Long arm cast
1. Introduction
Pediatric considerations
Simple application of a plaster of Paris cast for an undisplaced, stable fracture is performed without sedation in older children and in compliant younger children.
The envirnment should be one in which the child and the parents/carers are comfortable.
Important considerations include:
- A child-sensitive approach
- Child-friendly clinical area
- Careful explanation of the procedure, in language that is understood by the child and the parents/carers
- Availability of all equipment and material
When a procedure including manipulation is required, general anesthesia is usually necessary.
Indications
Unstable fractures require a long arm cast to control forearm rotation and therefore decrease the risk of displacement.
In a very young child, or when there are concerns about compliance, a long-arm cast is always required.
A cast applied in the period immediately following injury, should be adequately padded and split longitudinally.
2. Preparation for cast application
Equipment
- Examination couch
- Tubular bandage (40-80 mm wide, depending on the size of the child)
- 2-4 rolls of padding (40-150 mm wide, depending on the size of the child)
- 2-8 plaster of Paris (POP) bandages (40-150 mm wide, depending on the size of the child)
- Malleable (thermoplastic, leather, or lead) strip
- Bucket with cold water
- Protective aprons for the team members and the child
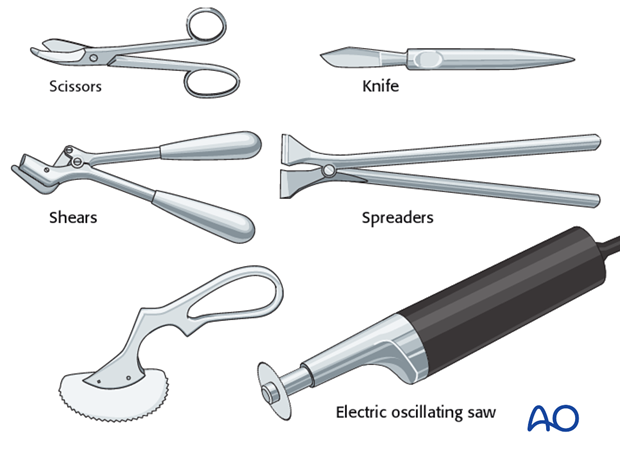
- Appropriate equipment to cut, split, or remove the cast
3. Long arm cast
Flexion of arm
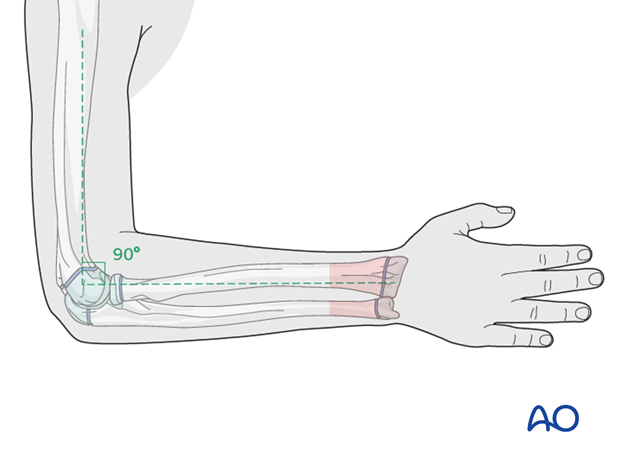
The elbow is flexed to 90° prior to application of the tubular bandage and padding, to avoid compression at the antecubital fossa.
The forearm is placed in neutral rotation for undisplaced, stable fractures.
Preparation for splitting the cast
A temporary malleable (thermoplastic, leather, or lead) strip can be placed beneath the tubular bandage, prior to plaster application, in order to protect the skin when plaster splitting is required.
The location of the strip should be planned to avoid:
- Areas of molding
- Areas with underlying, protruding K-wires
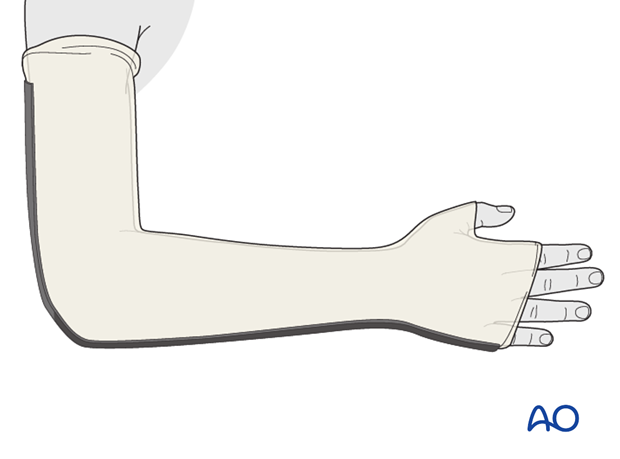
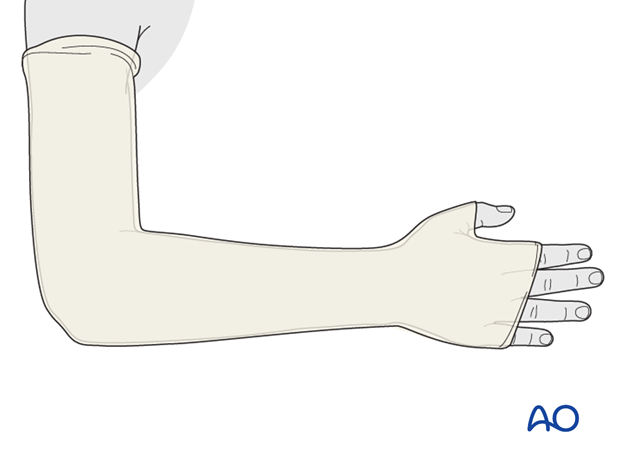
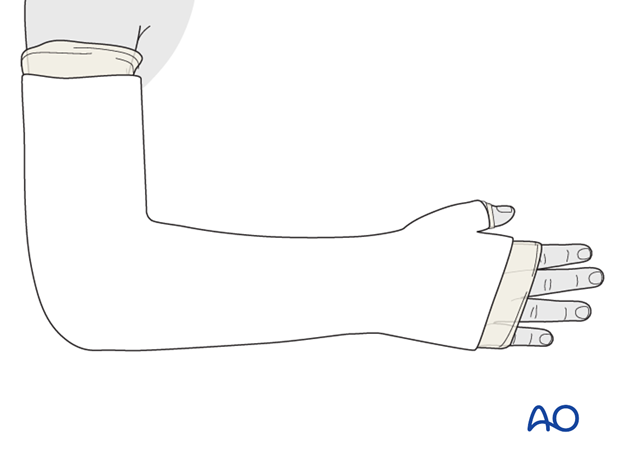
Application of tubular bandage
A tubular bandage is applied directly onto the skin and malleable strip, from the axillary crease to just distal to the MCP joints allowing sufficient bandage for protection of the cast edges.
A hole is cut for the thumb.
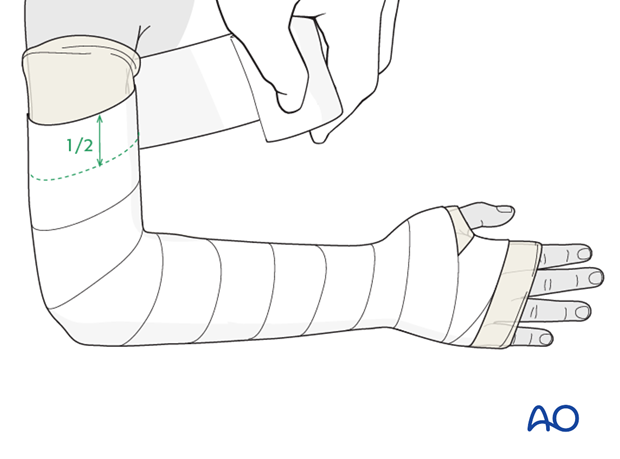
Application of padding
A single layer of padding is applied from the MCP joints of the fingers and thumb to the axillary crease.
Each layer is overlapped by 1/2.
Extra padding should be applied over pressure areas, including the olecranon and any protruding K-wires.
Care is taken not to constrict the antecubital fossa.
The tubular bandage and padding should be applied without creases.
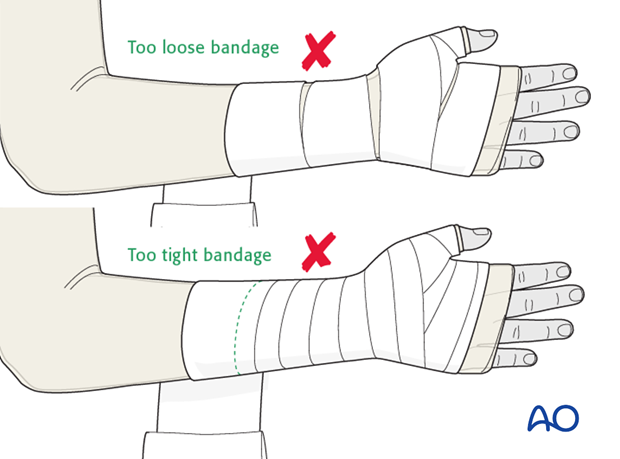
Application of plaster
The POP bandage is immersed for 5-10 seconds and excess water is then removed by gentle squeezing.
A complete plaster is applied using layers of appropriately-sized POP bandage.
The plaster extends distally to the metacarpal heads and palmar flexor crease and proximally to just distal to the axillary crease.
Excess plaster is trimmed to accommodate the thumb and fingers.
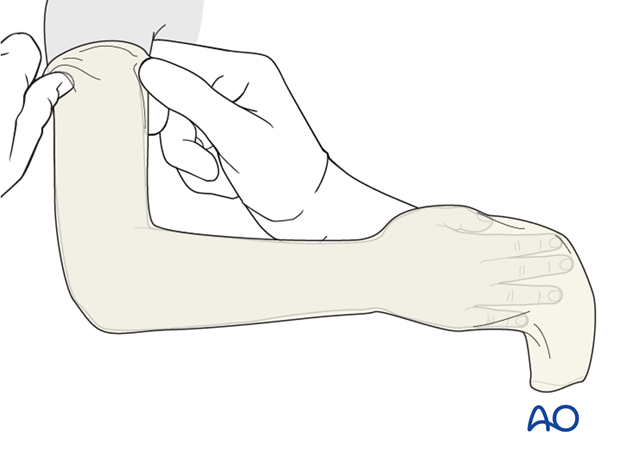
Completion of plaster cast
The proximal and distal ends of the tubular bandage are folded over the cast and covered with an additional single layer of plaster bandage.
It is important to ensure that the edges of the cast are well-padded and smooth, to avoid abrasion during the period of plaster immobilization.
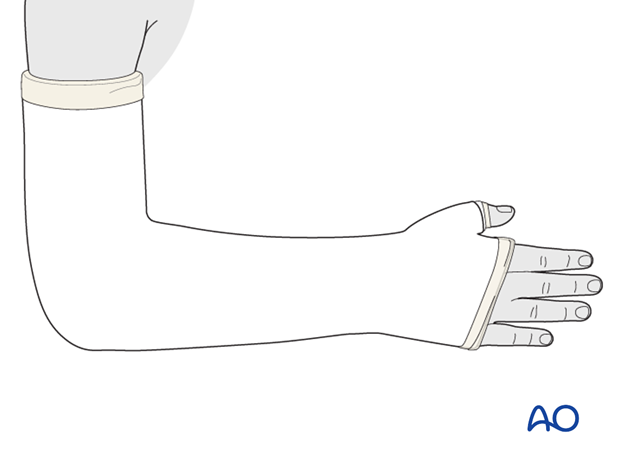
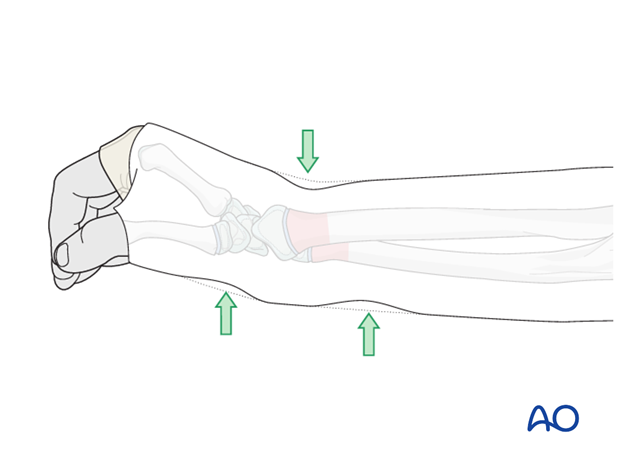
The cast should be oval in cross section, conforming to the anatomy of the forearm. The surgeon should apply manual pressure using the his/her thenar eminence, to produce three-point fixation, until the plaster is hardened.
The cast is gently molded to provide three point fixation at the fracture site reducing the likelihood of displacement.
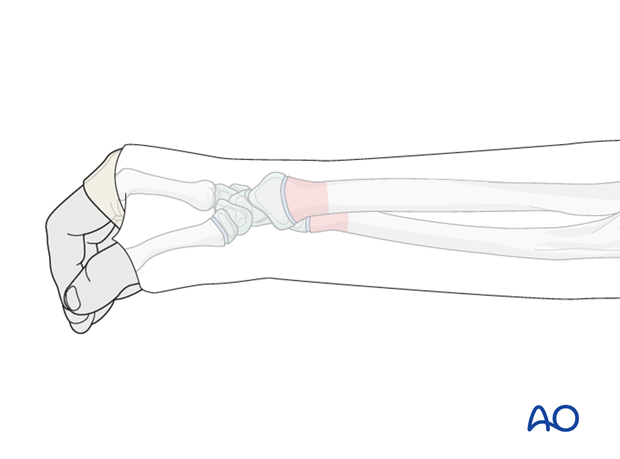
Illustration shows molding to maintain reduction for posteriorly displaced fractures.
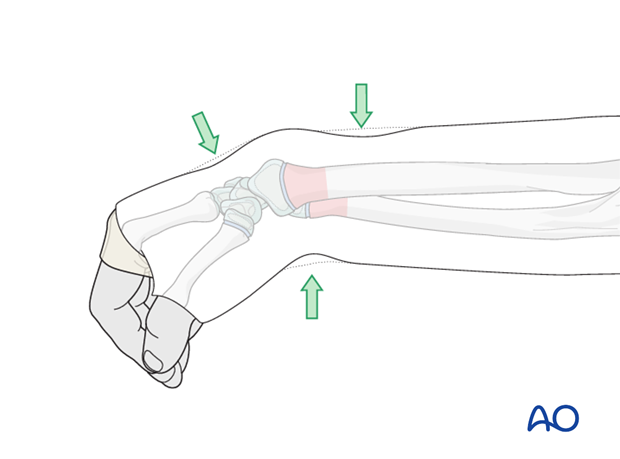
Illustration shows molding to maintain reduction for anteriorly displaced fractures.
The assistant should support the limb until the cast is hardened.
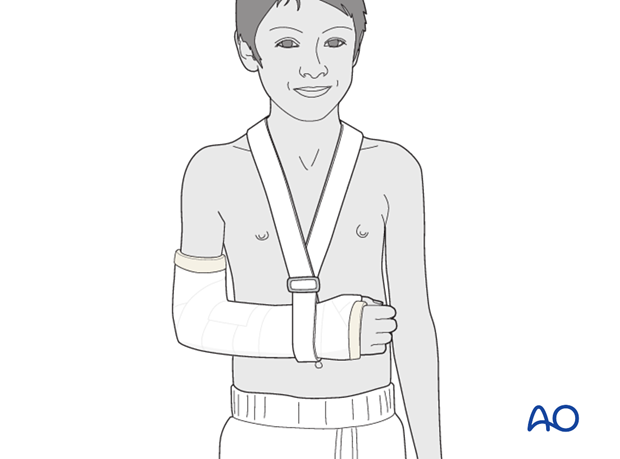
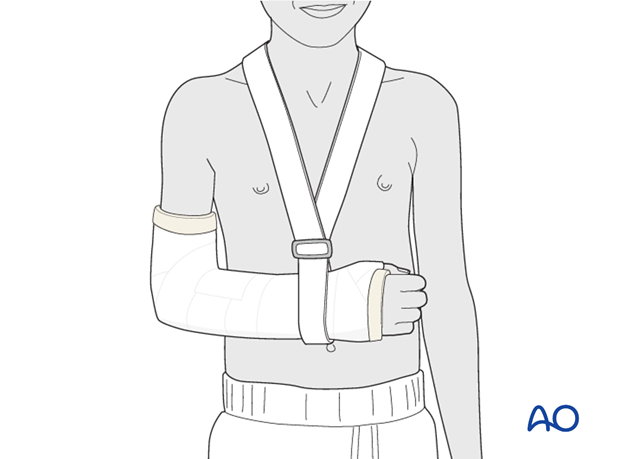
The arm is supported in a sling.
Splitting the cast
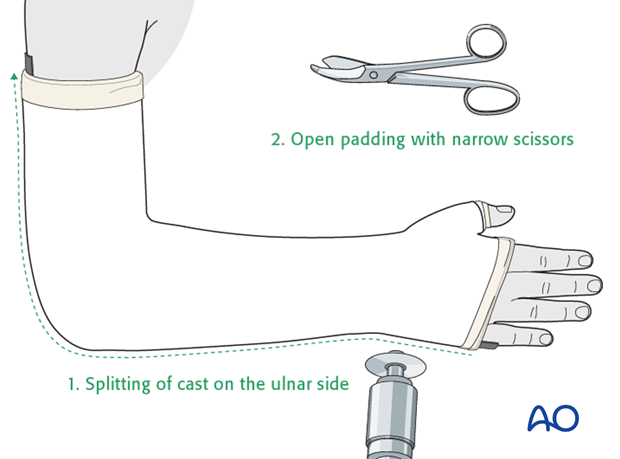
When required, the plaster should be split along the entire length of the medial border, unless this encroaches on an area of molding or any underlying, protruding K-wire.
Once the cast is hardened, it is marked, then split using an oscillating saw, a hand saw, or a sharp plaster knife.
Great care is taken to avoid injury to the underlying skin
The split is widened with a cast spreader. The underlying padding can then be divided with scissors and the protective strip is removed to expose the skin
A crêpe bandage is applied to protect the split cast.
When the swelling has subsided (after 5-7 days), the cast can be completed with a single POP bandage.
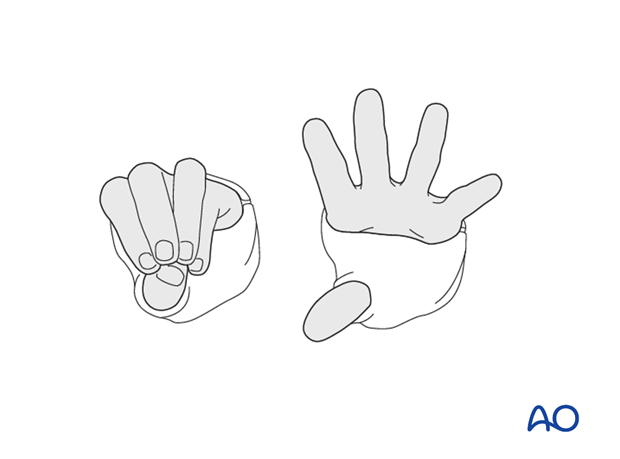
The ability to passively, or actively, fully extend the fingers without discomfort indicates absence of muscle compartment compression.
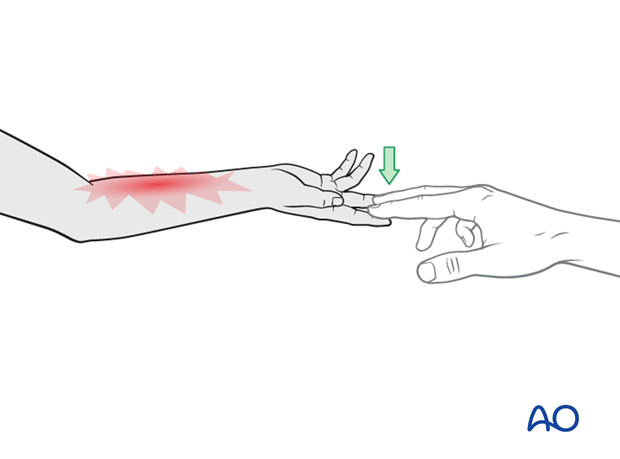
The ability to passively, or actively, fully extend the fingers without discomfort indicates absence of muscle compartment compression.
Care should be taken to ensure that the plaster cast does not restrict flexion of the MCP joints.