Posttraumatic growth disturbance
1. Introduction
Bone growth in the skeletally immature patient may be altered in several ways following long-bone trauma:
- Altered longitudinal growth rate, without physeal arrest - overgrowth
- Altered longitudinal growth rate, due to physeal arrest - shortening
- Altered physeal growth producing angular deformity
- Failure of modelling
2. Altered longitudinal growth rate, without physeal arrest - overgrowth
Longitudinal overgrowth principally affects the femur. [1-3]
- Mostly occurs in children aged 4-8 years [1]
- Mean overgrowth 1 cm (0.8 cm in Nottingham series [4]. Kregor et al. reported an average of 0.9 cm. (range, 0.3 to 1.4 cms) after femoral plating [3].
- Occurs within the 18/12 following fracture
- Aim for overlap with nonoperative treatment
- Most lengthening after fixation occurs intraoperatively ie, fixed long, rather than overgrowth
- Some is the result of periosteal stripping
- Occurs mostly if femur has healed short
- Also occurs with major open reduction
- Both possibly explained by effect of the inelastic periosteal cylinder that connects the proximal and distal perichondrial rings. If the sleeve is intact physeal growth is restrained
- If the tension in the periosteal cylinder is relaxed, for whatever reason, the rate of physeal growth will increase until such time as the sleeve re-tensions, or repairs itself, and thereby resumes its restraining effect on the physes
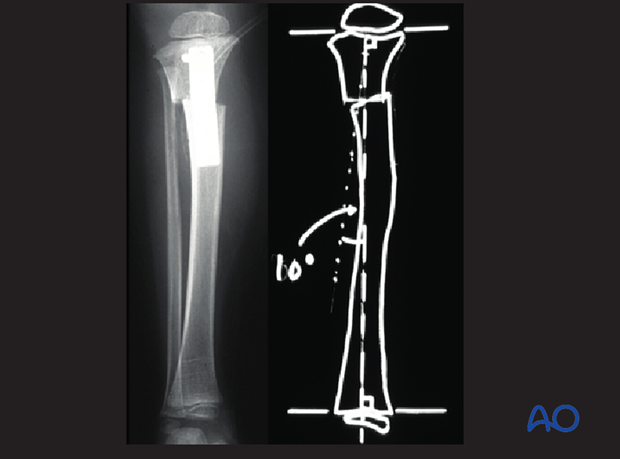
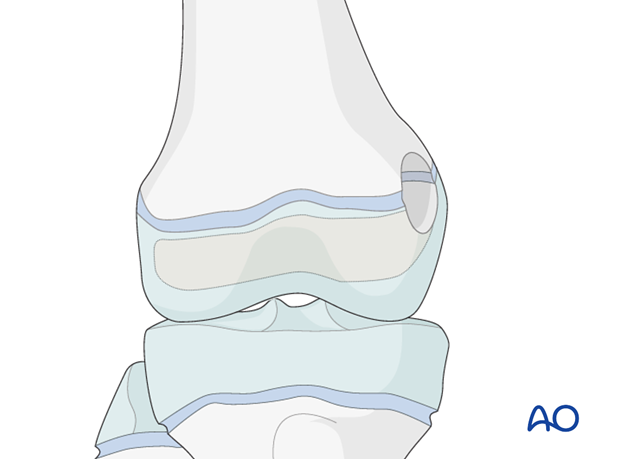
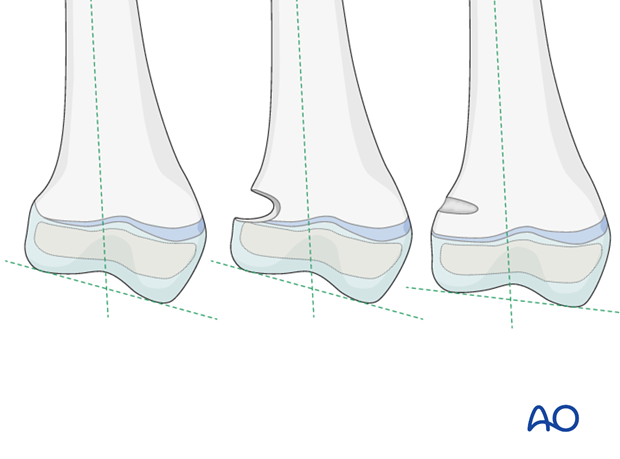
3. Valgus deformity resulting from proximal tibial metaphyseal fracture
Proximal tibial metaphyseal fractures are often characterized by a valgus deformity, with a gap in the medial cortex – so-called Cozen fracture.
Its reputation for progressive valgus deformity in the year, or two, following injury has been blamed on numerous factors:
- Inadequate closed reduction
- Too early weight-bearing
- Interposition of a pes anserinus/periosteal flap, which causes asymmetrical overgrowth by delaying the reconstitution of the periosteal restraint on the medial side
- Fibular tethering

The possibility of deformity should always be discussed with parents before treatment. Valgus occurs in 50% of proximal metaphyseal fractures. Maximal deformity occurs at 12-18 months after injury, usually followed by gradual modelling over several years. [6]
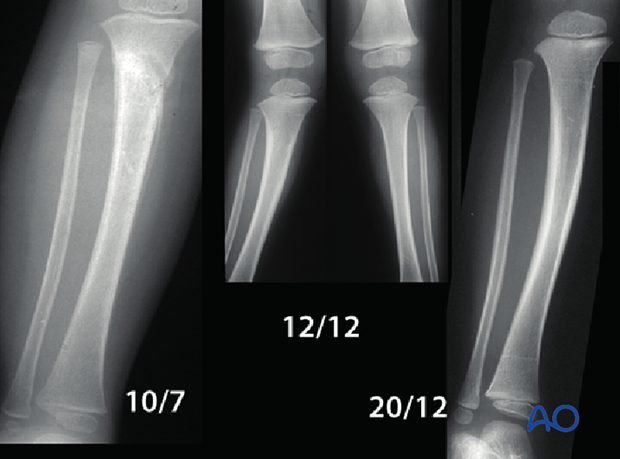
Such modelling defies the general rule that correction only occurs in the plane of motion of the adjacent joint.
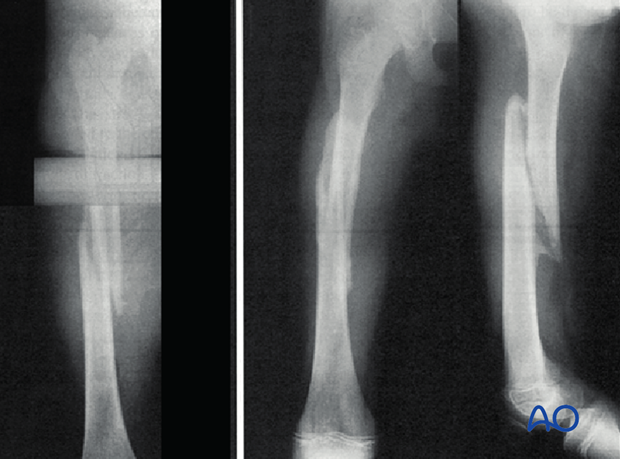
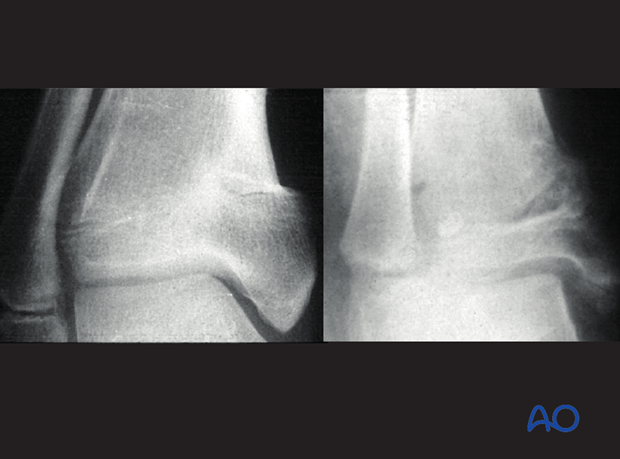
These pictures show valgus following a Cozen fracture modelled completely after 4 years.

Correction by osteotomy, or physeal stapling, should be deferred as long as possible so as to minimize the potential for recurrence. Correction of any recurrence, if necessary, can be obtained with hemiepiphysiodesis in early puberty [7].
In the past, planned, geometric, corrective osteotomy tended to be performed fairly early. However, modern practice is to wait, in the expectation of spontaneous correction, unless parents find the deformity unacceptable.
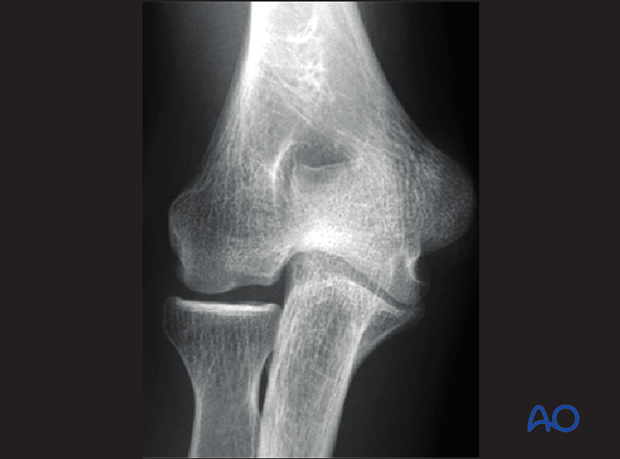
4. Altered longitudinal growth rate, due to physeal arrest - shortening
- Growth plate damage can lead to the formation of bony bar bridging and tethering the physis
- Increased incidence with increasing Salter Harris grade
- Commonest around knee (especially distal femur) and ankle
This X-ray show Central physeal arrest after Salter-Harris 5 injury

Treatment depends on the type of arrest, the type of deformity and the skeletal maturity of the patient.
Generally leg length inequality is easier to deal with than angular deformity, so consideration should be given to early epiphysiodesis to prevent deformity from developing.
Central growth arrest, if in a small area, can lead to a so-called fishtail deformity, necessitating excision of the physeal bar.
This X-ray show the end result of an untreated central growth arrest at the distal humerus
A wide physeal arrest can result in limb shortening without angular deformity, and requires leg-length balancing surgery.
5. Altered physeal growth producing angular deformity
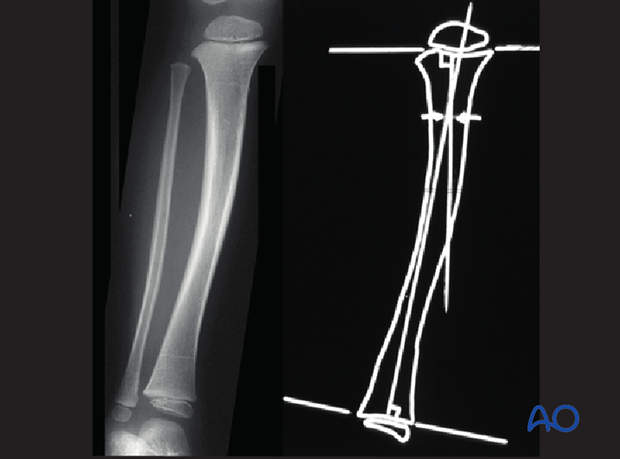
Asymmetrical physeal arrest leads to angular deformity, requiring planned corrective geometrical osteotomy, Ilizarov-type distraction, or selective epiphysiodesis.
The excision of physeal bars or tethers (epiphysiolysis), was introduced by Österman [8] in 1972, and popularized by Langenskiöld [9] in 1981.
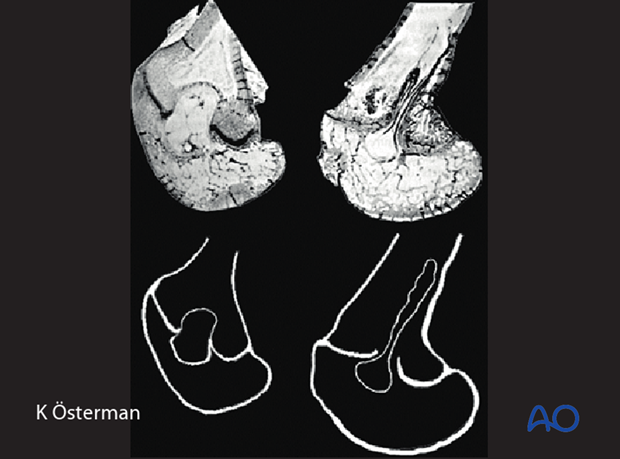
The physeal bar is mapped using CT/planar tomography.
The resultant map dictates surgical approach and technique.
If more than 50% of the cross sectional area of the physis is involved, then epiphysiolysis is contraindicated.
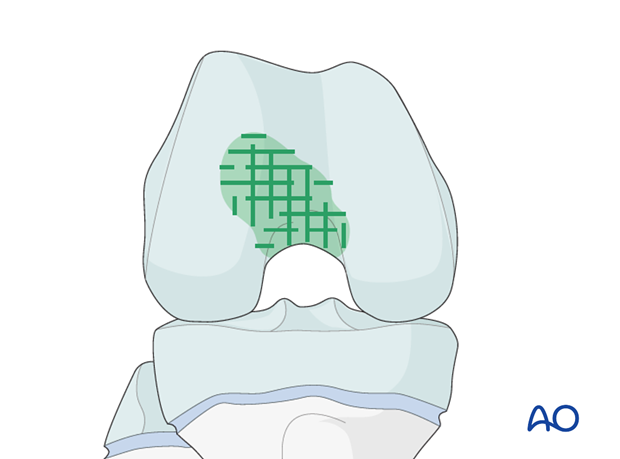
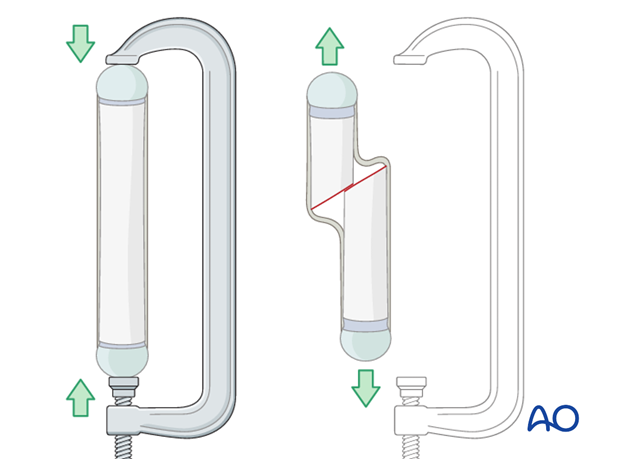
Through an appropriate cortical window in the metaphysis, the bar is carefully removed, using a cooled burr, until a “vein” of growth plate is seen to be continuous around the wall of the cavity.
The defect is then filled with an interposition material – usually fat, or cranioplast.
Different types of bar require different excision techniques.
Langenskiöld reported a high rate of successful reestablishment of physeal growth in 97 cases [9].
Epiphysiolysis is specialized surgery. It should be reserved for younger children with considerable remaining growth.
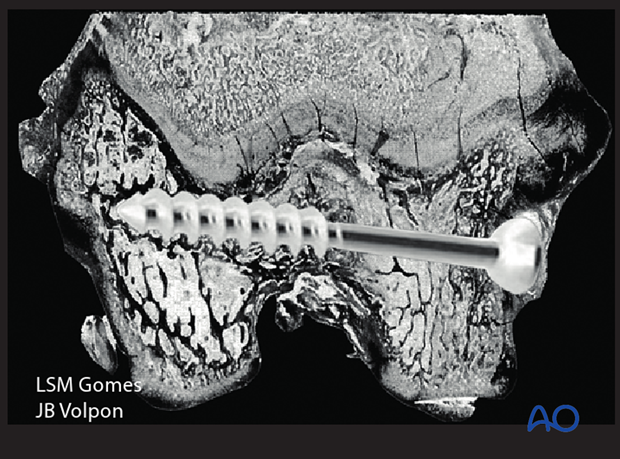
6. Experimental physeal disruption
Gomes and Volpon (1993) investigated the micro-evolution of physeal bars after Salter-Harris IV injuries, at a histological level.
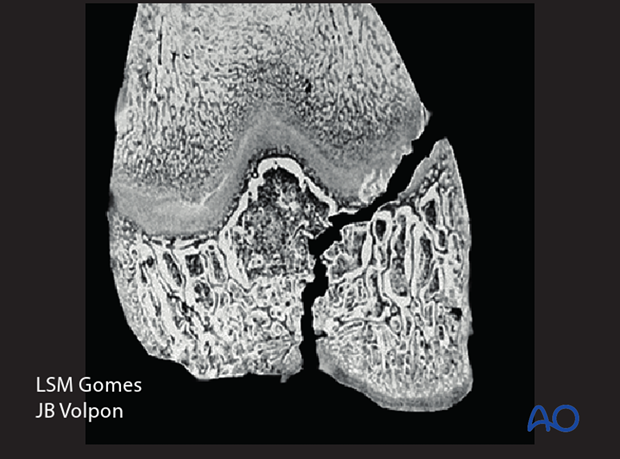
They demonstrated that if the transphyseal fracture plane was not closed by surgical fixation, vessels invaded the plane, laying down bone, so forming a bony tether across the physis. This led to a locus of growth arrest.
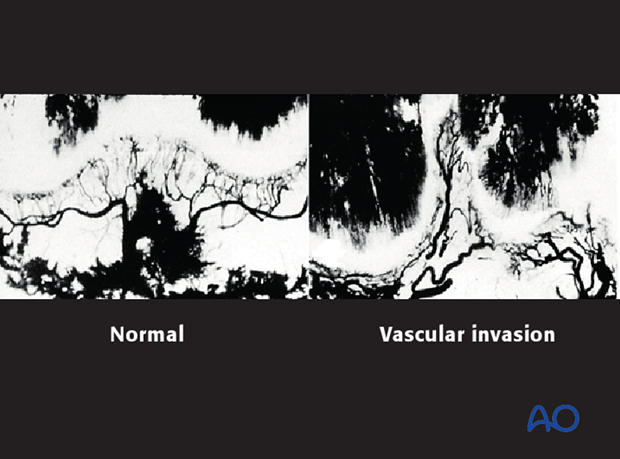
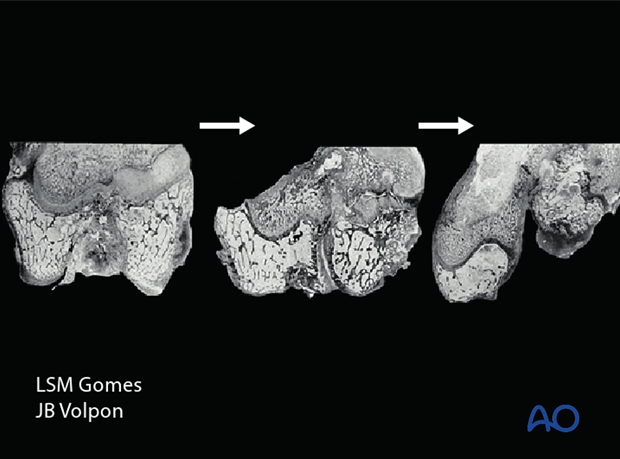
By contrast, if “watertight” reduction and fixation are performed, the vascular ingrowth into the fracture plane is prevented and physeal function is re-established and proceeds normally.
Conclusion
Any displaced intra-articular physeal fracture (Salter-Harris III and Salter-Harris IV) requires anatomical reduction and “watertight” fixation.
7. References
[1] Staheli LT. Femoral and tibial growth following femoral shaft fracture in childhood. Clin Orthop Relat Res 1967 Nov-Dec;55:159-163.
[2] Corry IS, Nicol RO. Limb length after fracture of the femoral shaft in children. J Pediatr Orthop . 1995 Mar-Apr;15(2):217-219.
[3] Kregor PJ, Song KM, Routt ML Jr, et al. Plate fixation of femoral shaft fractures in multiply injured children. J Bone Joint Surg Am. 1993 Dec;75(12):1774-80.
[4] Clement DA, Colton CL. Overgrowth of the femur after fracture in childhood. An increased effect in boys. J Bone Joint Surg Br. 1986 Aug;68(4):534-536.)
[5] Cozen, L. Knock knee deformity after fracture of the proximal tibia in children. Orthopedics. 1959;1:230-232.
[6] Robert M, Khouri N, Carlioz H, et al. Fractures of the proximal tibial metaphysis in children: review of a series of 25 cases. J Pediatr Orthop . 1987 Jul-Aug;7(4):444-449.
[7] McCarthy JJ, Kim DH, Eilert RE. Posttraumatic genu valgum: operative versus nonoperative treatment. J Pediatr Orthop . 1998 Jul-Aug;18(4):518-521.
[8] Osterman K. Operative elimination of partial premature epiphyseal closure. An experimental study. Acta Orthop Scand Suppl. 1972;3-79.
[9] Langenskiöld A. Surgical treatment of partial closure of the growth plate. J Pediatr Orthop . 1981;1(1):3-11.
[10] Gomes LS, Volpon JB. Experimental physeal fracture-separations treated with rigid internal fixation. J Bone Joint Surg Am. 1993 Dec;75(12):1756-1764.













