Open reduction; plate fixation (ulna)
1. General considerations
Introduction
Plating is the standard technique for treating forearm fractures in adults and is also appropriate for children approaching skeletal maturity.
Children with open physes have thick active periosteum favoring stability and rapid healing with ESIN techniques. In more proximal ulnar fractures plating may be used in younger children.
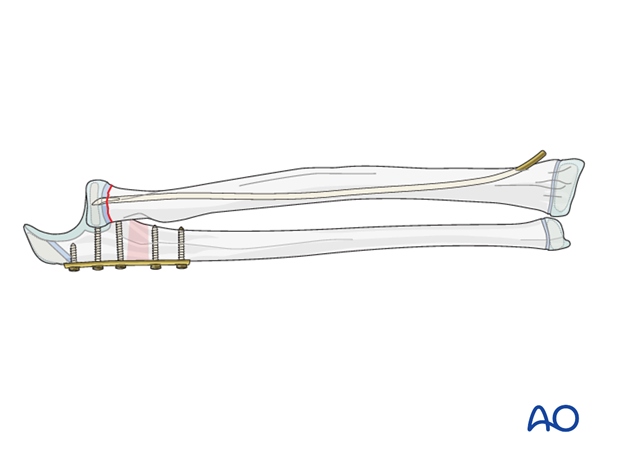
Combination with other treatment options
Plating the ulna may be combined with ESIN of the proximal radial fracture.
This allows for stable anatomical restoration of the forearm axis and early motion.
K-wire fixation of the radial fracture may be performed but is not recommended. This provides less stability and requires additional immobilization.
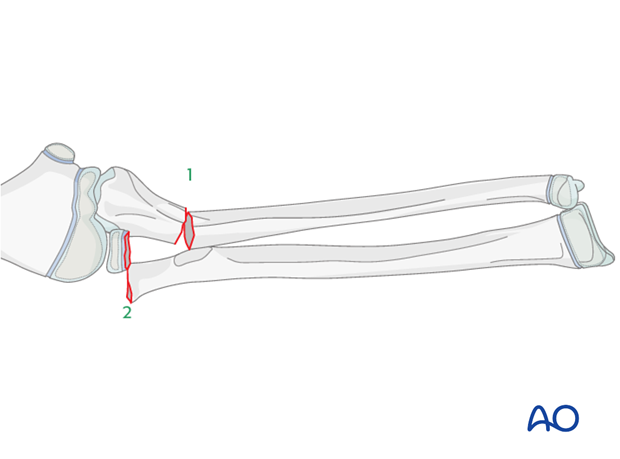
2. Order of reduction and fixation
The ulnar fracture (1) is treated first.
The radial neck fracture (2) may spontaneously reduce after anatomical reduction and fixation of the ulna.
The radial neck fracture should be fixed with an intramedullary nail to prevent redisplacement and to allow early joint mobilization.
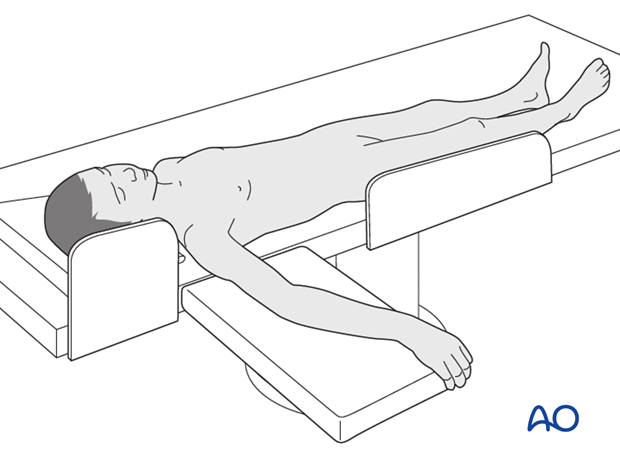
3. Patient preparation
This procedure is normally performed with the patient in a supine position.
4. Choice of approach
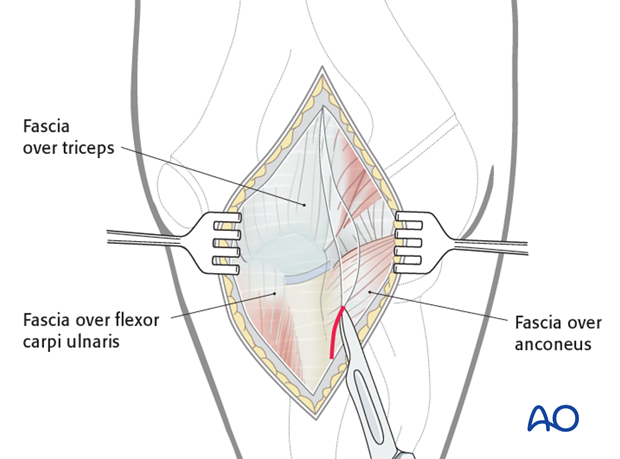
The ulna is exposed through a posterior approach.
An alternative is the posterolateral approach, which provides access to both the proximal ulna and the radial head. A disadvantage of this approach is the potential for cross-union.
If there is residual displacement of the radial neck fracture after optimization of the ulnar correction, a closed reduction using ESIN or an open reduction should be performed.
Open reduction may also be necessary if an image intensifier is not available or if soft-tissue structures are trapped between the fragments.
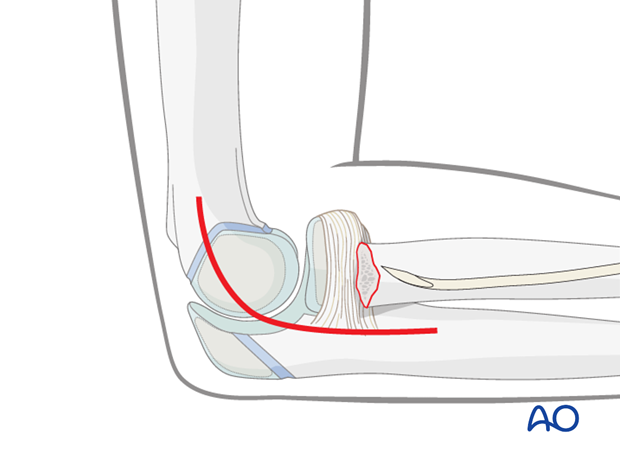
A lateral approach centered on the epicondyle may be used to visualize the radial neck fracture.
5. Reduction and fixation of the ulna
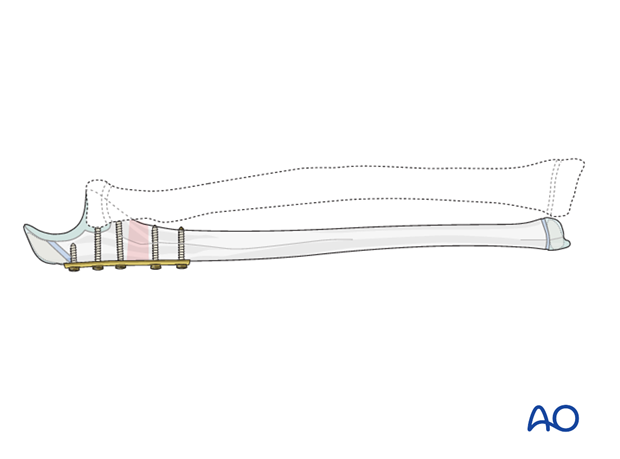
The proximal ulnar fracture should be reduced and stabilized anatomically. The type of plate fixation depends on the fracture pattern.
Ensure that the ulna is out to length and rotationally aligned. With Monteggia equivalents an overreduction of the ulna is not required.
6. Reduction and fixation of radial head/neck
Entry points to the radius
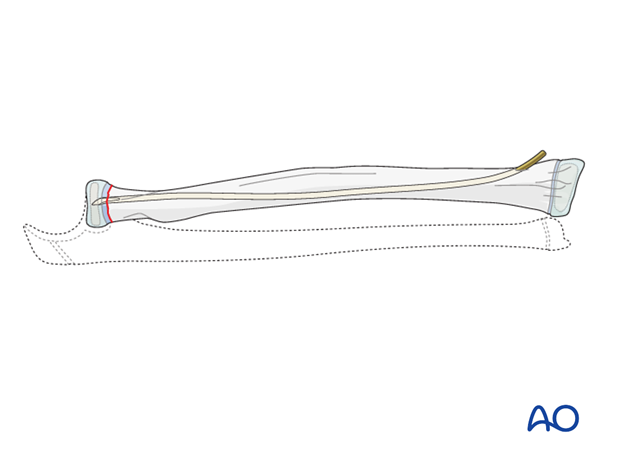
The distal lateral entry point is in common use and shown in this example.
The dorsal entry point (Lister’s tubercle) is also well established and offers more versatile nail manipulation.
Find more details in ESIN entry points (radius).

ESIN procedure
The steps required for proximal radial fracture fixation are described in the ESIN procedure, illustrated with a 21r-E/1.1 fracture.
This technique is also appropriate for reduction and fixation of other proximal radial fracture types.
7. Final assessment
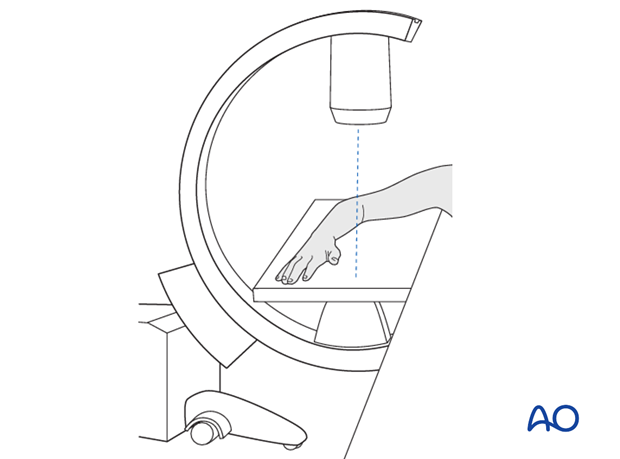
Check the completed osteosynthesis with image intensification. These images should be retained for documentation.
If an image intensifier is not available an x-ray should be obtained before discharge.
Make sure that the plate is at the correct location, the screws and the nail are of appropriate length and the desired reduction has been achieved.
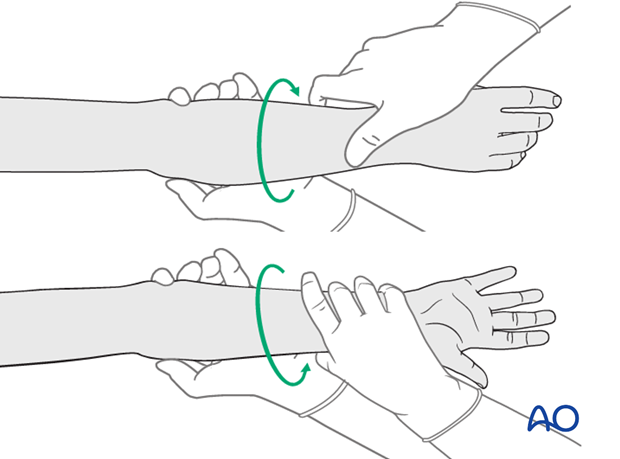
Check the forearm rotation.
8. Aftercare following plating and ESIN
Immediate postoperative care
Whilst the child remains in bed, the elbow and forearm should be elevated on pillows to reduce swelling and pain.

Cast or splint immobilization
If the radial head is fixed with ESIN supplementary casting or splinting is not required.
Analgesia
Ibuprofen and paracetamol should be administered regularly during the first 24-48 hours after surgery, with opiate analgesia for breakthrough pain.
Opiates should not be necessary after 48 hours and regular ibuprofen and paracetamol should be sufficient until 4-5 days after injury or surgery.
The child should be examined if the level of pain is increasing or prolonged analgesia is needed.
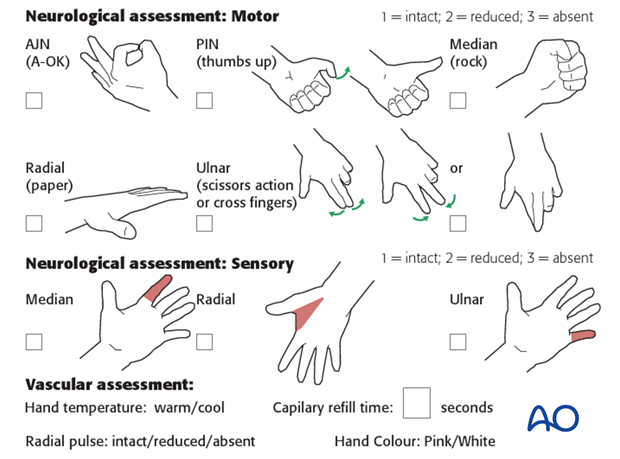
Neurovascular examination
The child should be examined regularly, to ensure finger range of motion is comfortable and adequate.
Neurological and vascular examination should also be performed.
Compartment syndrome should be considered in the presence of increasing pain, especially pain on passive stretching of muscles, decreasing range of active finger motion or deteriorating neurovascular signs, which is a late phenomenon.
See also the additional material on complications and postoperative infections.
Compartment syndrome
Compartment syndrome is a possible early postoperative complication that may be difficult to diagnose in younger children.
The presence of full passive or active finger extension, without discomfort, excludes muscle compartment ischemia.
If there are signs of a compartment syndrome:
- Remove or split constrictive dressings or casts.
- Elevate the limb.
- Encourage active finger movement.
- Reexamine the child after 30 min.
If a definitive diagnosis of compartment syndrome is made, then a fasciotomy should be performed without delay.

Discharge care
Discharge from hospital follows local practice and is usually possible after 1-3 days.
The parent/carer should be taught how to assess the limb.
They should also be advised to return if there is increased pain or decreased range of finger movement.
It is important to provide parents with the following additional information:
- The warning signs of compartment syndrome, circulatory problems and neurological deterioration
- Hospital telephone number
- Information brochure
For the first few days, the elbow and forearm can be elevated on a pillow, until swelling decreases and comfort returns.
The arm can be placed in a sling for a few days until the patient is pain free. Many children are more comfortable without support.
Mobilization
Early movement of the elbow and forearm should be encouraged as soon as the patient is pain free.
Formal physiotherapy is normally not indicated, but children should have a sheet of exercises to stimulate mobilization. See also the additional material on elbow stiffness.
Follow-up
The first clinical and radiological follow-up is usually undertaken 2-3 weeks postoperatively.
At this point, the child should be able to move the elbow with only slight restriction.
AP and lateral x-rays are required.
See also the additional material on complications and healing times.
Plate removal
Plate removal is delayed until function has fully recovered and can be performed as a day case, under general anesthesia.
Incise or excise the old scar. Incise the bursal tissue and remove the screws and plate. Close the wound in layers.
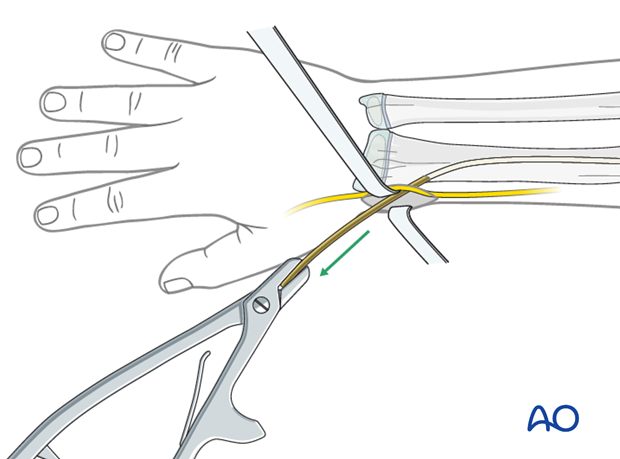
Nail removal
Nail removal is delayed until the fracture has modelled completely and can be performed as a day case, under general anesthesia.
The nail end may slip under tendons and nerves. This may irritate the soft tissues and make it difficult to palpate the nail tip.
Exposure of the nail end should be performed under direct vision with small retractors.
In most cases, a small bursa forms over the nail tip. Once this bursa is opened, the end of the nail can be seen.
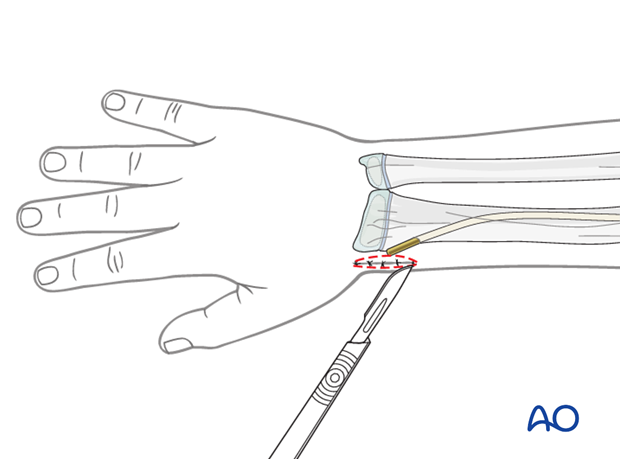
The nail can be removed with the extraction pliers, or a similar clamp. A strong needle holder is also useful.