Lateral/anterolateral approach to the distal femur
1. General considerations
The lateral approach to the distal femur allows for visualization, reduction, and fixation of the distal femur.
The lateral approach relies on an atraumatic elevation of the vastus lateralis from the lateral aspect of the distal femur, and a lateral arthrotomy for joint visualization. The approach can be extended proximally, as described in the lateral approach to the femoral shaft (click here for a description of the lateral approach to the femoral shaft).
The approach can also be used without an arthrotomy if it is not required to visualize the inside of the joint.
This approach is safe in the presence of a healed previous midline skin incision for a total knee replacement.
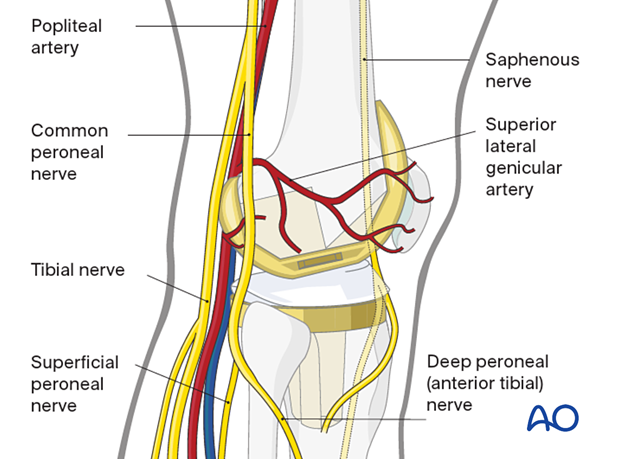
Neurovascular risks
There are no significant arteries, veins, or nerves on the lateral side of the knee.
There may be bleeding from the lateral genicular arteries, which will need to be controlled using diathermy.
At the posterior aspect of the knee lie the popliteal artery, nerve, and vein. It must be borne in mind that these structures can be damaged by the injury or can be damaged by the surgeon during the reconstruction.
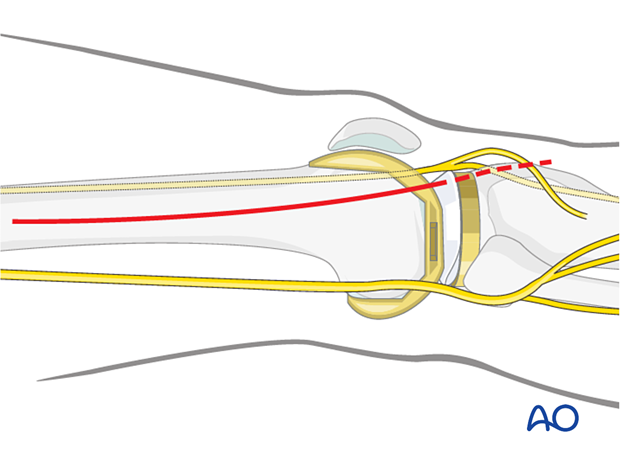
2. Skin incision
Begin the skin incision in the mid-lateral line of the femoral shaft at Gerdy's tubercle and curve it proximally over the lateral femoral condyle. The proximal starting point for the skin incision depends on the most proximal extent of the fracture.
The need for a distal extension of the skin incision depends on whether an arthrotomy needs to be performed. If joint visualization is required, the incision is carried beyond the level of the Gerdy's tubercle (dashed line).
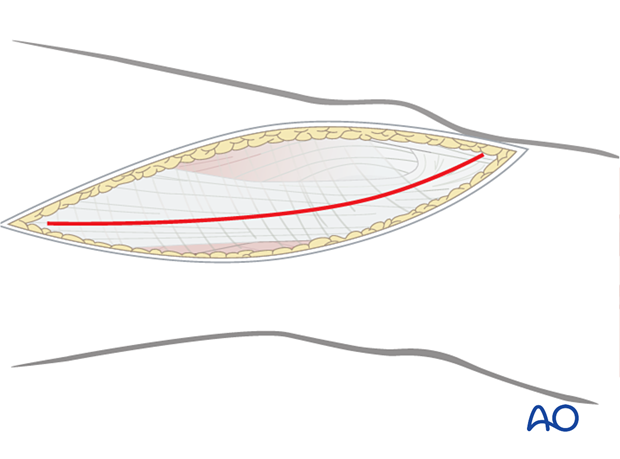
3. Division of the iliotibial band
Divide the iliotibial band (tract) in line with the skin incision. Distally, the fibers slope anteriorly towards the Gerdy's tubercle. The incision through the iliotibial band should follow the muscle fiber orientation. To facilitate a perfect closure, the iliotibial band should be divided in one precise incision only.
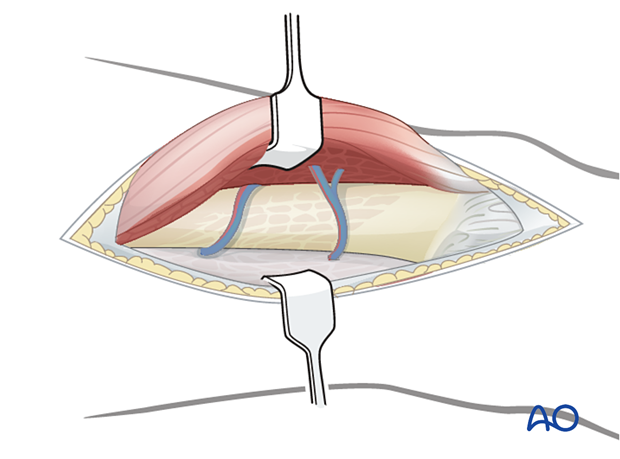
4. Elevation of vastus lateralis
Beneath the iliotibial band, the muscle fibers of the vastus lateralis are minimal in the distal 8-10 cm of the femur. Incise the muscle fascia surrounding the vastus lateralis just anterior to the lateral intermuscular septum and elevate the muscle fibers of the septum, working from distal to proximal. This is most easily accomplished by the use of a large elevator.

Retract the vastus lateralis anteromedially. Several perforating vessels of the profunda femoris artery and vein must be ligated. Failure to do so will result in excessive bleeding. It is important to only remove muscles from the lateral surface of the distal femur and protect as much periosteum surrounding the distal femur as possible for later fracture healing.
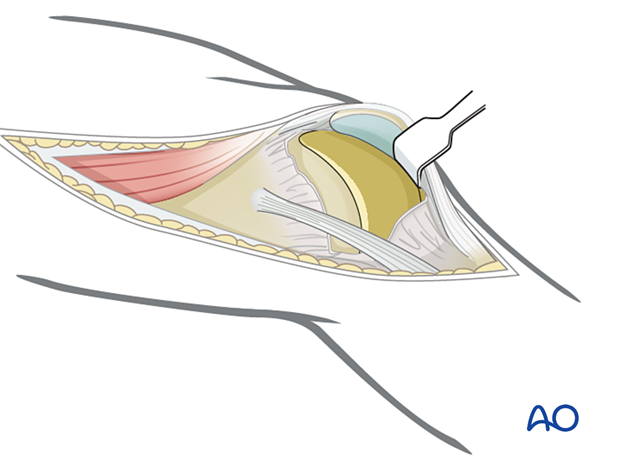
5. Joint capsule arthrotomy for articular surface visualization (optional)
For cases in which the joint needs to be exposed, perform a joint capsule arthrotomy.
Distally, incise the joint capsule over the anterior third of the lateral femoral condyle. This joint arthrotomy can be carried distally as far as the lateral tibial component. Bleeding from branches of the genicular vessels might be encountered and should be cauterized.
To facilitate further exposure of the joint surface, use a blunt angled retractor. Take care to avoid excessive tension on the patellar tendon, especially in osteoporotic individuals.
6. Wound closure
Close any joint capsule arthrotomy with absorbable sutures.
Proximally, close the fascia of the vastus lateralis with a running absorbable suture or interrupted sutures.
Close the iliotibial band with absorbable sutures. Close the skin and subcutaneous tissues in a routine manner.














