External fixation
1. General considerations
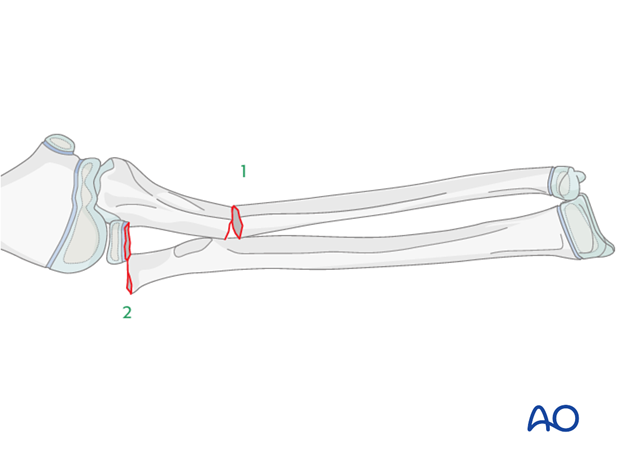
Reduction and fixation of the ulnar shaft fracture
The ulnar fracture should be addressed first. The ulna must be brought out to length to assist with reduction of the radius.
Overcorrection of the ulna may be necessary to stabilize the radial neck fracture.
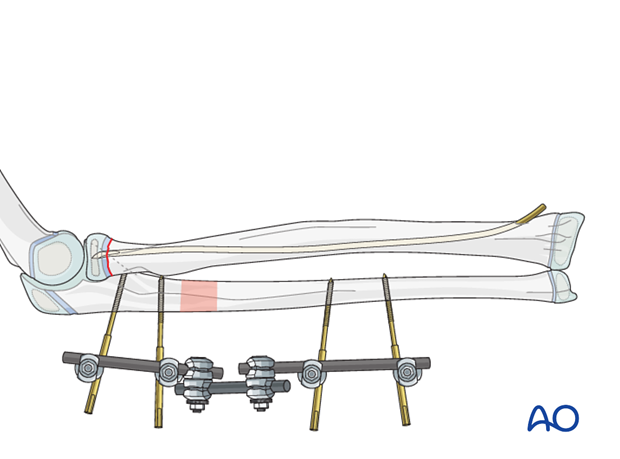
An external fixator is a versatile device in this situation and allows multidirectional correction.
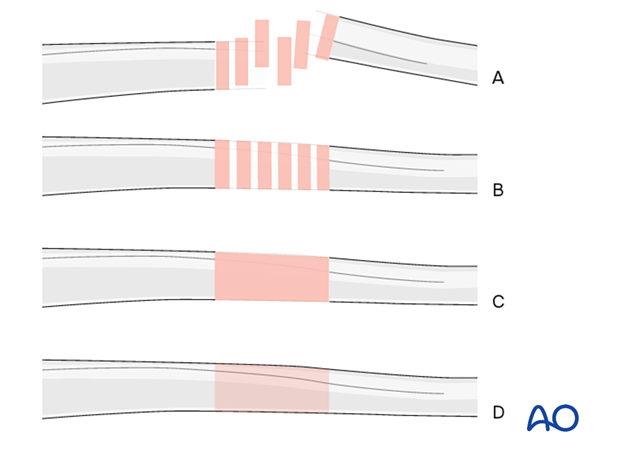
Throughout this section generic fracture patterns are illustrated as:
- Unreduced
- Reduced
- Reduced and provisionally stabilized
- Definitively stabilized
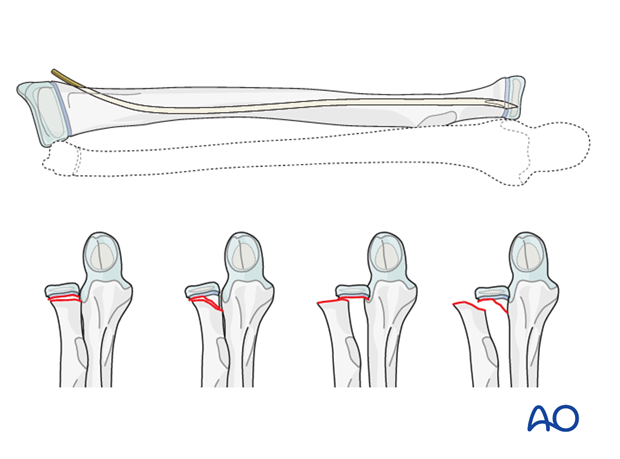
Reduction and fixation of radial head/neck
The techniques required for proximal radial fracture fixation are described in the ESIN procedure for each fracture type:
2. Principles of modular external fixation
Modular external fixator
The versatility of a modular external fixator is an advantage in the management of children’s fractures and can accommodate age specific variations in fracture biology and anatomy.
An external fixator may be used for definitive management of forearm fractures in children due to the short healing time.
Practical considerations are illustrated in detail in the Basic technique for application of modular external fixator in children.
Specific considerations for the forearm shaft are given below.
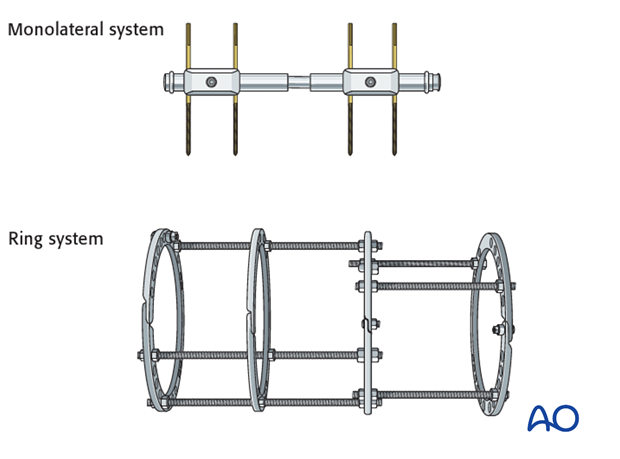
Other types of external fixator
Alterative configurations are available and include monolateral or ring systems.
Disadvantages of these systems in children include:
- Fixed distance of pin insertion defined by the clamp
- Excessively stiff construct
Pin size in forearm fractures
External fixation is suitable for all ages, but the pin diameter must be appropriate to the size of the bone.
Pins with a thread diameter of 2.5-4.0 mm are suitable for forearm fractures and should be about 1/3 of the bone diameter.
Sequence of pin insertion
Determined by:
- Fracture morphology
- Personal preference
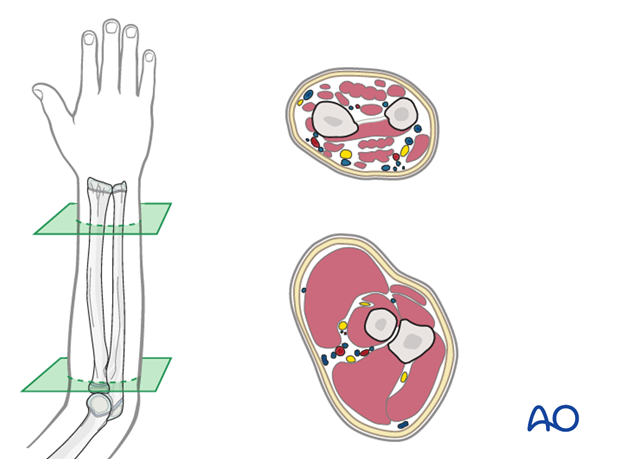
Safe zones for pin placement
The forearm anatomy is complex due to the presence of three major neurovascular bundles. Pin placement should avoid these structures.
Read more about Safe zones for pin placement in the ulna.
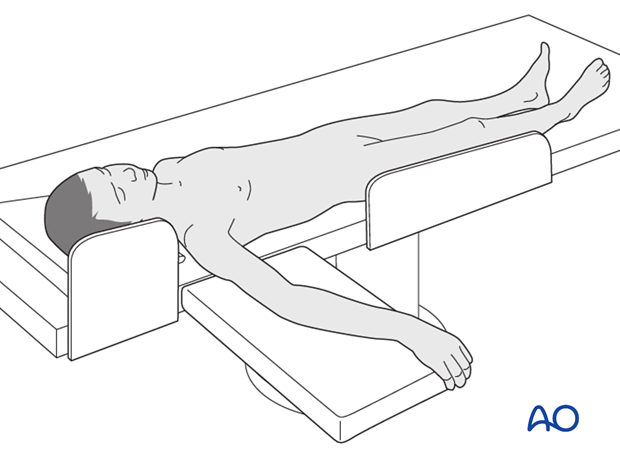
3. Patient preparation
This procedure is normally performed with the patient in a supine position.
4. Frame construction on the ulna
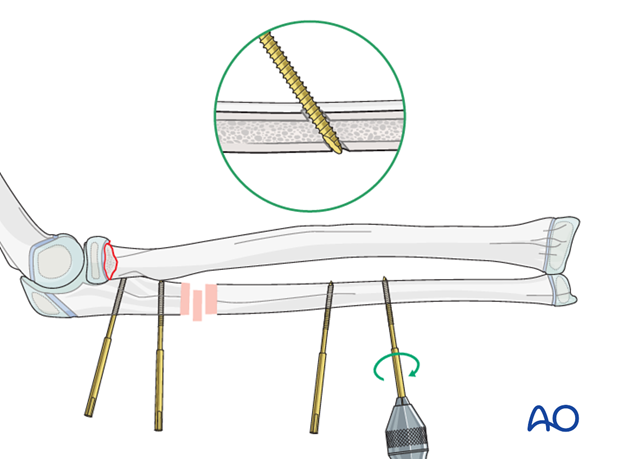
Proximal pin insertion
Insert the proximal ulnar pins through the subcutaneous cortex of the posterior border of the ulna between the extensor and flexor muscle masses.
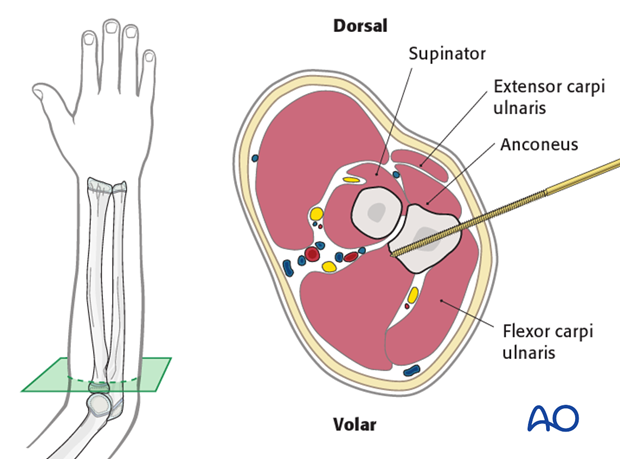
Make an 8-10 mm skin incision over the site of pin insertion.
Use an artery clip for blunt dissection down to the bone, protecting important anatomical structures.
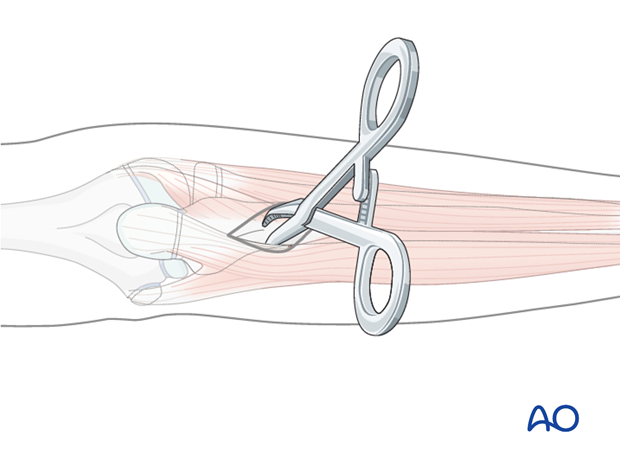
The posterior border of the ulna is subcutaneous and offers the best access.
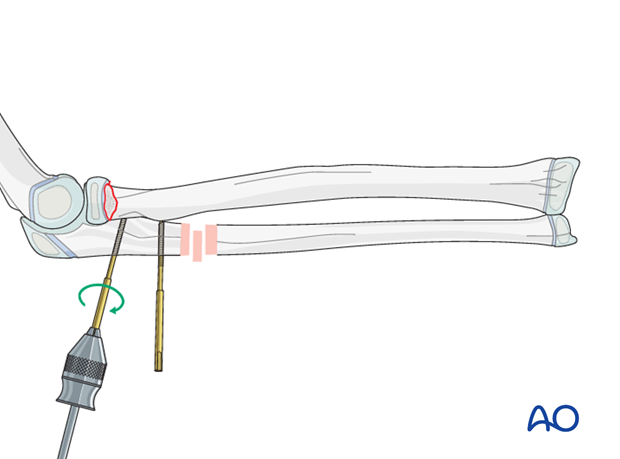
Insert the pin in the near cortex and through the center of the bone into the far cortex.
Take care not to advance the tip of the pin beyond the far cortex to avoid damage to neurovascular structures.
Pins should not be placed closer than 1 cm to the physis.
Distal pin insertion
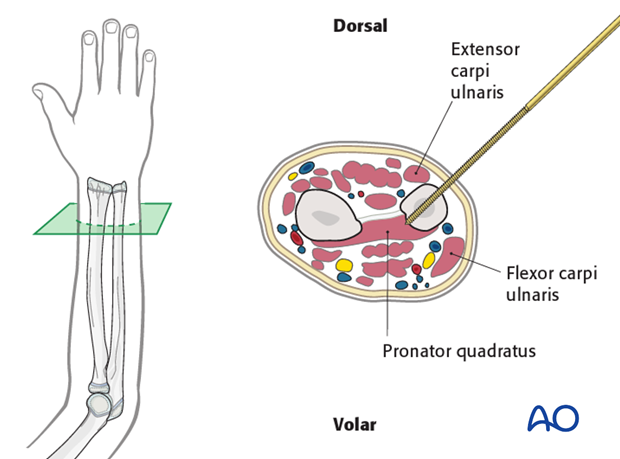
Safe access to the subcutaneous dorsomedial cortex is improved with the elbow flexed and the forearm in mid-supination.
Make an 8-10 mm skin incision over the site of pin insertion.
Use an artery clip for blunt dissection down to the bone, protecting important anatomical structures.
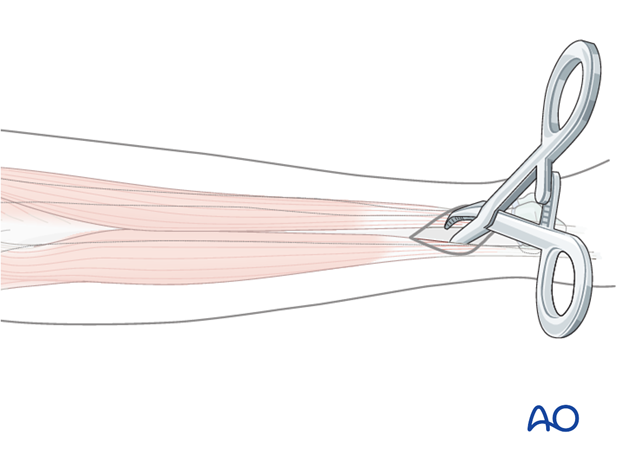
Insert the distal ulnar pins from dorsomedially between the extensor carpi ulnaris and flexor carpi ulnaris.
As the distal ulna in children has a small diameter, oblique pin placement improves bony contact.
Pins should not be placed within 1 cm of the physis.
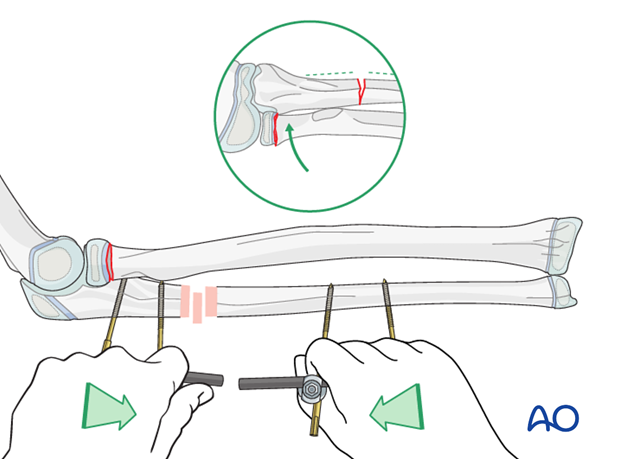
Reduction of ulnar and radial neck fracture
Manually reduce the ulnar fracture using the unlinked pin blocks as handles. Some overcorrection may be necessary if the radial fracture does not reduce spontaneously.
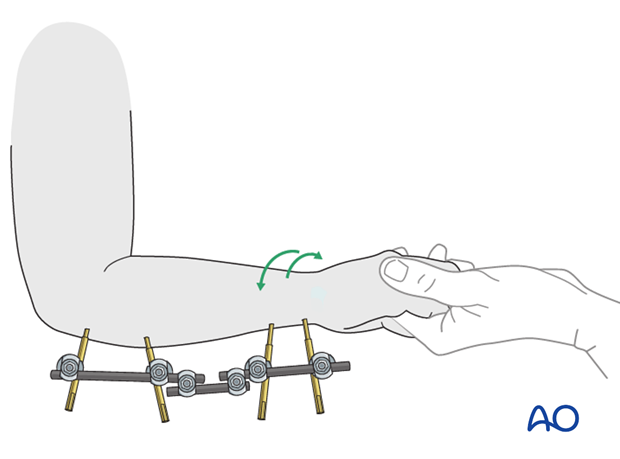
5. Assessment of forearm rotation
Once the fracture is reduced and stabilized, the position may be checked with an image intensifier.
The rotation of the forearm is also assessed clinically. Pronation and supination may be limited by the injury and fixator configuration.
If there is important radiological malalignment or functional restriction, the external fixator may be adjusted.
6. Aftercare following external fixation
Pin-site care
There is no universally agreed protocol for pin site care.
The following points are however recommended:
- Pin site care should continue until removal of the external fixator.
- The pin sites should be kept clean.
- Crusts or exudates should be removed.
- The pins may be cleaned with water, saline, disinfectant solution or alcohol. The frequency of cleaning varies from daily to weekly.
- Ointments or antibiotic solutions are not recommended for routine pin site care.
- Pin sites do not need to be protected whilst showering or bathing with clean water, but should be dried immediately.
Pin site infection
Initial management is with oral anti-staphylococcal antibiotics.
In case of pin loosening or unresponsive pin site infection, the following steps should be taken:
- Remove all involved pins and place new pins in a healthy location.
- Debride the pin sites in the operating theater, using curettage and irrigation.
- Take specimens for microbiological culture to guide appropriate antibiotic treatment.
Internal fixation following an infected external fixator pin has a high risk of infection and should be avoided unless no reasonable alternative is available.
See also the additional material on postoperative infection.
Compartment syndrome
See the additional material on compartment syndrome.
Mobilization
Elevation is useful in the initial stages. A sling is helpful if fixator configuration allows its application.
The patient should be encouraged to move the wrist and elbow, within the limits of comfort.
Follow-up
The patient should be seen 7-10 days after surgery for a wound check.
X-rays are taken to check stability and alignment.
See also the additional material on healing times.












