MIPO
1. General considerations
Introduction
Diaphyseal fracture healing in pediatric patients occurs more rapidly as the periosteum has the ability to form new bone. Therefore, periosteal stripping or compression should be avoided. A minimally invasive approach in pediatric patients is particularly useful as it causes less damage to the periosteum.
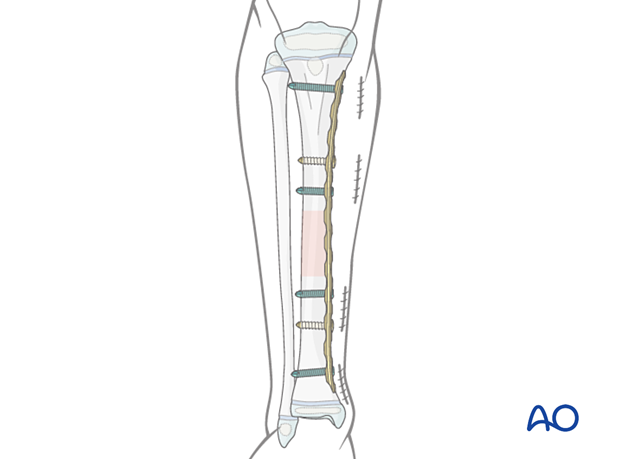
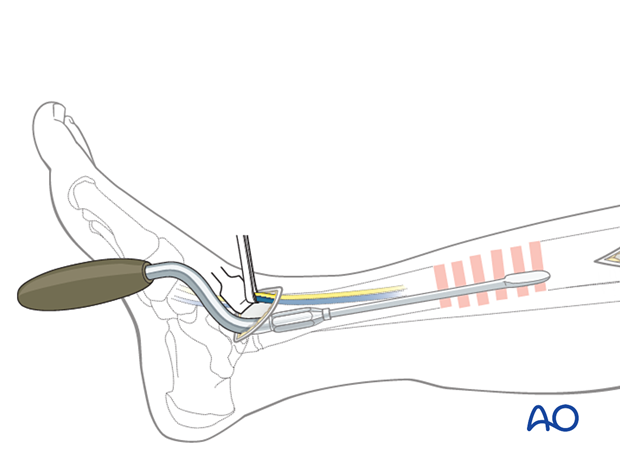
Plates inserted through a minimally invasive approach leave the soft tissues intact over the fracture site. The incisions are made proximally and distally, and the plate is inserted through a submuscular tunnel. The insertion typically requires monitoring under image intensification.
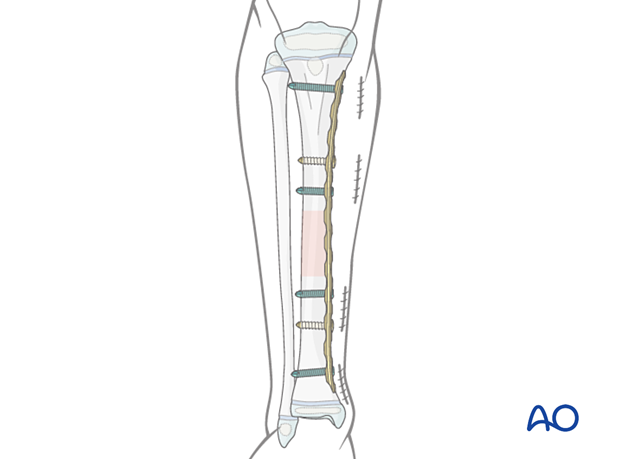
Minimally invasive plating may be performed for diaphyseal fractures of the tibia.
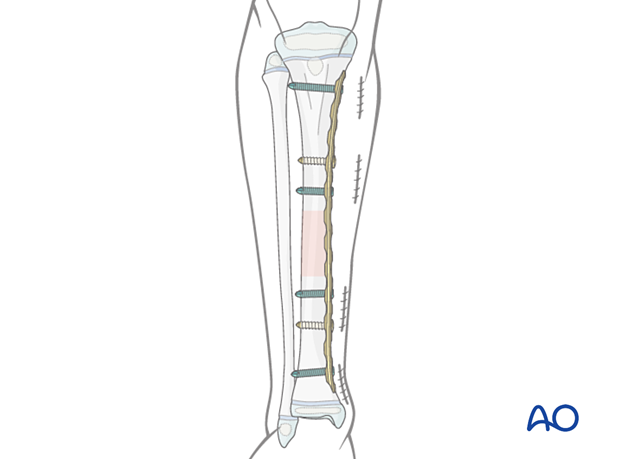
There should be at least three bicortical cortical or two locking head screws in each main fragment.
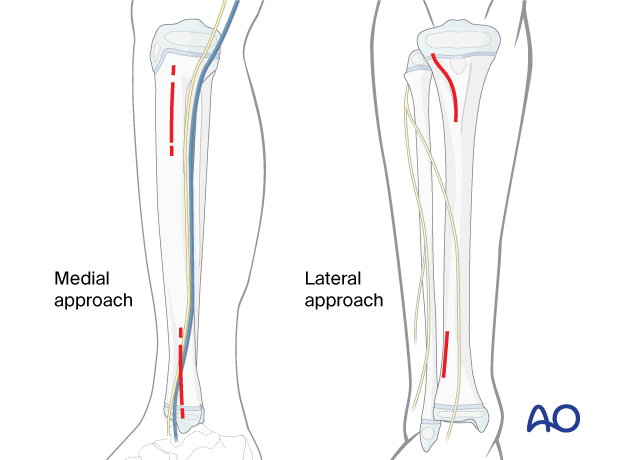
Typically, the plate is applied medially. If there is medial soft-tissue damage, lateral plating may be selected.
In this procedure, MIPO of a generic fracture of the middle third of the tibia is shown.
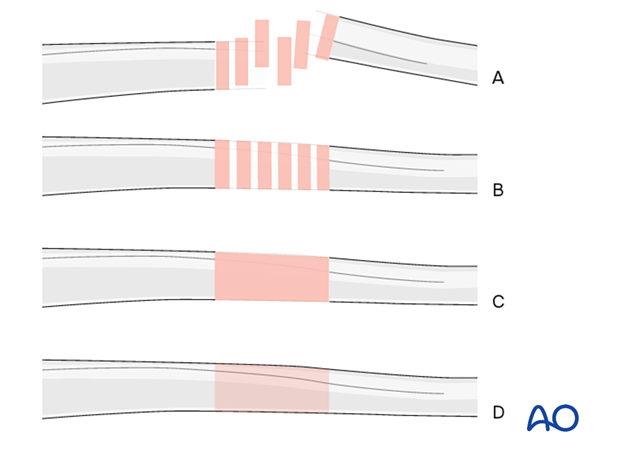
Throughout this section, generic fracture patterns are illustrated as:
- Unreduced
- Reduced
- Reduced and provisionally stabilized
- Definitively stabilized
Bridge plating
In pediatric shaft fractures, MIPO is usually performed in bridging mode.
This uses the plate as an extramedullary splint, fixed to the two main fragments, preserving the fracture zone.
Anatomical reduction of any intermediate fragments is not necessary. Furthermore, direct manipulation risks disturbing their blood supply.
If the soft-tissue attachments to these fragments are preserved and the fragments are relatively well aligned, healing is not disturbed.
Mechanical stability, provided by the bridging plate, is adequate for functional rehabilitation and results in healing with abundant callus formation.
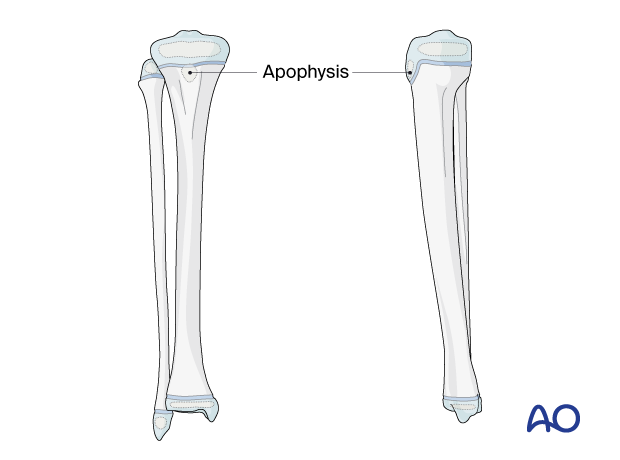
Proximal and distal tibial physes
The physis at each end of the tibia must be protected during surgical approaches and implant application.
The proximal tibial physis extends anteriorly and distally as an apophysis, which forms the tibial tuberosity.
This may be damaged as a consequence of injury and surgery, leading to tibial deformity.
2. Implant selection
Plate size
For younger children, a 3.5 plate can be used.
For older children and adolescents, a narrow 4.5 mm plate is typically used.
A locking plate is a good option for fractures with a short end segment. The plate does not need to be contoured precisely to fit the bone, as it functions as an internal fixator. Attaching it to the bone does not alter fracture alignment, as locking screws do not pull the main bone fragments to the implant. If cortical screws are used, contouring is important.
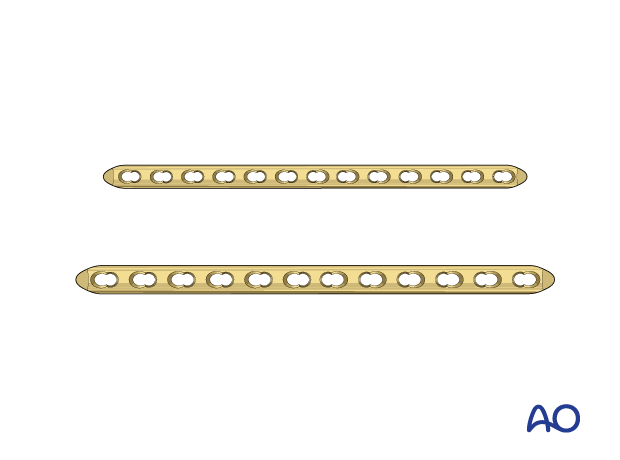
Plate length and number of screws
The plates for a bridging technique should be longer than for conventional “anatomical” fixation to distribute the forces more widely, as well as to provide sufficient stability.
A minimum of two and up to four bicortical locking-head screws should be inserted into each fracture fragment.
Do not fill all screw holes to ensure relative stability and enhanced fracture healing.
3. Patient preparation and approaches
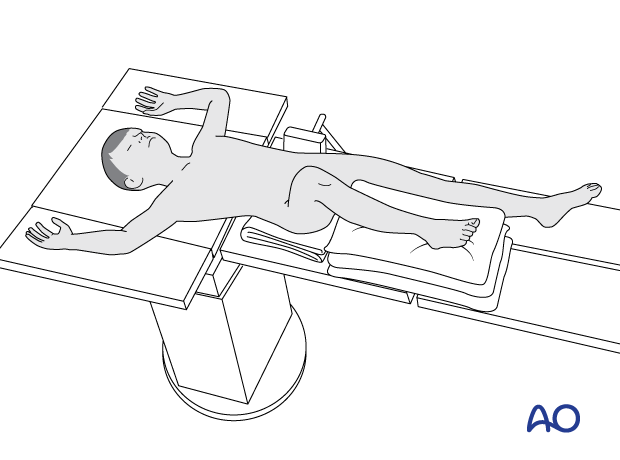
Patient positioning
Place the patient in a supine position on a radiolucent table.
Elevate the lower leg with a stack of towels.
Approaches
For this procedure, a minimally invasive approach is used.
4. Preliminary reduction
It is important to restore alignment, length, and rotation.
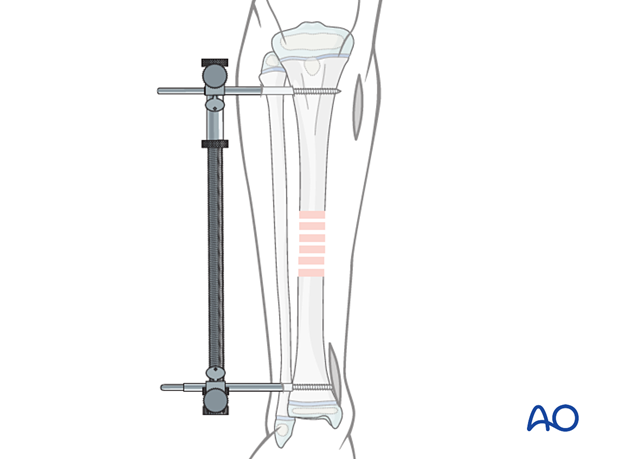
Reduction can be performed with a distractor, external fixator, or implant.
Manual traction is often sufficient for preliminary reduction.
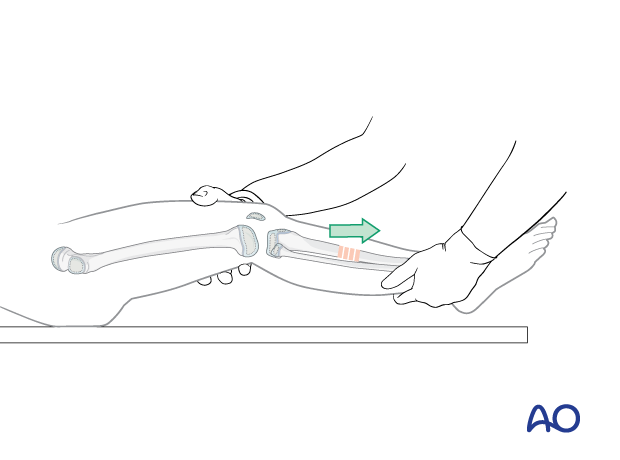
The application of a distractor helps maintain length and alignment, especially in older patients.
5. Contouring and insertion of the plate
Plate contouring
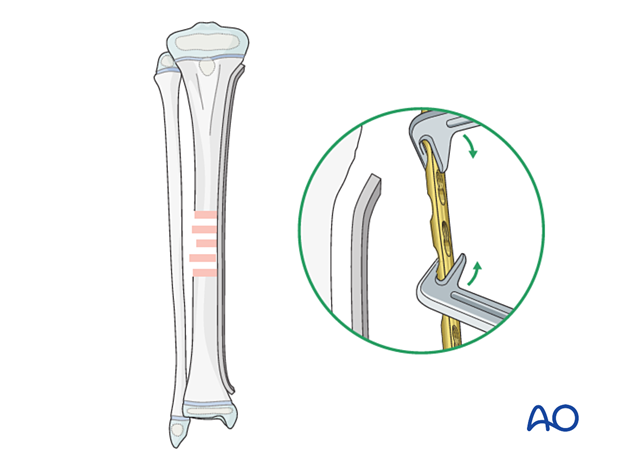
Contouring the plate over the fracture zone is not usually required.
Proximal and distal contouring of the plate may be necessary.
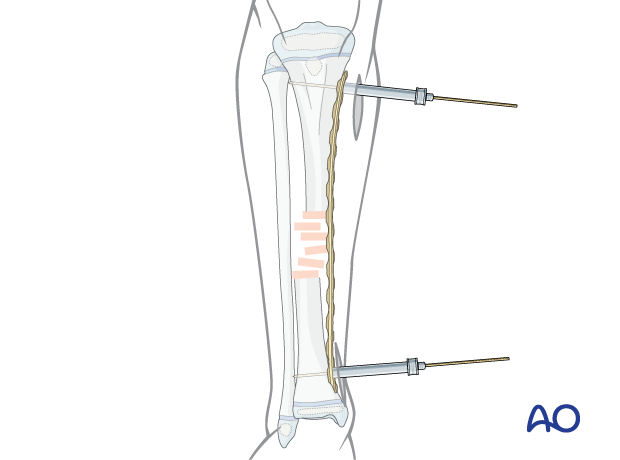
Direction of plate insertion
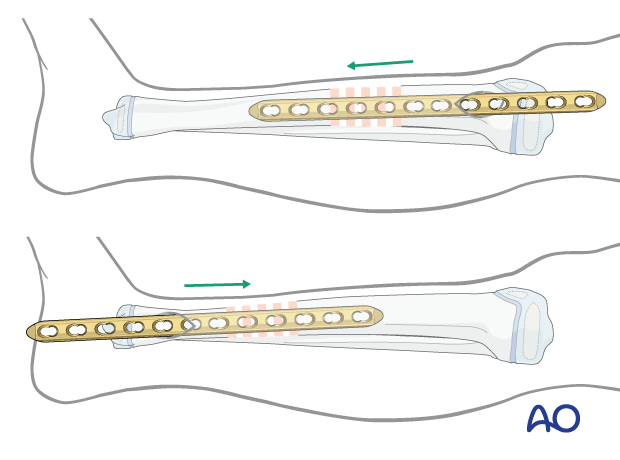
Insert the plate from the incision that is closest to the fracture.
Preparation of the plate tunnel
Use a soft-tissue elevator, or an appropriate plate, to prepare a tunnel.
6. Reduction and fixation
In tibial shaft fractures, final reduction and plate fixation are typically performed simultaneously using the plate as a reduction tool.
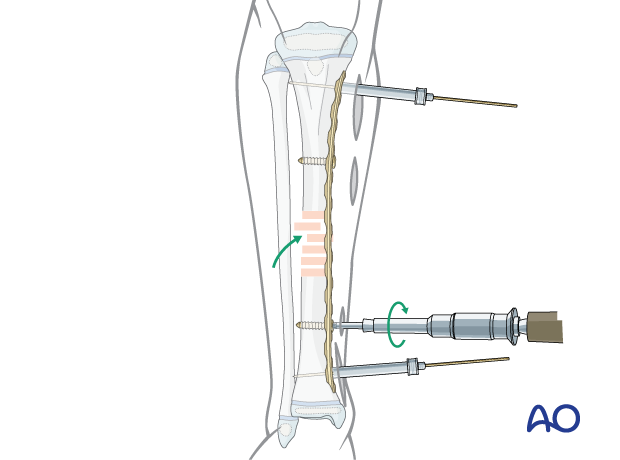
Cortical, locking-head, or a combination of screws may be used.
Locking head screws are preferred as they provide a better mechanical and biological environment.
A cortical screw may be used to reduce the gap between the plate and the bone. Compression of the plate against the periosteum must be avoided.
Locking head screws should then be inserted to hold the plate in position.
Attach the plate to the bone using temporary K-wires applied through proximal and distal positioning holes or through the most peripheral screw holes using appropriate sleeves.
Confirm alignment of the tibia and the position of the plate clinically and radiographically.
In cases where reduction is difficult, reduction forceps can be used via a small incision.
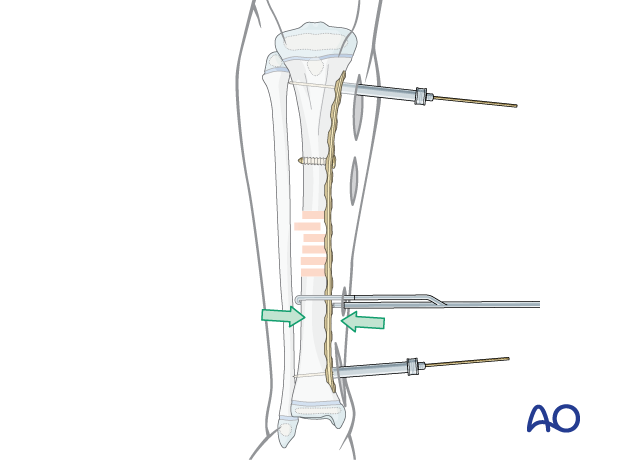
A cortical screw may be used to appose the plate to the bone as an alternative.
A small gap between the bone and the implant is to be anticipated and ignored.
Final screw fixation
The final reduction is achieved by inserting locking head screws according to the preoperative plan with optional removal of the reduction screws.
For older or heavier children, at least three screws are recommended for each main fragment.
7. Final assessment
Compare leg length and rotation with the uninjured leg.
Confirm and document the final construct with an image intensifier in two planes.
8. Aftercare
Postoperative documentation
X-rays in two planes (AP and lateral) of the tibia with adjacent joints should be taken to confirm fracture reduction.
Immediate postoperative care
Toe-touch weight bearing is recommended for 2–6 weeks and depends on fracture stability.
Older children may be able to use crutches or a walker.
Younger children may require a period of mobilization in a wheelchair.
Neurovascular examination
The patient should be examined frequently to exclude neurovascular compromise or evolving compartment syndrome.
Follow-up
Clinical follow-up is undertaken to check wound healing.
A radiological follow-up for bone healing should be taken after about 4–6 weeks.
Mobilization
Graduated weight bearing is usually possible after early clinical and radiological signs of consolidation.
Patients are encouraged to start range-of-motion exercises. Physiotherapy supervision may be necessary in some cases but is not mandatory.
Sports and activities that involve running and jumping are not recommended until full recovery of local symptoms and function.
Implant removal
Implant removal is not mandatory and requires a risk-benefit discussion with patient and carers.
A medial subcutaneous plate may cause local soft-tissue irritation.
Follow-up for growth disturbance
Leg length should be evaluated up to 2 years following injury due to the effect of growth stimulation.













