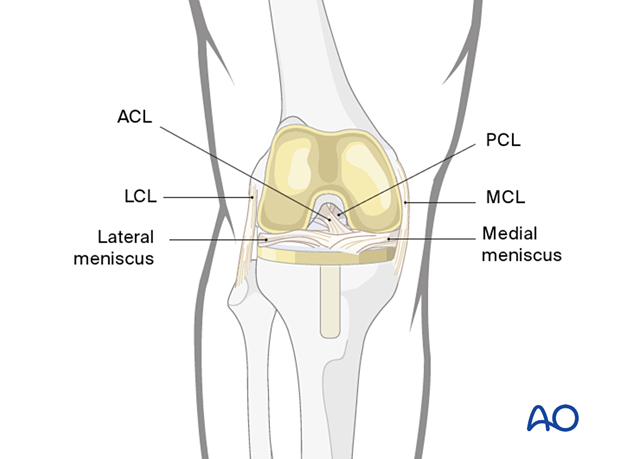
Fixation of ligamentous avulsion fractures is essential to knee joint stability, especially in association with intra-substance ligament injuries. Healing in displacement results in joint stiffness and laxity.
Consultation and advice from specialist knee reconstructive surgeons should be obtained.
Pellegrini-Stieda lesion
Long-term effects of avulsion of the medial collateral ligament from its femoral attachment, causing local pain and heterotopic ossification, comprise the “Pellegrini-Stieda” lesion.
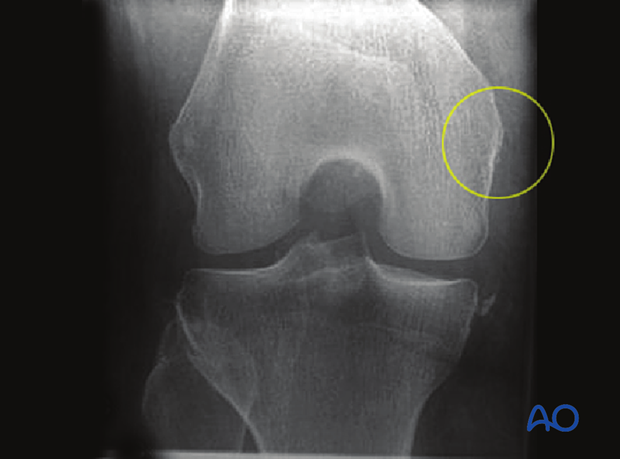
Lateral fracture
Avulsion of the lateral collateral ligament from the distal femur may accompany serious injuries to the knee. There may be peroneal nerve, or meniscal, injuries.
Similar principles apply to the fracture treatment on both the lateral and medial side of the distal femur.
To illustrate the principles of reduction and fixation, we will show the medial avulsion injury.
2. Patient preparation and approach
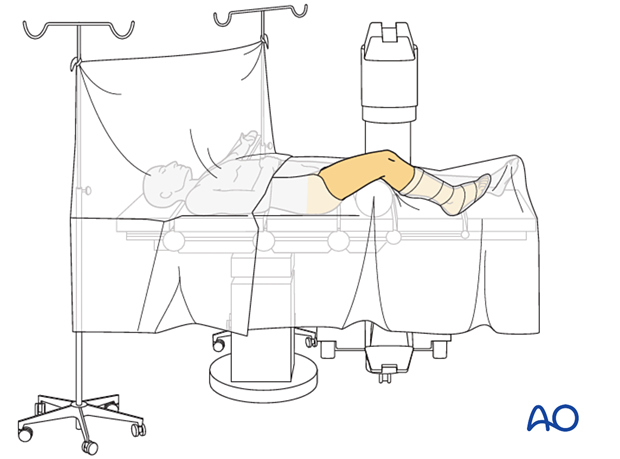
Positioning
This procedure may be performed with the patient in one of the following positions:
- Supine position knee flexed 30°
- Supine position knee flexed 90°
- Lateral decubitus (particularly in obese patients)
Surgical approach
For avulsion fractures from the lateral epicondyle, the lower end of the standard lateral/anterolateral approach is used.
For medial fractures, a direct medial longitudinal incision immediately over the medial epicondyle is used (approx. 2 cm long) and deepened cautiously to expose the medial face of the medial condyle. Care is taken to avoid the saphenous nerve and its infrapatellar branch.
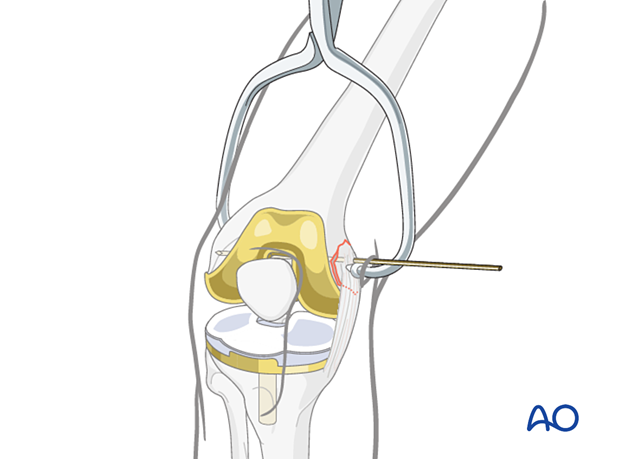
3. Reduction
Reduce the fracture with a large pointed reduction forceps. Small thin fragments may fracture if such a forceps is applied, and reduction and control with a dental pick may be preferable. The fracture is then secured with a temporary K-wire, taking care not to conflict with the proposed screw track.
4. Fixation
Drill hole for the lag screw
The forceps are then removed, and the hole for the lag screw is drilled through the center of the avulsed fragment.

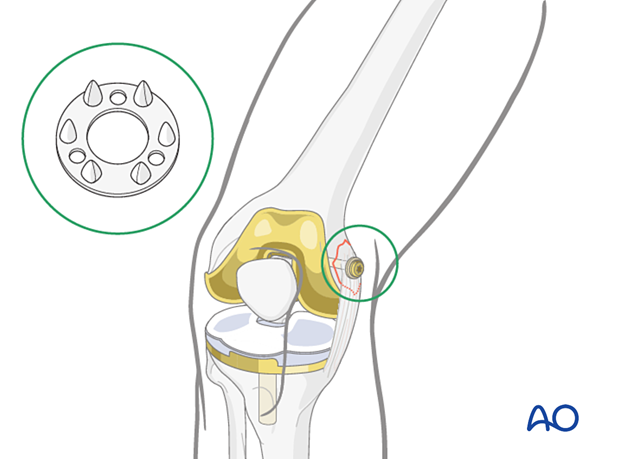
Insertion of lag screw
Insert a cannulated or non-cannulated lag screw according to the standard procedure.
To secure the ligaments and small, thin fragments, a special ligament washer can be used on the screw. These washers are made of either metal, or plastic material.
Final examination
Gently examine the knee under anesthesia to test for ligament instability. Be careful not to stress the reattached ligament too aggressively.
5. Aftercare
Functional treatment
Gentle range of motion with or without a hinged-knee brace is begun early and continued for 6 weeks.
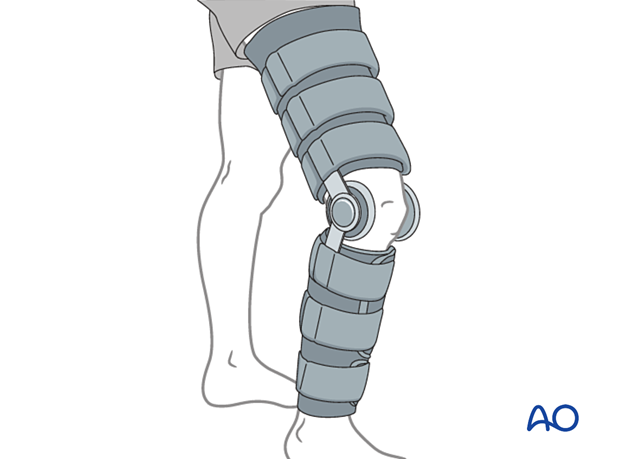
Functional treatment
Early progressive partial weight bearing (touch down, or 10-15 kg) may be performed, with the aid of crutches, or a walker.
Follow-up
Wound healing should be assessed regularly within the first two weeks. Subsequently 2, 6 and 12 week follow-ups are usually made. A longer period of follow-up may be required if the fracture healing is delayed. Complete knee extension must be achieved or limping is expected.
Thrombo-embolic prophylaxis
Consideration should be given to thrombo-embolic prophylaxis, according to local treatment guidelines.













