Posterior column screw fixation
1. Principles
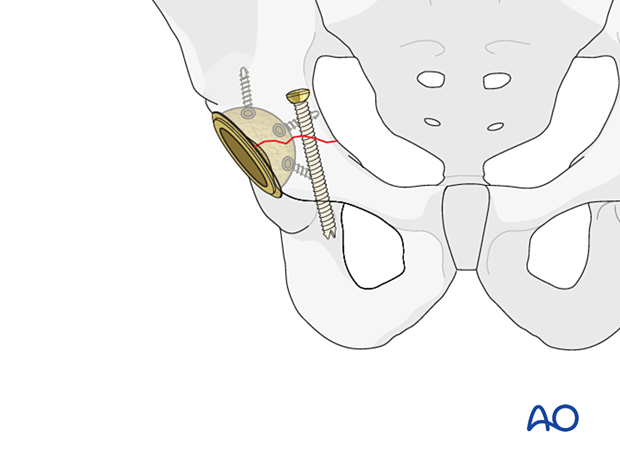
Fracture morphology and surgeon's experience will dictate the choice of fixation method to achieve fracture stability and maintain cup stability.
In the setting of intraoperative stable fractures, the acetabular exposure will already be complete. The relative risk of screw stabilization in a fracture that appears to be stable must be evaluated by the surgeon. If there is a safe opportunity for screws stabilization it should be considered to minimize the possibility of late displacement.
For further information about standard techniques for ORIF in native acetabular fractures, please refer to the acetabulum section of the AOSR.
2. Implant selection
Column screw fixation is typically performed with non-cannulated screws when the fracture is reduced openly as the starting point is easily visualized.
Percutaneous methods are often aided using cannulated screw fixation. Ideally, screws with an outer diameter over 6.5 mm will provide the most rigid guide pin and prevent guide pin complication.
The column corridors of the bone must allow for screws of this caliber.
3. Fracture exposure and reduction
Exposure through open posterior approach
A posterior approach to the hip typically provides access to posterior column screw fixation. In this approach, the patient is placed in a lateral position.

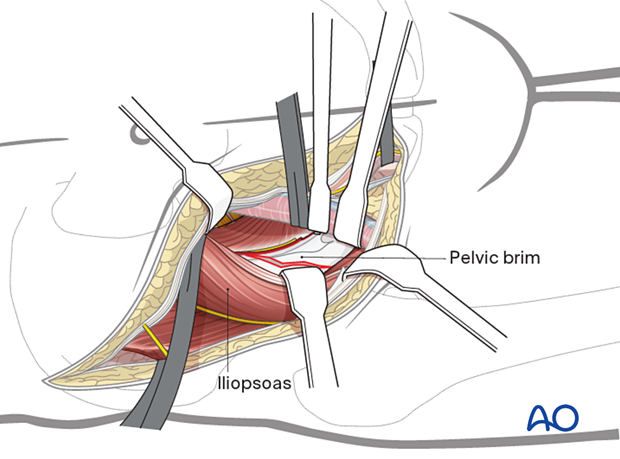
Exposure through open lateral window of the ilioinguinal approach
This procedure can be performed via an exposure into the lateral window of the ilioinguinal approach which is often available to the surgeon within the sterile field. In this approach, the patient is placed in a supine position.
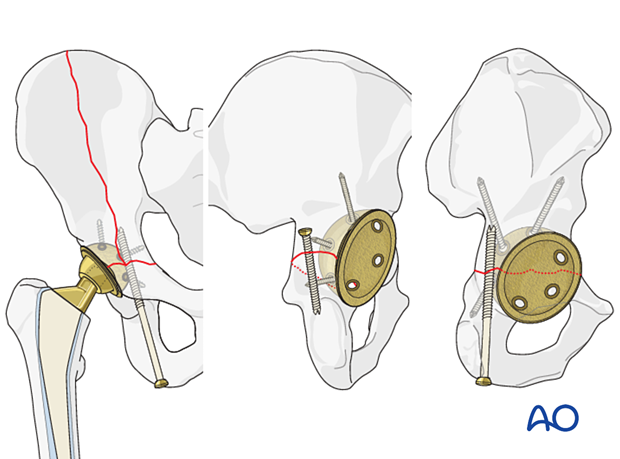
Posterior column fracture reduction
In these fractures, anatomic reduction of the articular surface is not relevant. Columnar stability and wall containment are needed.
If there is a transverse fracture or a posterior column fracture, utilization of pelvic reduction clamps might be helpful.
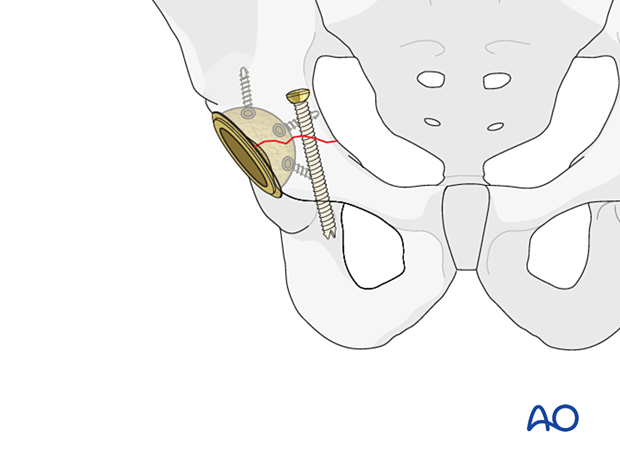
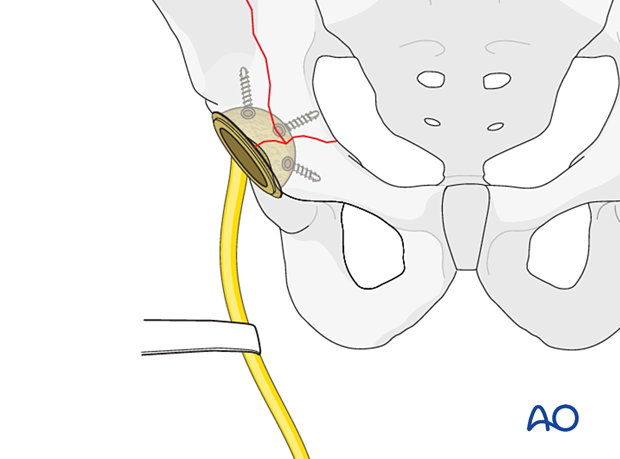
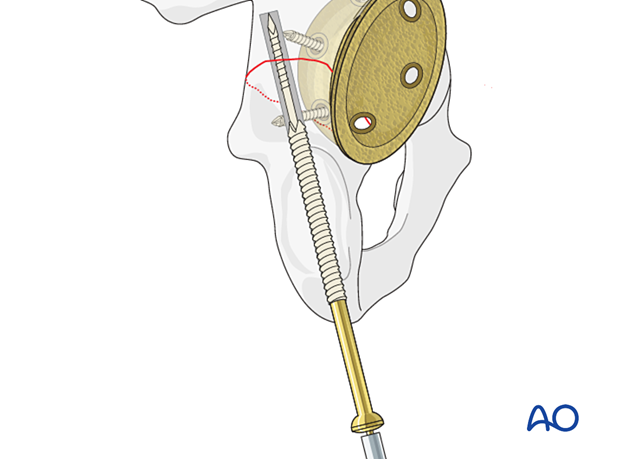
4. Screw application in antegrade fashion
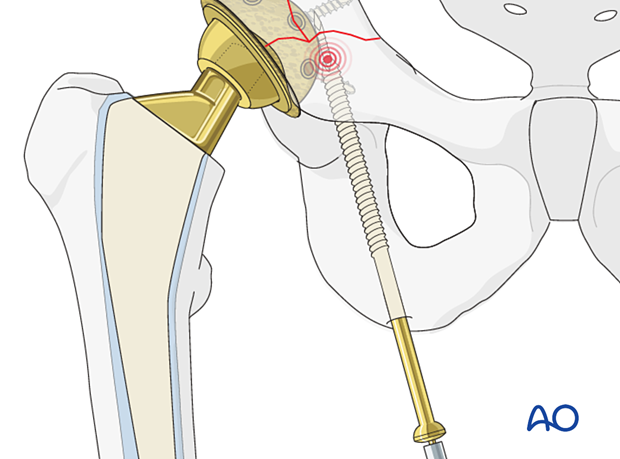
Posterior column fixation
Posterior column screw is applied in the antegrade fashion from the lateral window of the ilioinguinal approach into the ischium.
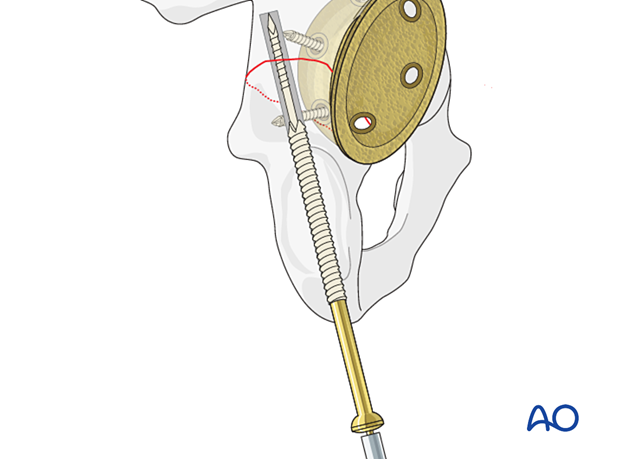
5. Reduction and screw application in retrograde fashion
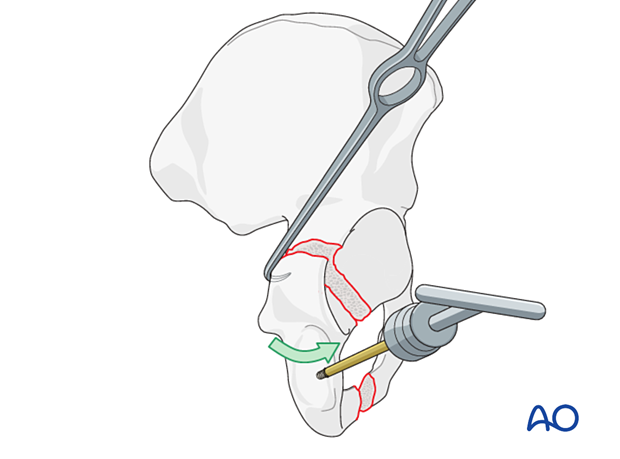
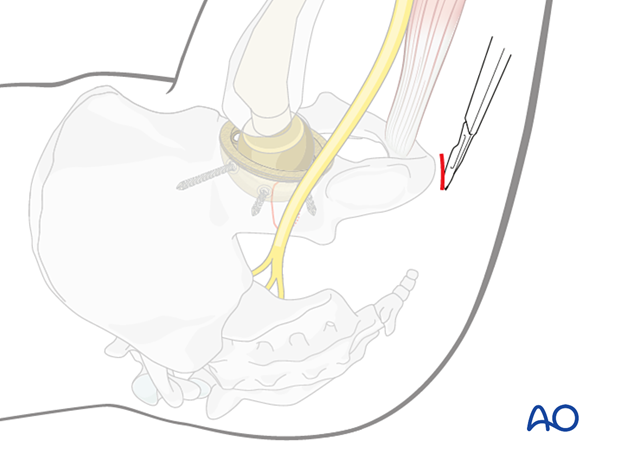
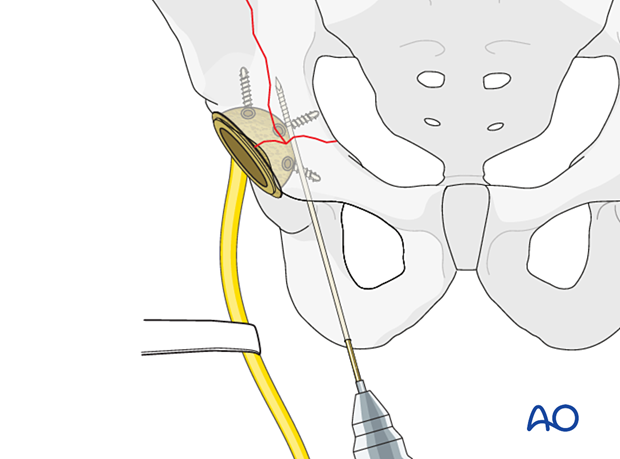
Percutaneous ischial tuberosity access
Screws can be inserted in the posterior column in a retrograde fashion from the ischial tuberosity.
With the hip flexed approximately 45 to 60 degrees, a 2 cm incision is made over the ischial tuberosity.
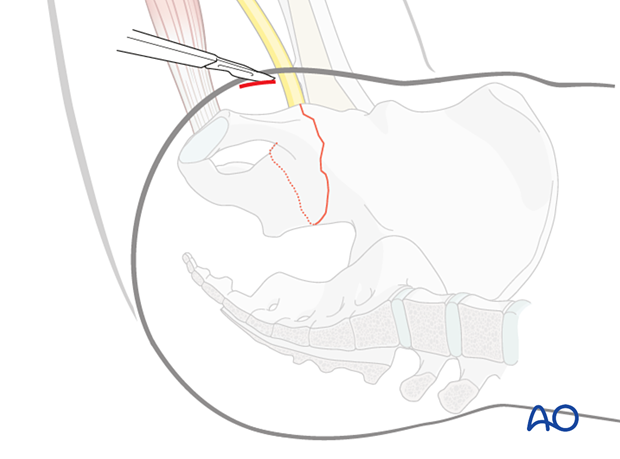
The sciatic nerve is carefully retracted laterally.
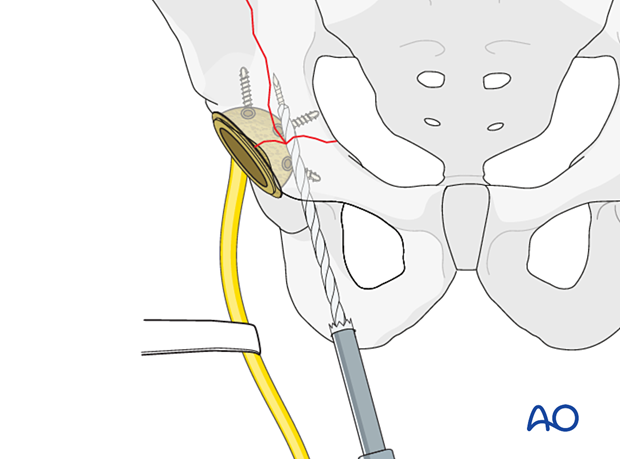
The drill guide is placed onto the ischial tuberosity.
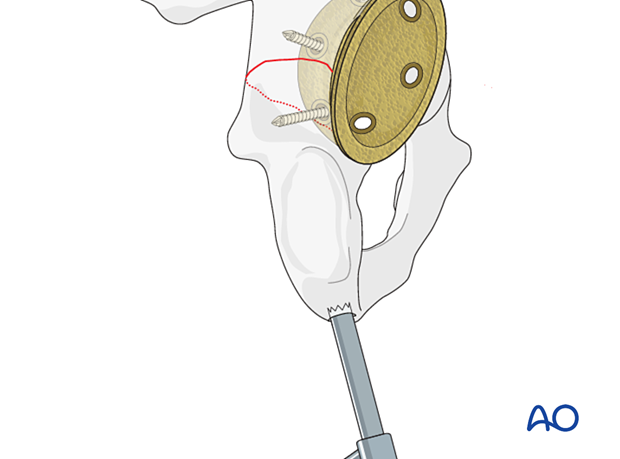
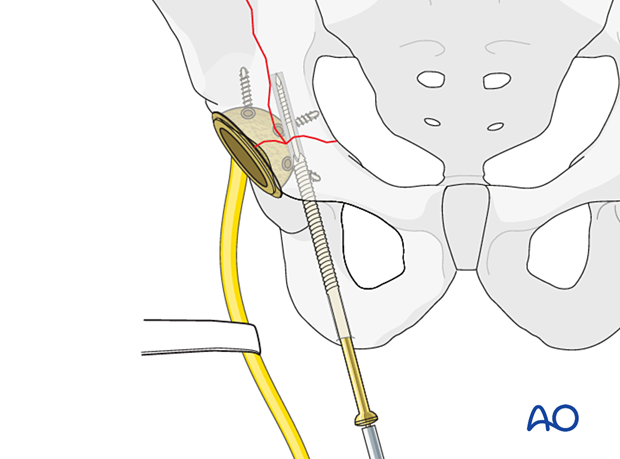
A long guidewire is inserted and its placement confirmed utilizing fluoroscopy or intraoperative CT.

Consider drilling the entry point of the posterior column.
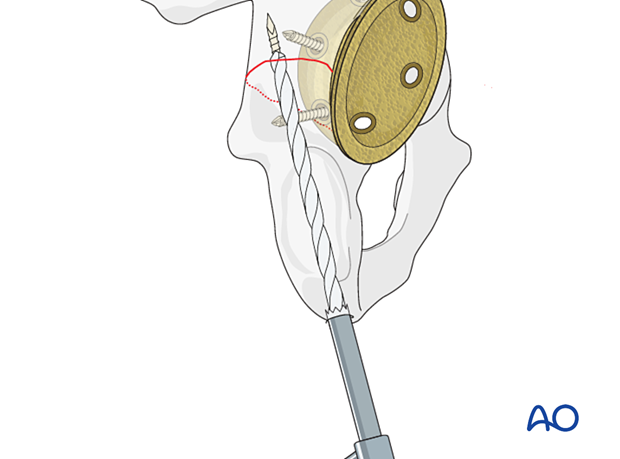
The screw is inserted over the guidewire.
Percutaneous anterior approach
From an anterior approach to the hip, when the patient is supine, a percutaneous approach can be applied depending on the location of the fracture and the experience of the surgeon.
The posterior column can be addressed with the hip flexed approximately 45 to 60 degrees, a 2 cm incision is made over the ischial tuberosity.
The sciatic nerve is carefully retracted laterally.
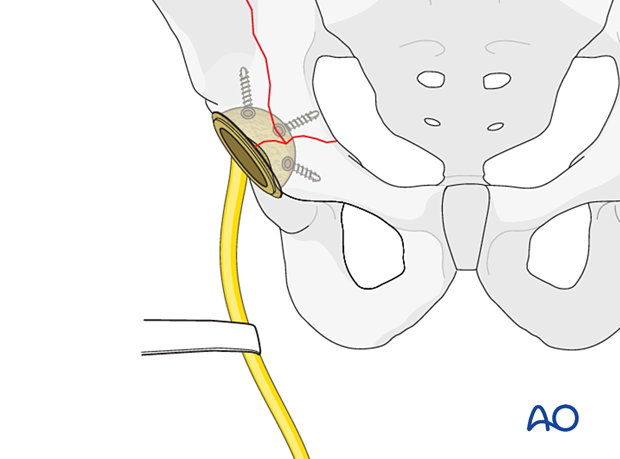
The drill guide is placed onto the ischial tuberosity.
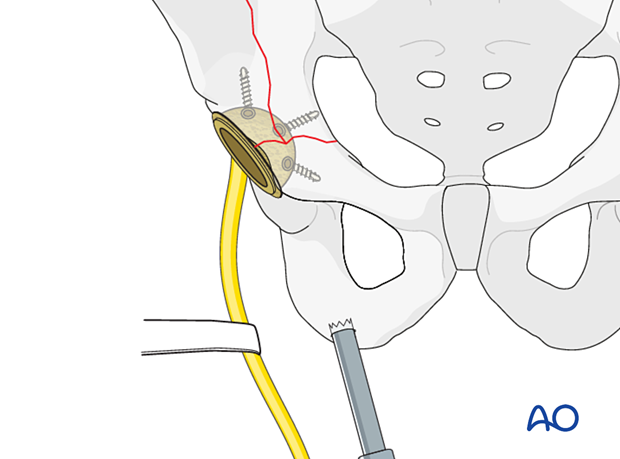
A long guide-pin is inserted, and its placement confirmed utilizing fluoroscopy or intraoperative CT.
Consider drilling the entry point of the posterior column.
The screw is inserted over the guidewire.
6. Aftercare following ORIF
Postoperative management
Postoperative management should include careful monitoring of hematocrit and electrolytes particularly in the elderly patients.
Postoperative IV antibiotics should be administered up to 24 hours.
Consideration should be given to anticoagulation for a minimal course of 35 days. If there are thromboembolic complication this treatment is extended.
Drains can be discontinued when output is less than 30 to 50 cc per 12 hours.
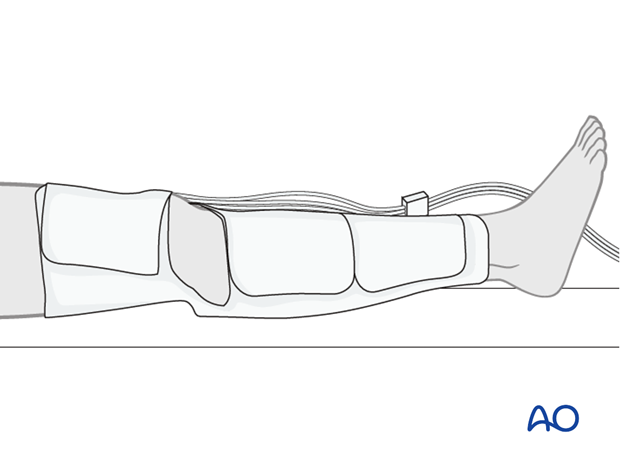
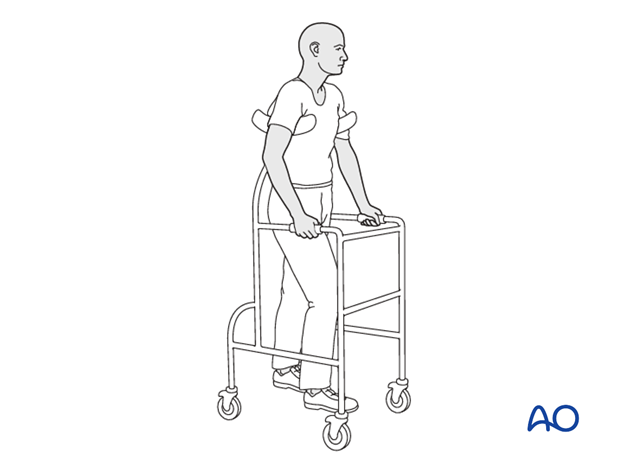
Patient mobilization
Immediate mobilization of the patient should commence. If fracture stability will allow, the patient should be made weight bearing as tolerated as soon as possible. Long periods of limited weight bearing are extremely detrimental to patient recovery.
Precautions against hip dislocation
Hip precautions can be extremely important in patients who have suffered intraoperative acetabular fracture. Much work has been done to minimize the surgical exposure during hip arthroplasty to decrease the risk of dislocation. These advantages are typically removed when acetabular stabilization need to be performed. A dislocation in the postoperative course of such a patient can be disastrous.
Patients are instructed to follow standard hip precautions against dislocation based upon the surgical approaches for hip arthroplasty.
Wound healing
Avoidance of edema postoperatively is critical for both wound healing and patient mobilization. This can be aided by pneumatic compression devices. If negative pressure wound therapy is utilized, it can be discontinued after 5 to 7 days. Staples or sutures are typically removed at 14 to 21 days.