Minimally invasive medial approach to the tibia
1. Principles
Periosteum makes an important contribution to fracture healing in the immature skeleton.
A minimally invasive approach is, therefore, particularly useful in pediatric patients as it causes less damage to the periosteum.
Minimally invasive fixation of tibial fractures, particularly distal fractures, is usually performed through the medial approach.
This may not be possible if the overlying skin is injured.
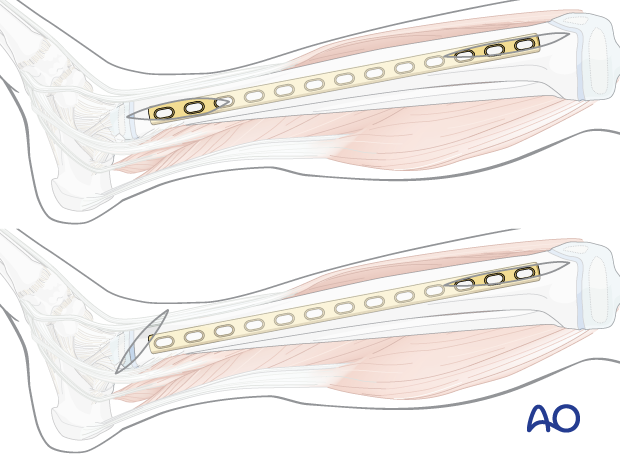
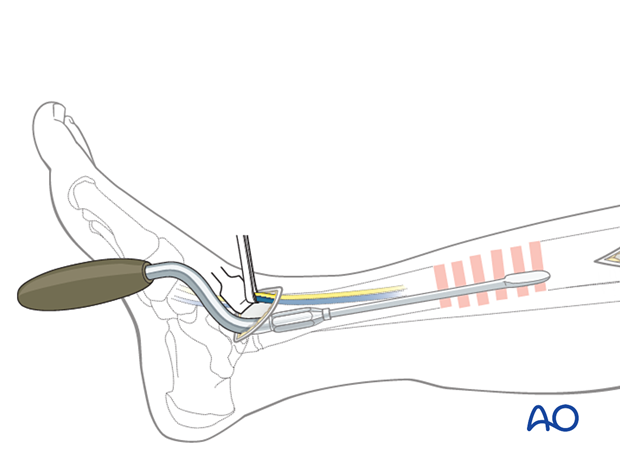
A contoured plate can be passed subcutaneously to fit the medial tibial surface.
This approach leaves the periosteum and muscles intact and does not affect the tibial blood supply.
2. Anatomy
The triangular shape of the tibia
The lateral and posterior surfaces of the tibia are covered by muscle. The anteromedial surface has only a thin layer of subcutaneous tissue and skin. This surface provides less blood supply to the underlying bone.
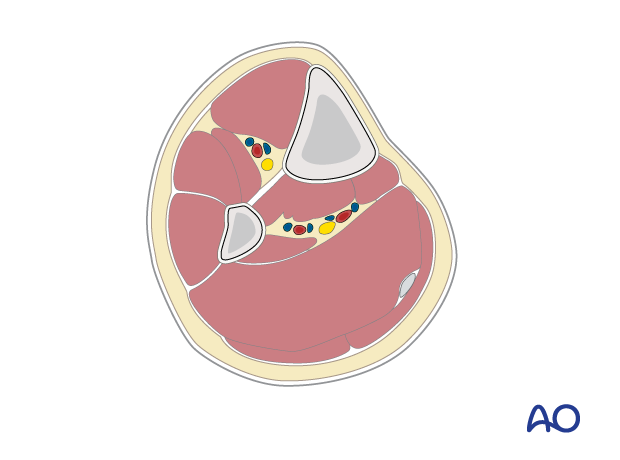
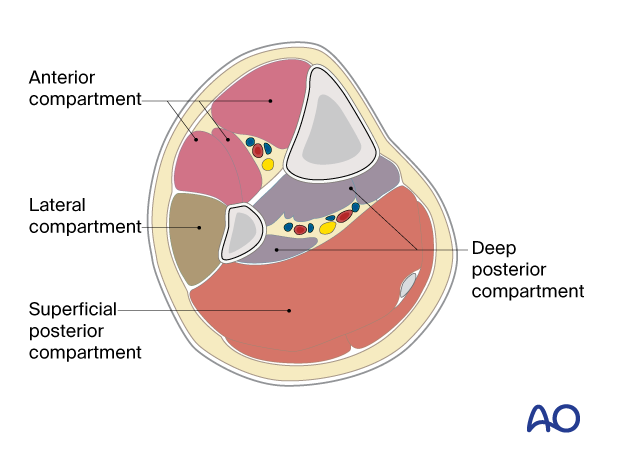
Compartments
The lower leg has four compartments.
The anterior compartment contains:
- Tibialis anterior
- Extensor hallucis longus
- Extensor digitorum longus
- Anterior tibial artery
- Deep peroneal nerve
The lateral compartment contains:
- Peroneus longus
- Peroneus brevis
- Superficial peroneal nerve
The deep posterior compartment contains:
- Tibialis posterior
- Flexor hallucis longus
- Flexor digitorum longus
- Peroneal artery
- Posterior tibial artery
- Tibial nerve
The superficial posterior compartment contains:
- Gastrocnemius
- Soleus
- Sural nerve
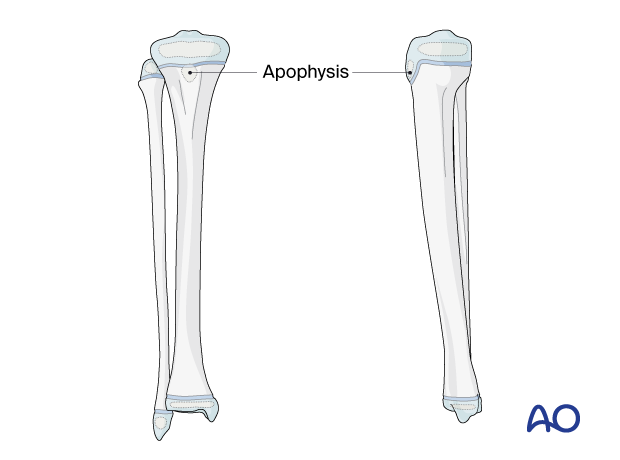
Proximal and distal tibial physes
The physis at each end of the tibia must be protected during surgical approaches and implant application.
The proximal tibial physis extends anteriorly and distally as an apophysis, which forms the tibial tuberosity.
This may be damaged as a consequence of injury and surgery, leading to tibial deformity.
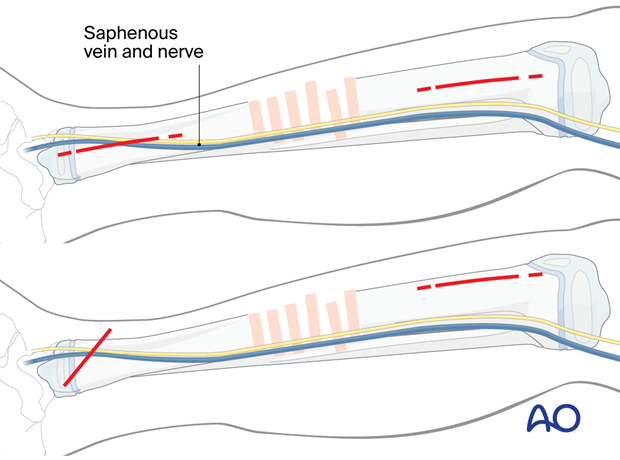
3. Skin incisions
Identify the level of the physis with image intensification and mark this on the skin before making an incision.
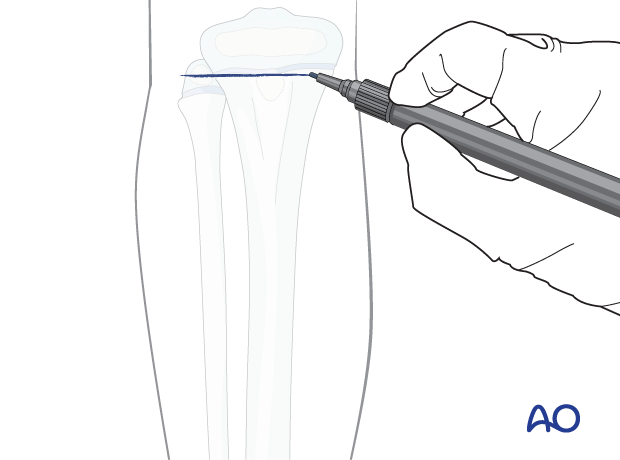
Make separate proximal and distal skin incisions, approximately 5 cm long, on the medial surface of the tibia.
The incisions span a length equal to that of the planned plate.
Distally, two options are possible:
- Straight incision
- Slightly oblique incision
The oblique incision may increase the risk of injury to the saphenous nerve and vein, which should be identified and protected.
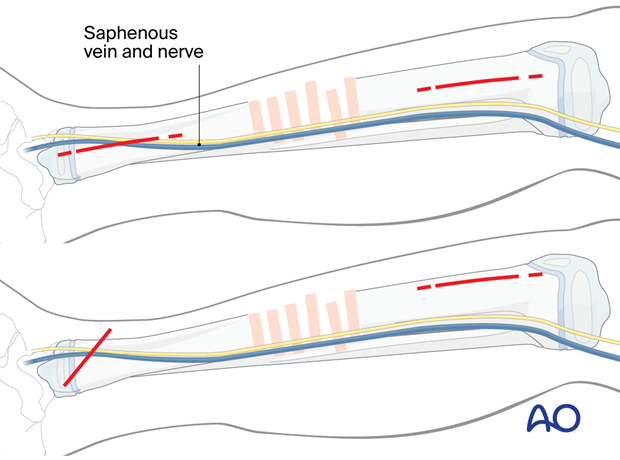
The straight incision lies directly over the plate.
The oblique incision does not lie directly over the plate and allows insertion while reducing the risk of wound healing complications.
4. Deep dissection
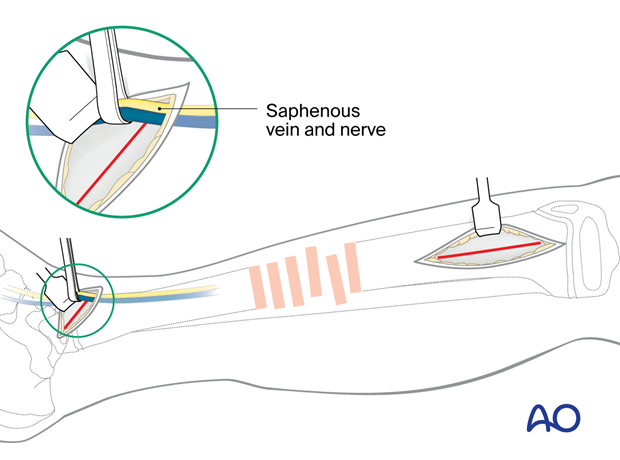
Deepen the dissection to the periosteum, which is left intact.
Identify and protect the great saphenous vein and nerve in the distal incision.
Make sure not to damage the perichondral ring at either physis.
A large distractor may be used to reduce and stabilize the fracture.
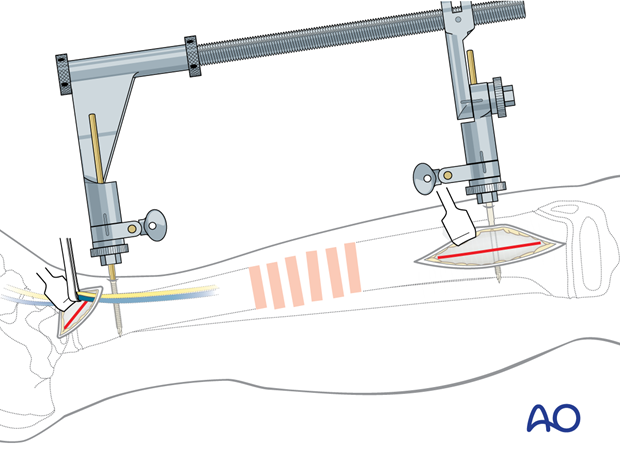
Retract the anterior tibial vessels and deep peroneal nerve laterally or anteromedially under direct vision and use a soft-tissue elevator, or an appropriate plate, to prepare a tunnel between the anterior compartment muscles and the periosteum.
5. Wound closure
Close the skin and subcutaneous tissues according to surgeon preference.













