Closed reduction; K-wire fixation
1. Principles
For extension-type fractures (apex anterior, about 95% of fractures), closed reduction results in good preliminary stability due to intact posterior periosteum.
For flexion-type supracondylar fractures (apex posterior), the reduction and pinning technique may need to be modified, even if the fracture is minimally displaced.
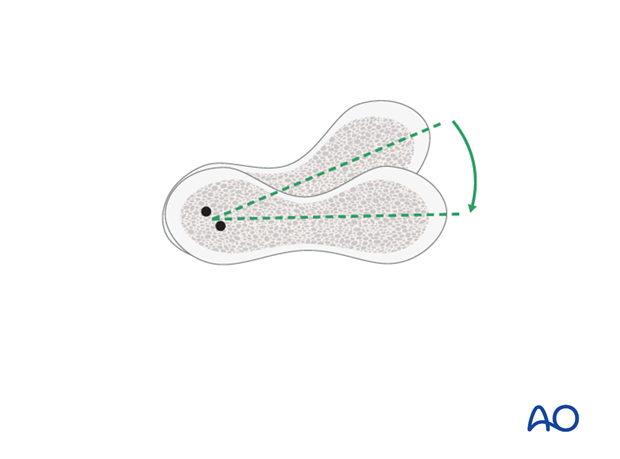
How periosteum can aid in temporary stability after reduction
The intact posterior periosteum confers stability once the fracture is reduced and the elbow is held in maximal possible flexion.
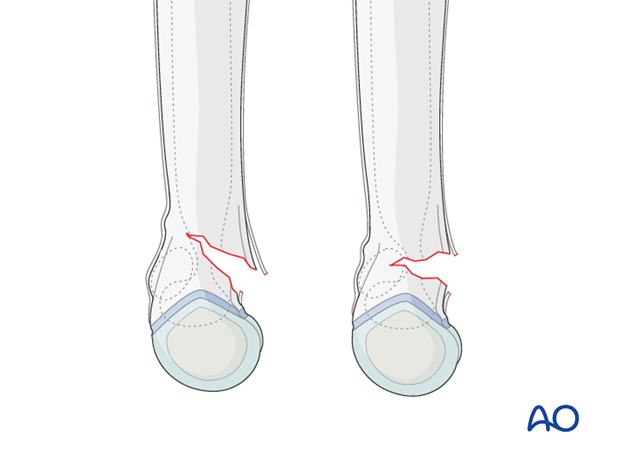
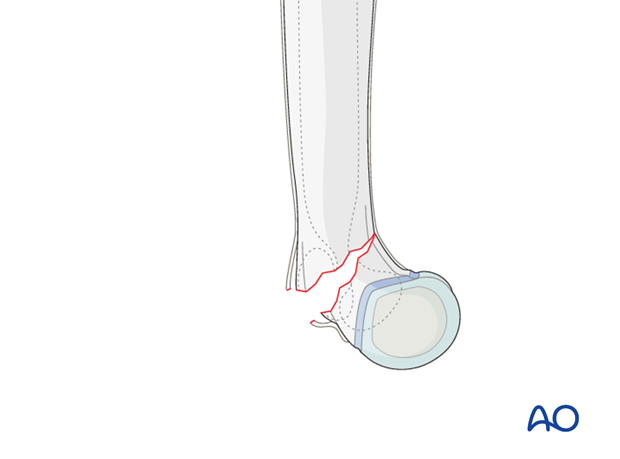
In flexion-type supracondylar fractures (apex posterior) the posterior periosteum is likely to be torn. These occur in around 5% of all supracondylar humeral fractures.
Closed reduction is possible for most of these fractures.
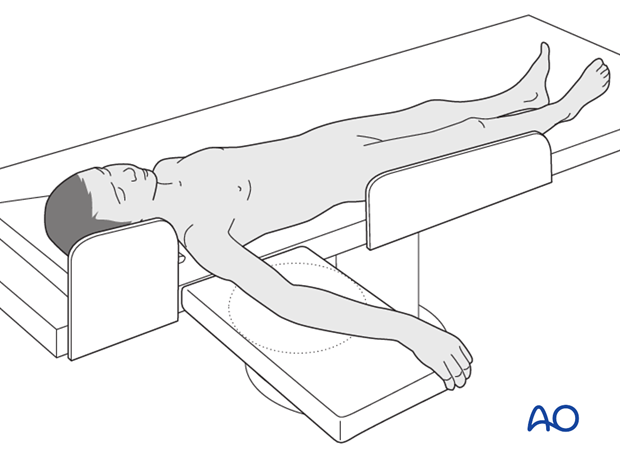
2. Patient preparation
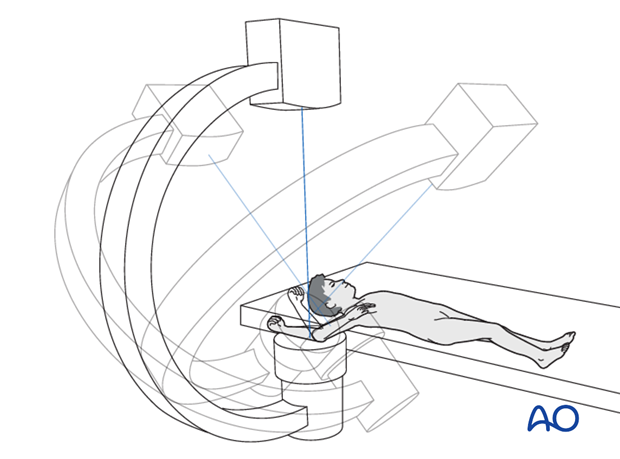
This procedure is normally performed with the patient in a supine position.
3. Closed reduction
Correction of extension type supracondylar fractures
Any incomplete fracture which is oblique in an AP view will have a small component of varus or valgus deformity.
This will correct itself at the same time as the extension angulation and with the following maneuver.
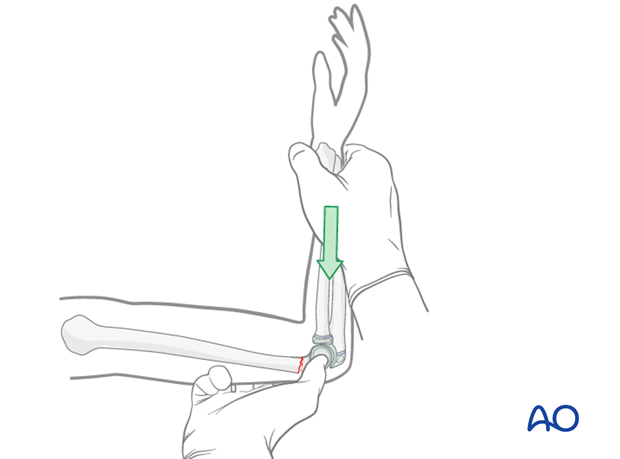
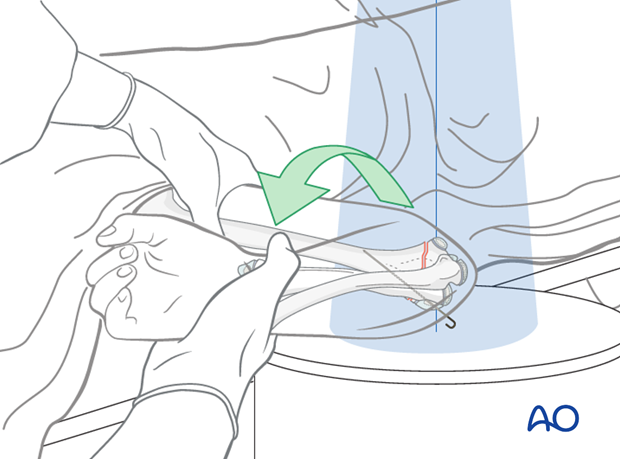
With the elbow extended, a thumb is positioned on the back of the olecranon and pushed distally and anteriorly whilst the elbow is smoothly flexed.
If the elbow will not flex fully it is likely that the reduction is incomplete. A complete reduction may be felt.
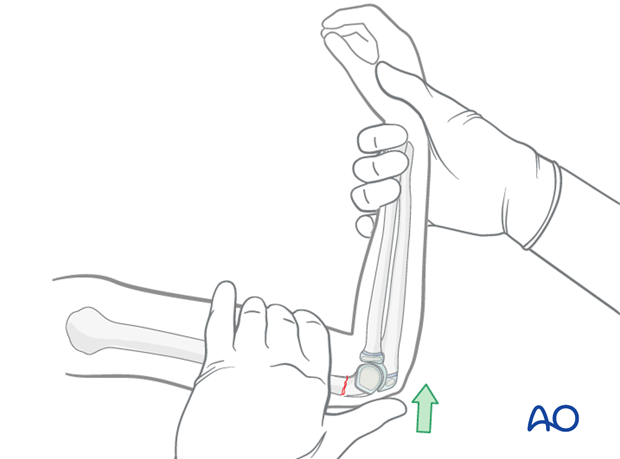
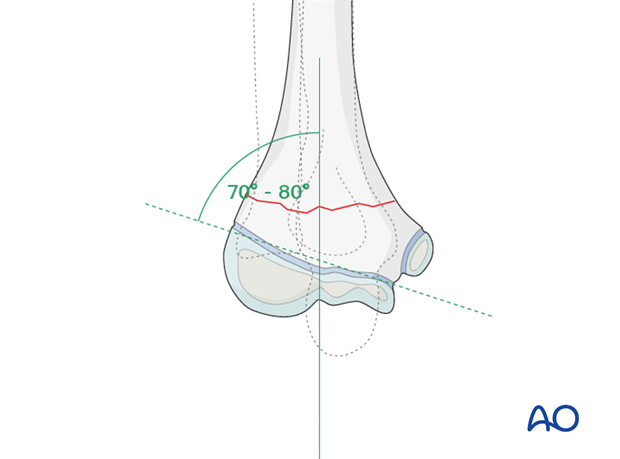
The elbow is maintained in maximal possible flexion and the reduction is verified on an AP image. Baumann's angle should be correct (70-80°) at this stage.
Visually evident varus malposition should not be accepted. The carrying angle should be equal to the opposite arm.
The reduction is also verified on a lateral view taken by externally rotating the entire arm as a unit held with the elbow maximally flexed.
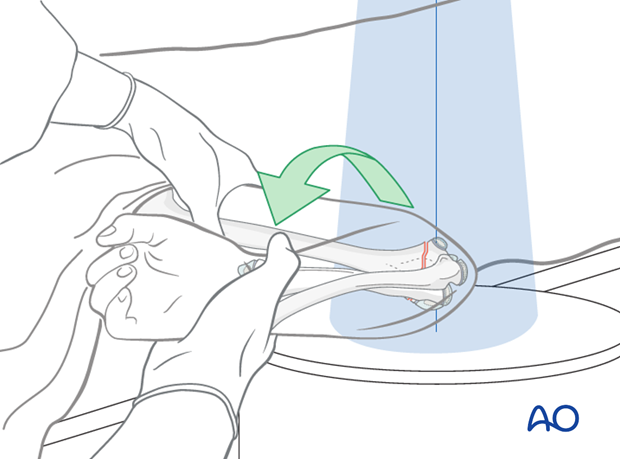
An alternative is not to rotate the arm, but to rotate the C-arm.
Note: Anatomical closed reduction is the objective of this procedure.
See also the additional material on closed reduction of supracondylar fractures.
Correction of flexion type supracondylar fractures
An incomplete flexion type supracondylar fracture can be manipulated by gentle extension of the elbow.
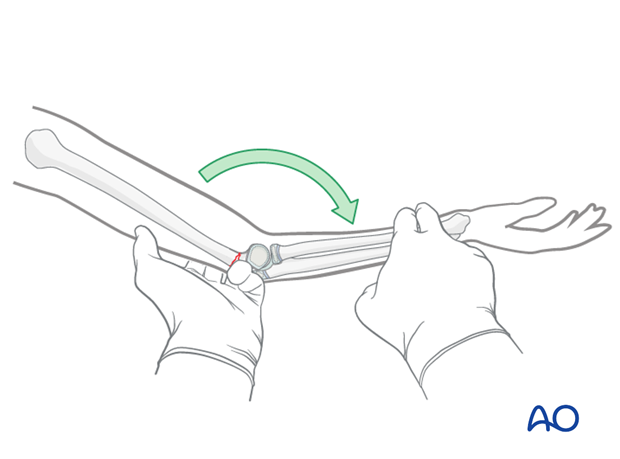
Alternatively, it can be manipulated by posteriorly directed pressure along the axis of the 90° flexed forearm.
These maneuvers should be performed with care in order to avoid completing and displacing the fracture.
If the fracture is inadvertently completed and displaced, it should be treated as either a 13-M/3.1 III or a 13-M/3.1 IV fracture.
4. Fixation
General guidelines for K-wire insertion
2.0 mm K-wires are used for most supracondylar fractures in larger children (usually > 6 years of age).
1.6 mm K-wires may be used for smaller and younger children.
It is preferable to insert all K-wires from the lateral side to avoid the risk of an iatrogenic ulnar nerve injury.
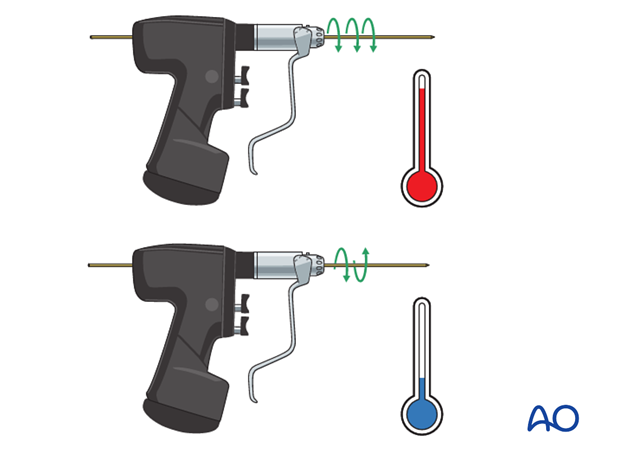
All K-wires should be sharp-pointed. Powered insertion of K-wires generates heat in the tissues: wires should be inserted with a slow-running drill, an oscillating drill, or by hand.
If multiple attempts are made to insert any one pin the bone may be weakened or the physis may be damaged. In general, only two attempts of insertion of any K-wire are permissible.
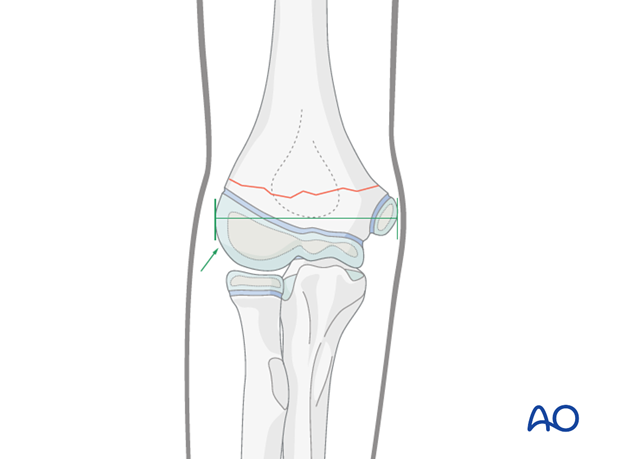
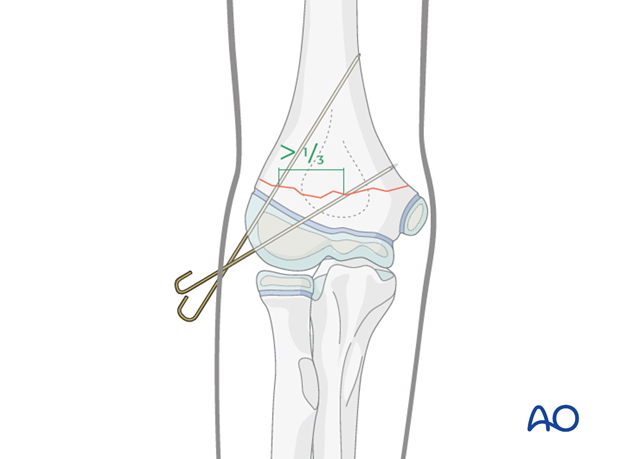
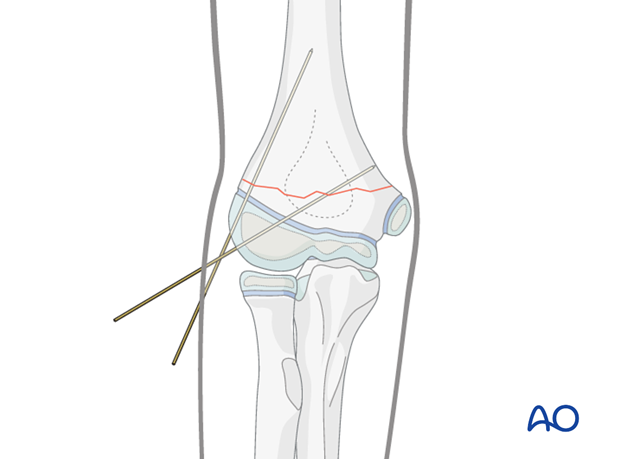
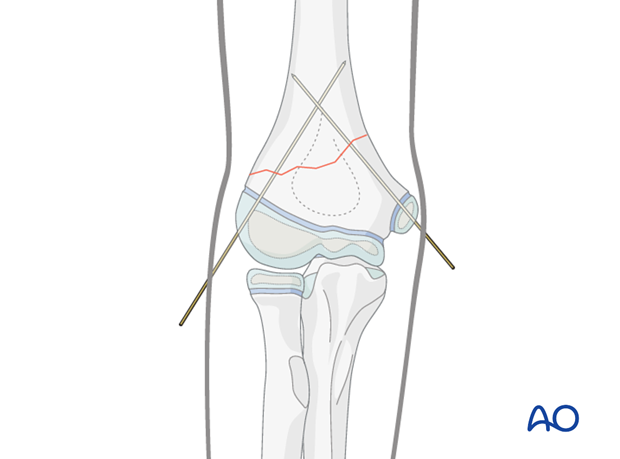
The pins must diverge to provide adequate spread at the fracture site on the AP view.
Adequate spread is obtained if each column contains at least one pin, or if the divergence of the pins exceeds 1/3 of the width of the fracture.
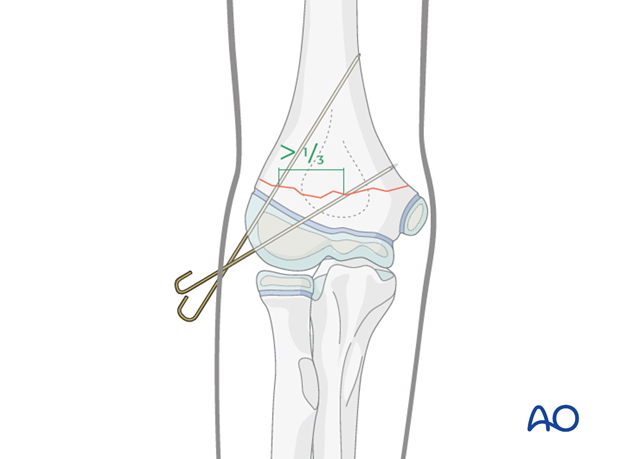
If the spread of laterally inserted pins is inadequate, the fixation will be rotationally unstable.
The tendency, in this case, is for the distal fragment to internally rotate and this allows collapse into varus, resulting in a cosmetically unappealing malunion.
Oblique fractures high on the lateral side
This fracture pattern is anatomically favorable for the insertion of two or three divergent lateral pins. A medial pin would only rarely be required.
The pin insertion is performed as described below for the transverse fracture pattern.
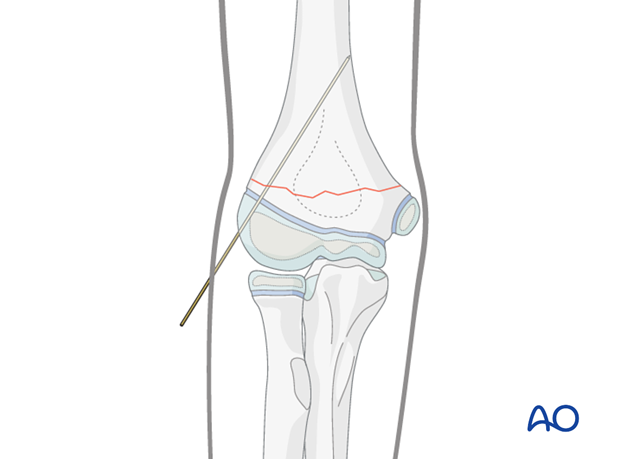
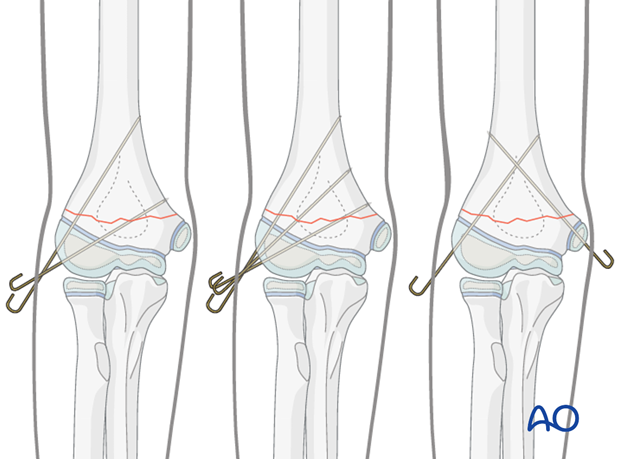
Transverse fractures
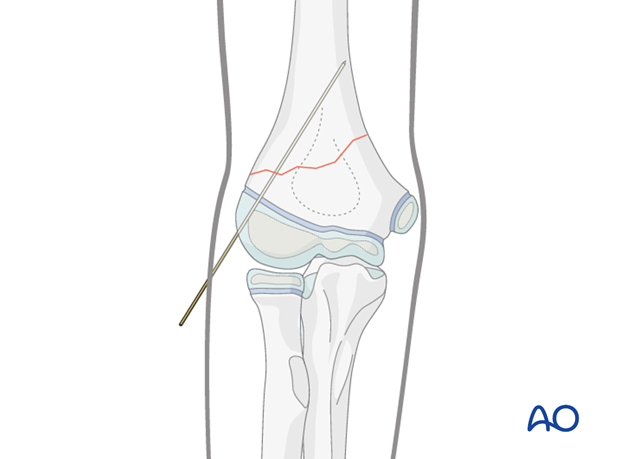
Pin entry points are located in the lateral humeral condyle, distal to its maximal width.
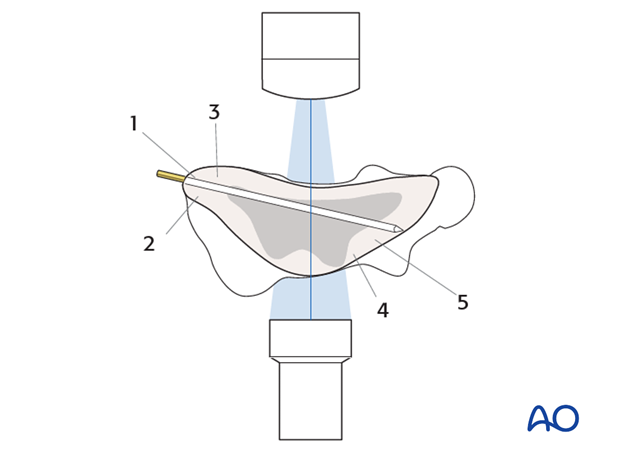
Any intraosseous pin will penetrate the following structures in sequence:
- Epiphyseal cartilage (or ossific center)
- Physis
- Metaphyseal bone of the distal fragment
- Metaphyseal bone of the proximal fragment
- Cortex of the proximal fragment
Note: Tactile feedback during pin insertion is important confirmation of intraosseous position of the pin.
AP image intensifier views are used during K-wire insertion.
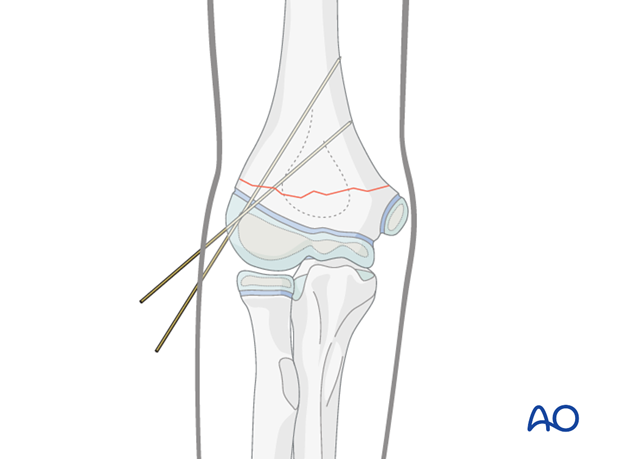
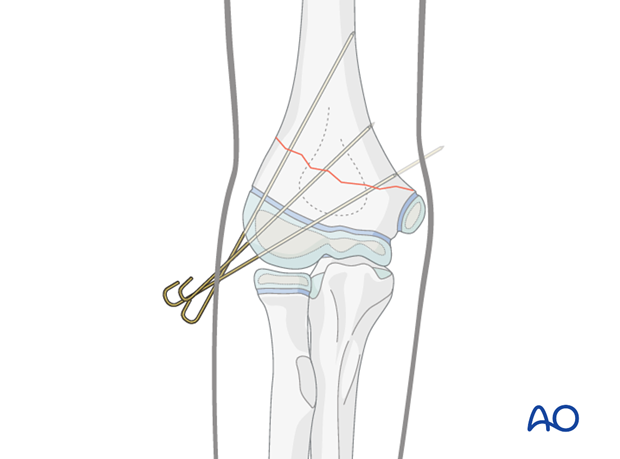
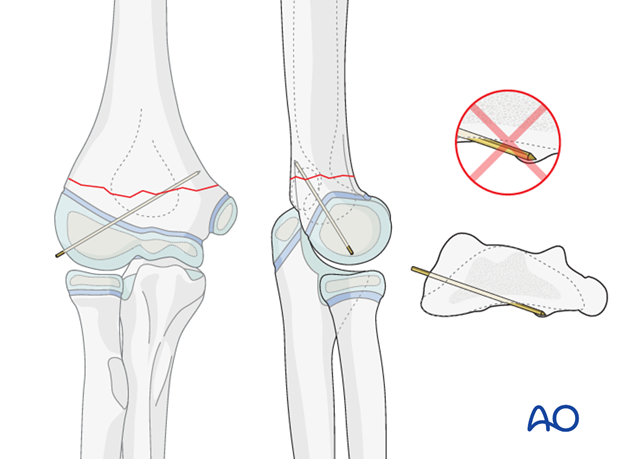
The first K-wire is inserted within the lateral column and should achieve strong purchase in the medial cortex of the proximal fragment. It can either engage, or just penetrate, this cortex.
Engagement of the cortex can be heard as a change in pitch of the K-wire driver and can be felt by the surgeon inserting the K-wire. If inserted by hand, the increased resistance is felt as the tip of the pin starts to gain purchase in the medial cortex.
Passage through other dense bony structures, eg, olecranon fossa cortex, may also be felt.
The surgeon should pay attention to correspondence between feedback from the K-wire driver (or T-handle) and what is seen on the image intensifier.
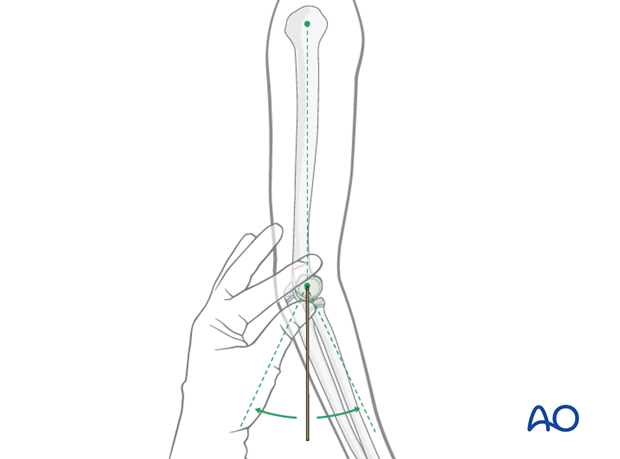
The position of the first K-wire is confirmed on both AP and lateral views, the latter by gently externally rotating the arm as a unit.
If the inserted pin prevents positioning of the arm in a true lateral view, either the pin can be cut short or the image intensifier rotated rather than the arm.
Techniques to assist correct insertion of the pin within the sagittal plane (lateral view) include:
- Identifying the alignment of the humeral shaft when evaluating the reduction and marking the sagittal alignment on the skin
- Palpation of the humeral head aiming the pin for its center
The second K-wire is inserted from the lateral side into the medial column through the capitellar secondary ossification center.
The pin spread at the fracture site should be more than 1/3 of the bone diameter.
The AP image can be used as a guide for aiming.
Care must be taken to ensure that the K-wire achieves purchase in the proximal fragment.
The audible and tactile feedback from the K-wire driver must be used because it is possible to miss the proximal fragment anteriorly…
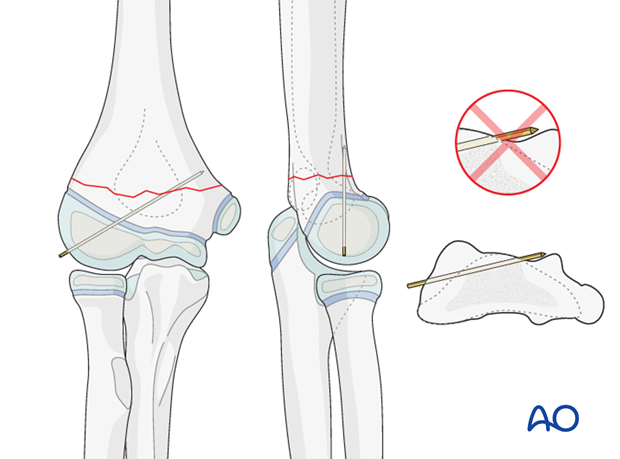
…or posteriorly and not notice on the lateral image.
Following insertion of the second K-wire, AP, lateral, and column (45° internal and 45° external) views are obtained.
K-wire position must be adjusted if necessary.
If the reduction and fixation are satisfactory, lateral real-time image intensification, with flexion and extension of the elbow, can be used to confirm fixation stability.
It is unusual to require a third K-wire.
However, if K-wire spread is inadequate in the AP view, or if the fixation is deemed insufficiently stable, then a third pin should be inserted at this point. Care must be taken to avoid skin tension.

Oblique fractures high on the medial side
The technique of medial K-wire insertion described below should be followed whenever at the surgeon's discretion medial intraosseous wiring is performed.
This fracture pattern is anatomically unfavorable for pinning from the lateral side alone. It may not be possible to achieve adequate fixation of both columns, or adequate pin spread, with lateral pins alone. In this case, the addition of a medial pin may be necessary.
The first lateral pin is inserted as described above.
Pitfall: Iatrogenic injury to the ulnar nerve occurs in up to 6% of medial pinnings .
( Howard A, Melpuri K, Abel MF, et al. The treatment of pediatric supracondylar humerus fractures - Evidence based guideline and evidence support. North River road: AAOS; 2011.)
In many children, the ulnar nerve can sublux forwards onto, or anterior to, the medial epicondyle with elbow flexion.
This may be easier to demonstrate on the contralateral, uninjured elbow and is difficult to appreciate in a swollen and injured limb.
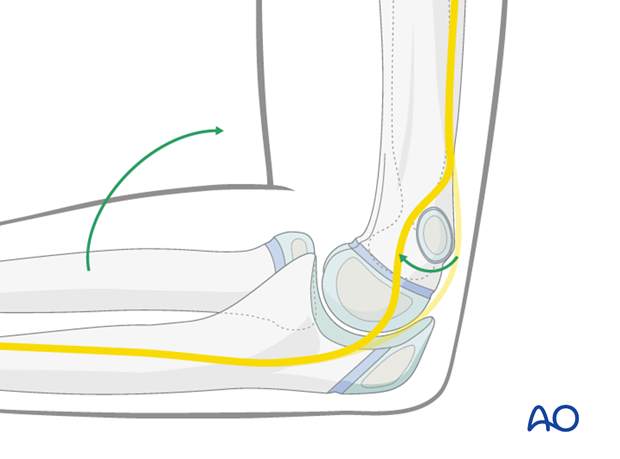
To minimize risk to the ulnar nerve, the medial pin is inserted with the arm in the position in which it will be immobilized (around 45° flexion) and a limited open technique is used to guard the ulnar nerve.
The medial epicondyle is palpated (this can be difficult in a swollen elbow).
A 1 cm longitudinal skin incision is made directly over the prominence of the medial epicondyle.
Blunt dissection is performed, until the medial epicondyle can be palpated and seen.
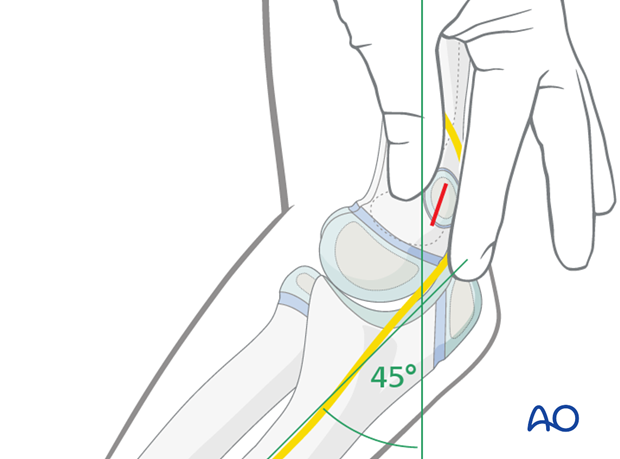
A 2.0 mm drill guide, placed directly onto the epicondyle, is used to establish the entry point of the K-wire.
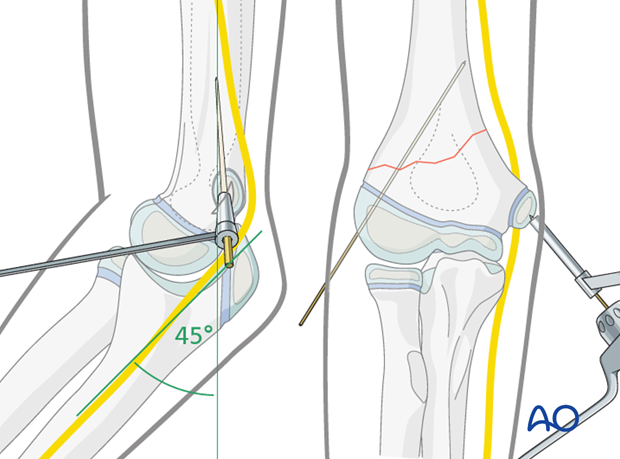
The K-wire is inserted through the medial epicondyle and across the fracture, within the medial column.
Attention should be paid to the audible and tactile feedback from the K-wire driver as the K-wire engages the lateral cortex of the proximal fragment.
Following insertion of the medial K-wire, AP, lateral, and column views (45° internal and 45° external) are obtained.
K-wire position must be adjusted if necessary.
If the reduction and fixation are satisfactory, lateral real-time image intensification, with flexion and extension of the elbow, can be used to confirm fixation stability.
Note
Most stable pin configurations will use two or three lateral entry pins.
Occasionally a medially inserted pin may be required.
Image intensification is used to confirm that the reduction and pin fixation are satisfactory and that the construct is stable.
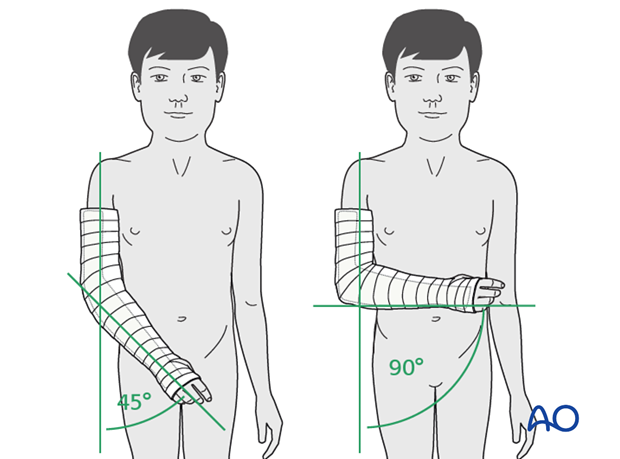
5. Immobilization
The arm is protected with a posterior plaster splint, applied at 45°–90° of flexion, depending on local protocol, for approximately three weeks.
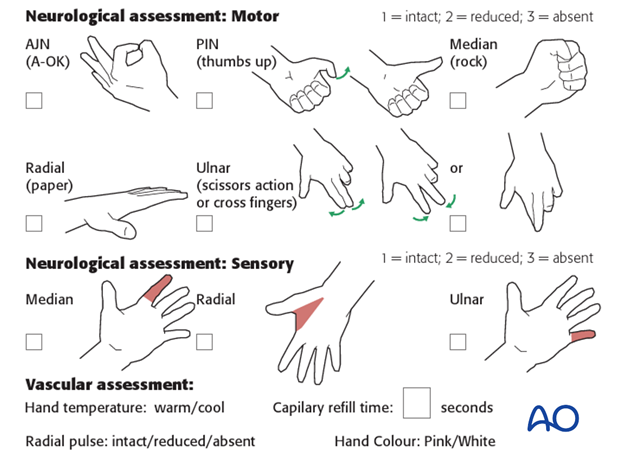
Neurological and vascular function is checked postoperatively.
Pins are usually removed in the clinic 3–4 weeks after insertion.
For the first few days, the elbow and forearm can be elevated on a pillow, until swelling decreases and comfort returns.
At this point, the child may choose to use a sling to support the arm. Many children are more comfortable without a sling.

6. Aftercare
Supracondylar humeral fractures heal rapidly and often within 3–5 weeks.
Analgesia, including ibuprofen and paracetamol, should be administered regularly.
Compartment syndrome
Compartment syndrome is a possible early postoperative complication that may be difficult to diagnose in younger children.
The child should be examined frequently, to ensure finger range of motion is comfortable and adequate.
Neurological and vascular examination should also be performed.
Increasing pain, decreasing range of finger motion, or deteriorating neurovascular signs should prompt consideration of compartment syndrome.
See also the additional material on postoperative infections.
Discharge care
When the child is discharged from the hospital, the parent/caregiver should be taught how to assess the limb.
They should also be advised to return if there is increased pain or decreased range of finger motion.
It is important to provide parents with the following additional information:
- The warning signs of compartment syndrome, circulatory problems and neurological deterioration
- Hospital telephone number
- Information brochure
Follow-up x-rays
Control x-rays may be taken at one week following injury to assess fracture position. Further x-rays may be necessary at three weeks to assess fracture healing. This should be performed after the splint has been removed.
Removal of cast or splint
Splints or casts are usually removed 3 weeks of the injury.
K-wire removal
Protruding K-wires can be removed in the clinic, without anesthesia.
A simple sling can be provided for comfort.
Recovery of motion
As symptoms recover, the child should be encouraged to remove the sling and begin active movements of the elbow.
The majority of elbow motion is recovered rapidly, usually within two months of splint removal. The older child may take a little longer.
Once the child is comfortable, with a nearly complete range of motion, he/she may resume noncontact sports incrementally. Resumption of unrestricted physical activity is a matter of judgment for the treating surgeon.













