Closed reduction; K-wire fixation
1. Introduction
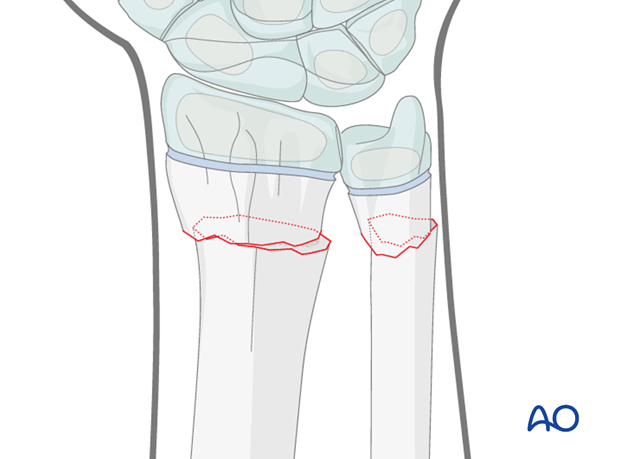
These fractures are usually posteriorly angulated (apex anterior) and can generally be reduced closed, ideally under general anesthesia. Impediments to reduction are interposed periosteum and pronator quadratus.
Fractures with an intact dorsal periosteum are stable after reduction and may not require wire fixation. K-wire stabilization may be strongly indicated in some cases.
Anteriorly angulated (apex posterior) fractures are less common and are also generally reduced closed. Impediments to reduction are the extensor tendons.
2. Patient preparation
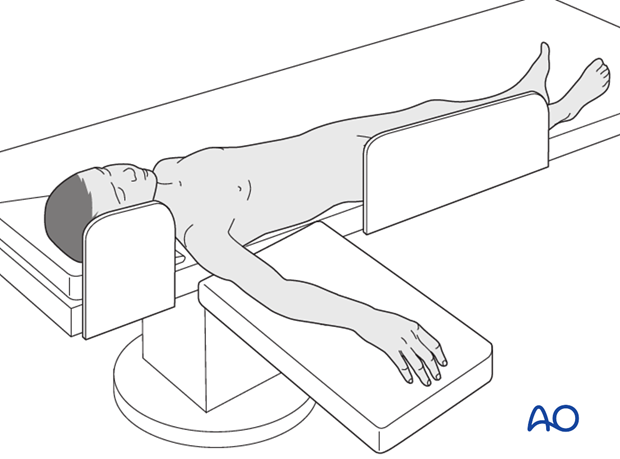
This procedure is normally performed with the patient in a supine position.
3. Anatomy of the distal forearm
A thorough knowledge of the anatomy of the wrist is essential.
The additional material gives a short introduction.

4. Reduction
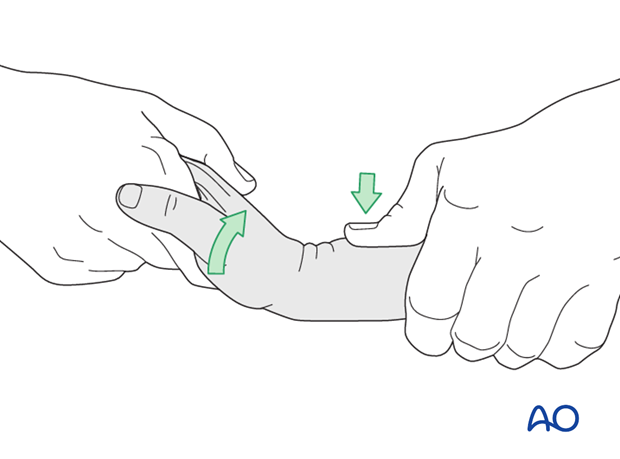
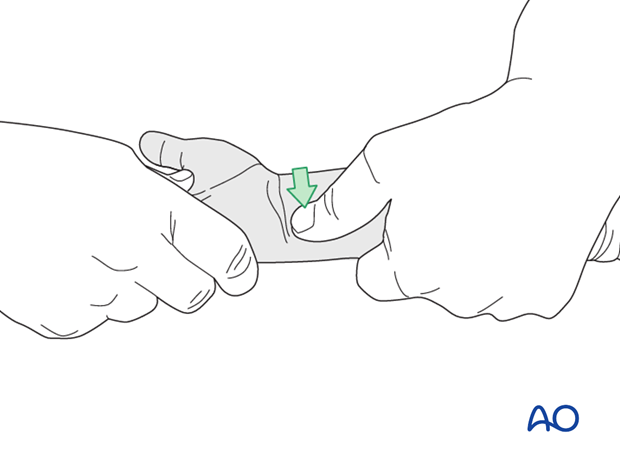
Indirect reduction of partially displaced fractures
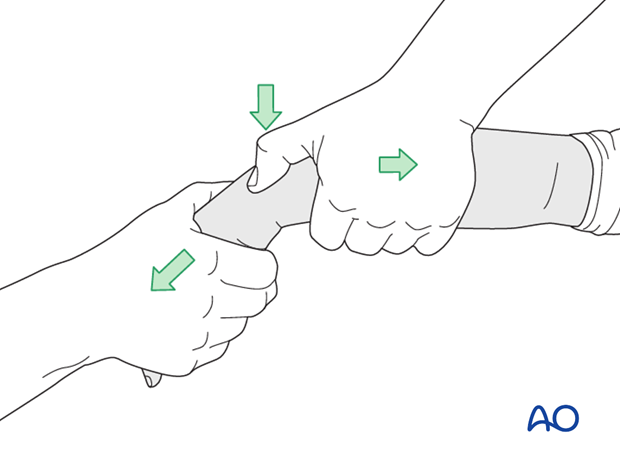
The reduction maneuver for posteriorly angulated fractures, together with some posterior translation (common) is by traction and direct pressure over the epiphysis, followed by palmar flexion.
Ideally, the reduction is verified with image intensification and any residual malalignment is corrected with direct pressure.
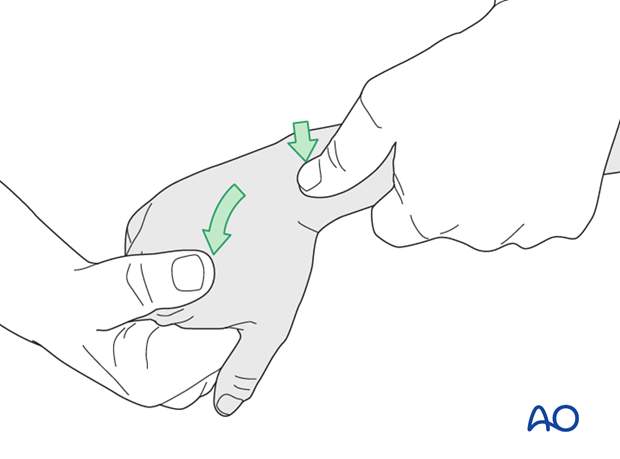
The reduction maneuver for anteriorly angulated fractures, together with some anterior translation (uncommon) is by traction and direct pressure over the epiphysis, followed by dorsiflexion.
Ideally, the reduction is verified using image intensification and any residual malalignment is corrected with direct pressure.
Indirect reduction of completely displaced fractures
For completely displaced fractures, the dorsal periosteum will act as a tension band and impede longitudinal traction.
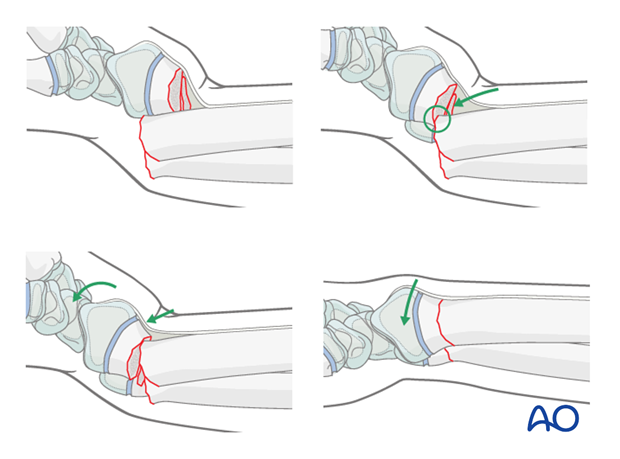
It is necessary to hyperextend the distal fragment, relaxing the posterior periosteum.
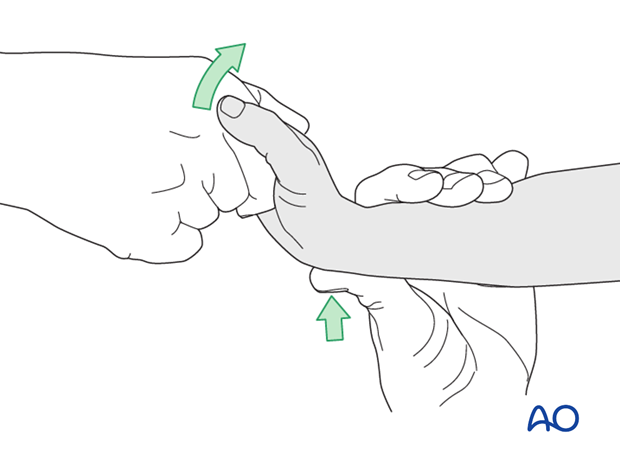
This is followed by direct thumb pressure to hitch the fragments.
At this point palmar flexion of the wrist will reduce the fracture.
Ideally, the reduction is verified using image intensification and any residual malalignment is corrected with direct pressure.
Once the radius is reduced, the ulna will usually also reduce.
Ideally, this should be confirmed using image intensification.
In case of persistent malreduction of the ulna, direct pressure on either the posterior…
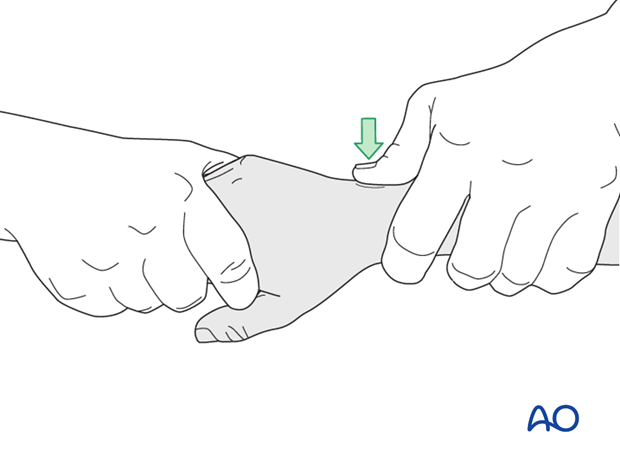
…or anterior surface should produce an anatomical reduction.
Reduction is often more straightforward than single bone fractures, and may not require K-wire fixation, if it is stable. Relaxing the manual reduction pressure, will determine whether it is stable, as an unstable reduction will redisplace.
See:
- Zamzam MM, Khoshhal KI. Displaced fracture of the distal radius in children: factors responsible for redisplacement after closed reduction. J Bone Joint Surg Br. 2005 Jun;87(6):841-843.
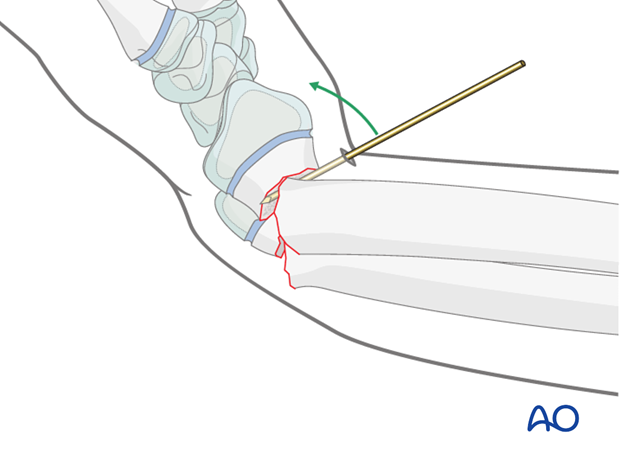
Direct reduction using K-wire
For irreducible fractures, a percutaneous K-wire can be inserted (through a stab incision) into the fracture site and used as a lever to facilitate reduction of either bone.
5. K-wire fixation
General considerations
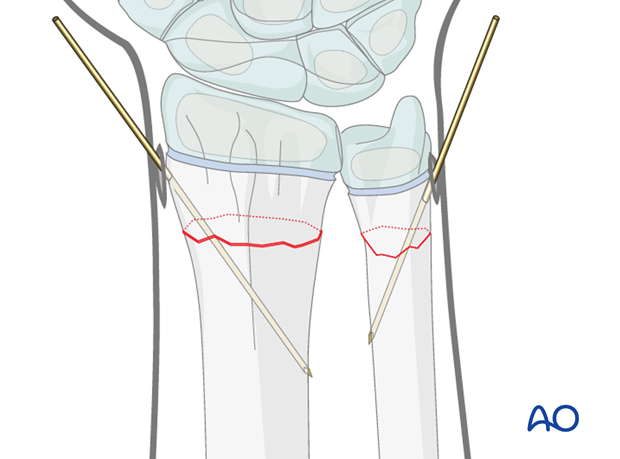
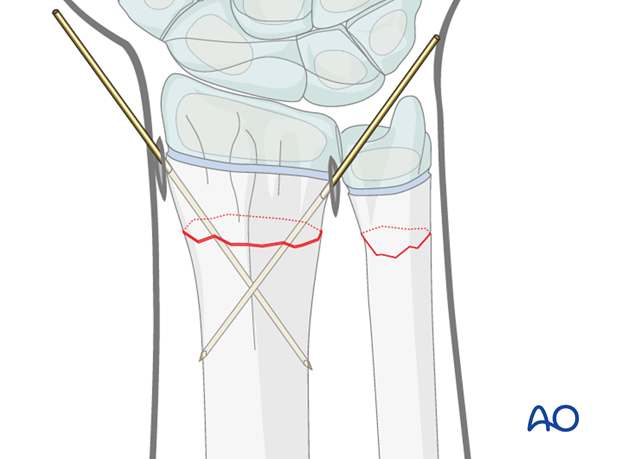
For fractures that are unstable after reduction, single, or crossed, K-wires are normally sufficient to stabilize the fracture.
Occasionally a further wire is used to stabilize the ulna.
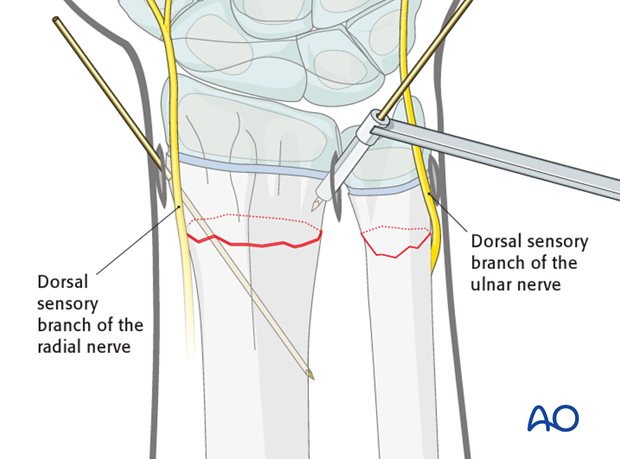
Approaches
A small skin incision is made.
The incision is deepened to the bone using a blunt artery forceps and a protective sleeve is inserted.
Care should be taken to avoid the dorsal sensory branch of the radial nerve and the dorsal sensory branch of the ulnar nerve.
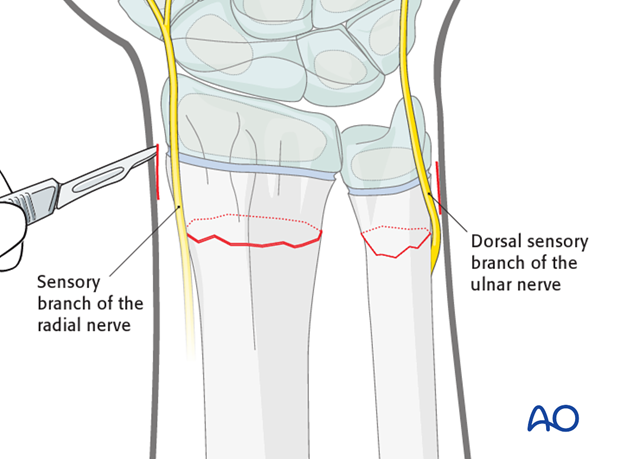
For a posteriomedially inserted second wire, a mini-open approach is used and a guide is required to protect the posterior soft tissues, particularly the extensor tendons.
K-wire insertion
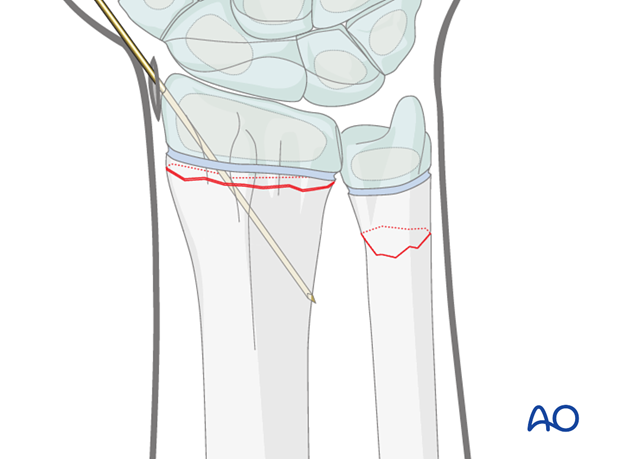
A single, or two crossed, smooth 1.6 mm K-wires are inserted through the radial metaphysis, avoiding the growth plate and the perichondrial ring.
The wires should be inserted with an oscillating drill and cooled with saline solution to prevent thermal injury.
The wires may also be inserted by hand using a T-handle.
Ideally, wires are inserted using image intensification control, in order to check the trajectory of the wire and to ensure engagement of the far cortex without penetration of the soft tissues.
Pearl: For more distal fractures, it is occasionally necessary to insert antegrade wires engaging the distal radial metaphyseal flare.
The insertion incisions should be deepened to bone by spreading the tissues using a blunt artery forceps. The wires should be passed through protective guides.
Care should be taken that the wires do not damage the perichondrial ring of the physis .
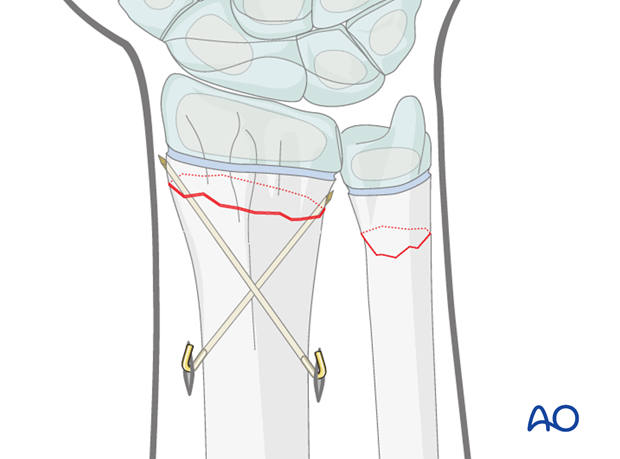
An alternative in more distal radial fractures is to insert the wire through the radial styloid and across the radial physis. If this is undertaken, it is especially important to avoid thermal injury.
Occasionally a second wire is used to stabilize the ulna.
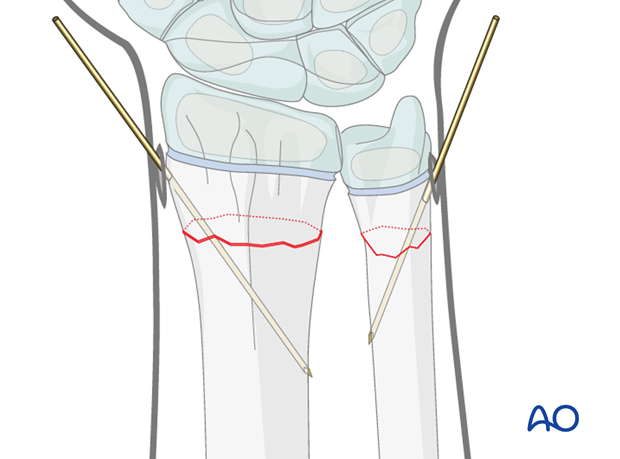
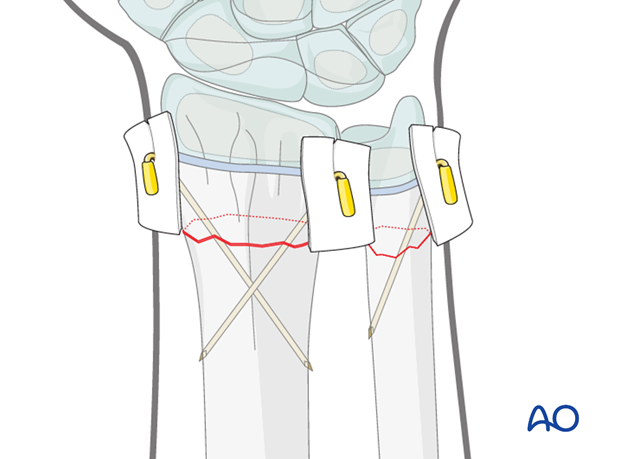
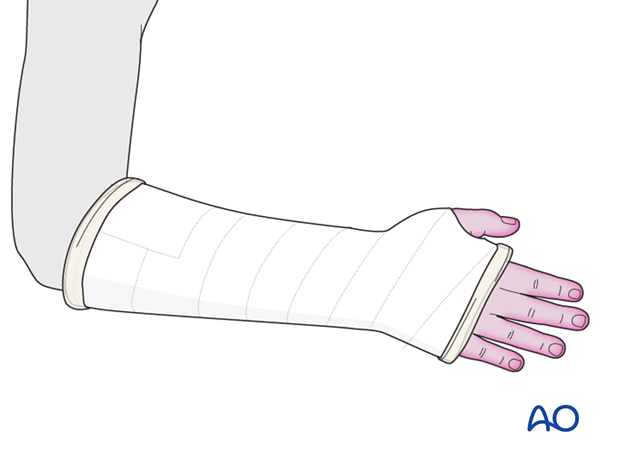
The K-wires are left protruding through the skin, bent and cut. The skin is protected with sterile padding prior to the application of a cast.
The illustration demonstrates the use of a small section of plastic tubing over the cut ends of the protruding wires. This adds further protection for the skin.
Note: Excessive pressure between dressing and skin should be avoided to prevent skin necrosis.
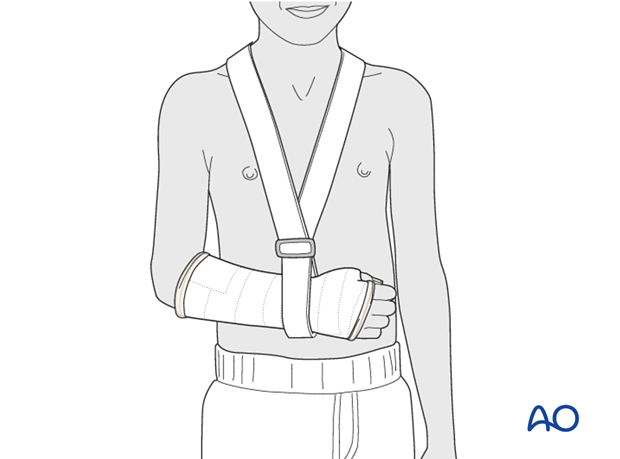
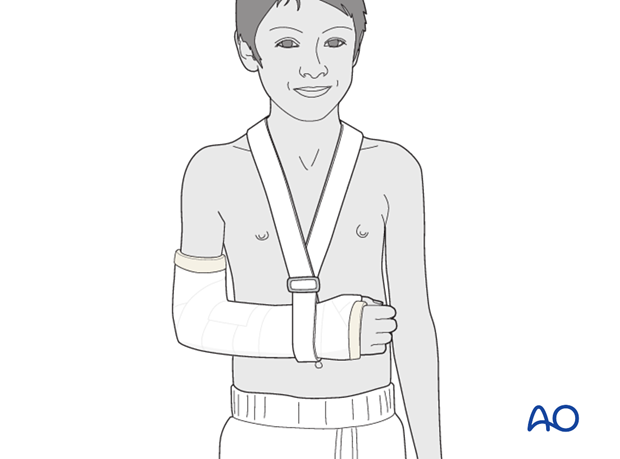
6. Short arm cast
General considerations
The purpose of the cast is protective and for pain relief, as stability is provided by the K-wire(s).
The short arm cast is applied according to standard procedure:
Note: In young, small, or noncompliant patients, it is safer to apply a long arm cast.
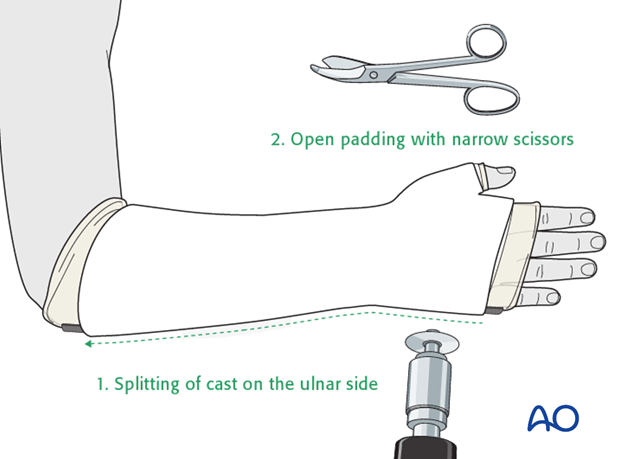
Splitting of cast
If a complete cast is applied in the acute phase after injury, it should be split over the full length of the cast. The split of the cast must be full thickness and expose the underlying skin.
7. Long arm cast
In the event that a long arm cast is necessary (see above) it is applied and split according to standard procedure.
8. Aftercare
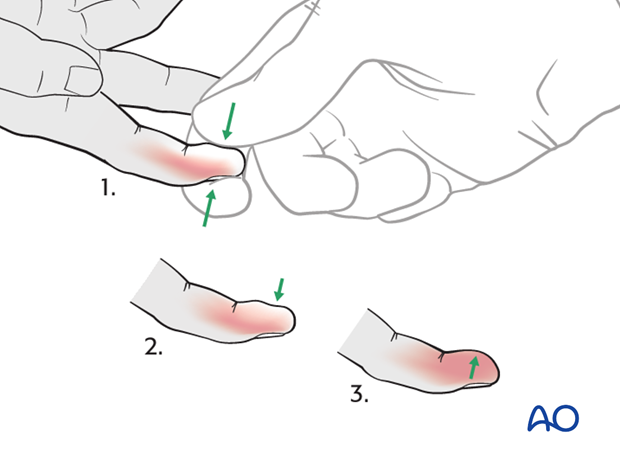
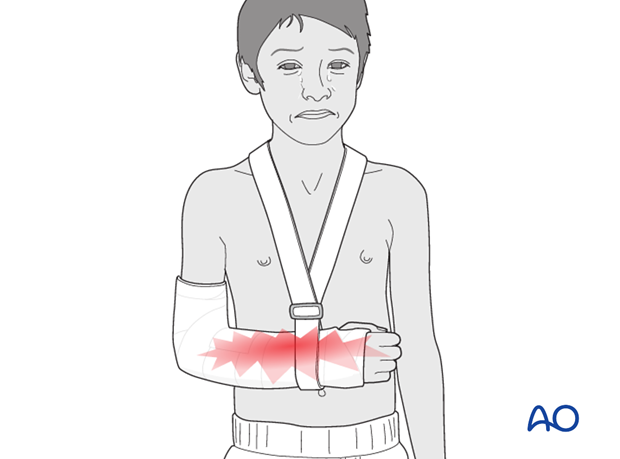
Tight cast
Further swelling in a restricting cast can cause pain, venous congestion in the fingers and occasionally a compartment syndrome.
For this reason any complete cast applied in acute phase should be split down to skin.
Parents/carers should be instructed how to detect circulatory problems by pressing and releasing the fingertips and watching if the blood flow/color returns to normal (capillary refill), compared to the opposite hand.
Compartment syndrome
Compartment syndrome is an unusual but serious complication after the application of a complete cast and can be difficult to diagnose, especially in younger children. Neurological signs appear late and the main sign is excessive pain on passive extension of the fingers.
It is important to make sure that the parents/carers are aware of the risk of compartment syndrome.
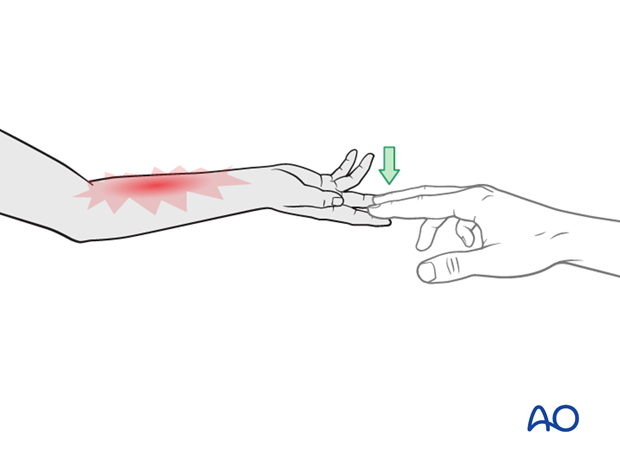
The parents/carers and patient should be informed to take note of increased pain and/or unresponsiveness to normal painkillers.
They should know that this may indicate serious complications. It is important for them to detect these signs as early as possible and report them urgently to the surgeon/nurse by telephone, or to attend the Emergency Room (ER) without delay.
Nerve compression is an occasional complication and the signs include:
- Sensory deficits (numbness)
- Weakness of active finger movement
- Paresthesia
Infections
See also the additional material on postoperative infections.
Cast care
If a normal plaster of Paris cast is used, it is important to keep the cast clean and dry in order to maintain the reduction.
When the swelling has reduced, the cast can become loose. The loss of support can result in loss of reduction.
In this circumstance, the parents/carers are advised to return to the healthcare provider.
Follow-up x-rays
Depending on the fracture pattern, the age of the child and the method of treatment, the patient has to return for follow-up x-rays to monitor the fracture position.
X-rays taken for fracture position can be taken with cast in place. Any x-rays to assess the state of bone healing must be taken without the cast and correlated with clinical examination.
In most cases, it is conventional to obtain follow-up x-rays after reduction to ensure that the position is maintained.
In general, in the child below 5 years of age, the follow-up is usually about 4-5 days after reduction. In the older child with a potentially unstable fracture, an x-ray would normally be taken at 7-10 days.
Further follow-up x-ray is a matter of clinical judgement, the responsibility of the treating surgeon, and tends to be longer in older children (see also Healing times).
For complete fractures of the metaphysis, redisplacement after reduction is not uncommon. It is therefore, important to take early follow-up x-rays in order to detect a possible redisplacement.
See also the additional material on posttraumatic growth disturbances.
K-wire removal
The K-wires can be removed without sedation in the clinic after approximately 3 weeks (depending on the age of the child).













