MIO - Percutaneous lag screws
1. Principles
Anatomical reduction
Anatomical reduction of the articular fracture component and fixation with absolute stability is mandatory.
Make sure the lateral meniscus is not caught in the fracture line
2. Patient preparation and approach
Patient preparation
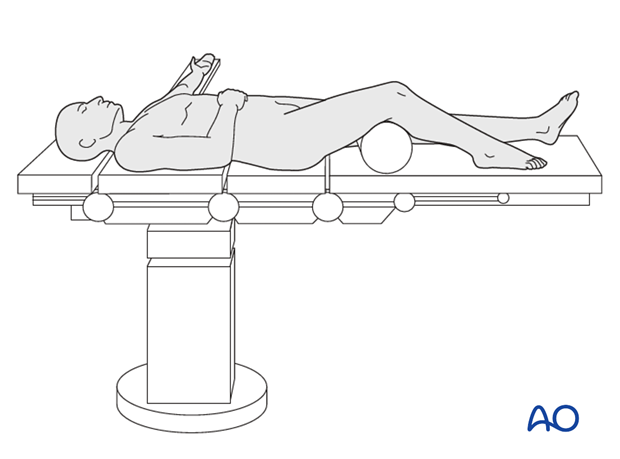
This procedure is normally performed with the patient in a supine position.
Approach
In order for screws to achieve a lag or compression effect at the fracture, they must be inserted perpedicular to the fracture plane. The fracture plane therefore dictates screw entry points.
If there is concern about the proximity of major nerves, simple stab incisions should not be used, the skin should be incised followed by blunt dissection to avoid nerve damage.
3. Reduction
Single clamp
Indirect reduction may be achieved by external manipulation of the fractured fragment using clamps. In cases where adequate closed reduction is not achieved the joint should be opened to allow anatomical reduction.
Check the reduction either arthroscopically or under image intensification.
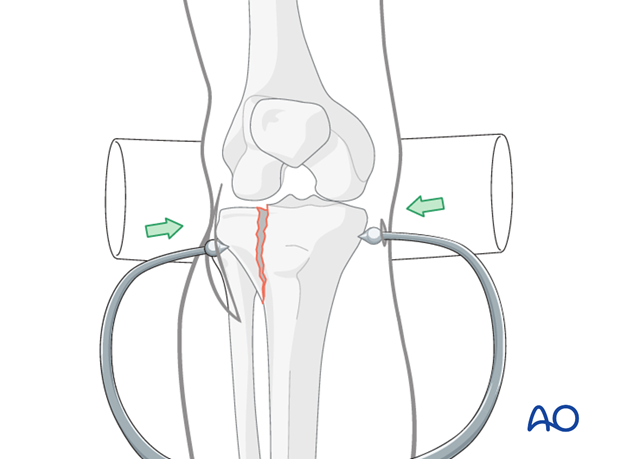
Multiple clamps
Depending on the fracture configuration more than one clamp may be necessary as shown in the image.

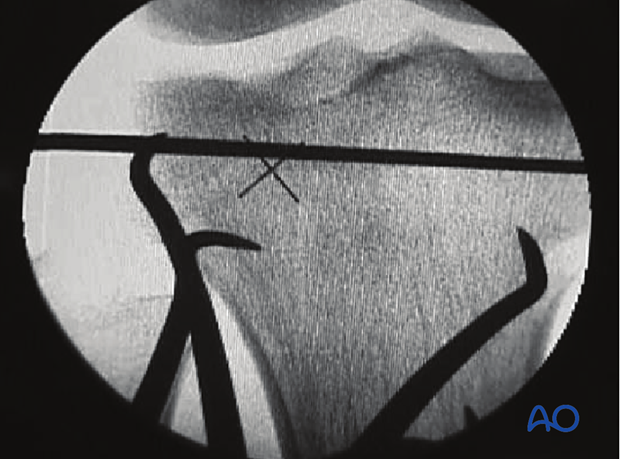
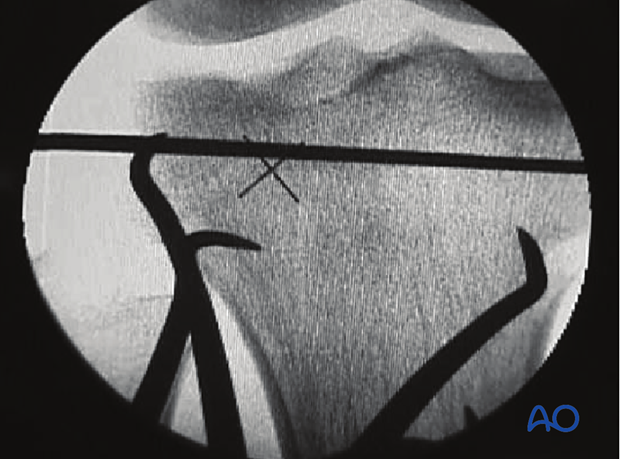
Secure reduction with K-wire
Apply a K-wire to secure the reduction and to facilitate cannulated screw fixation.
4. Fixation
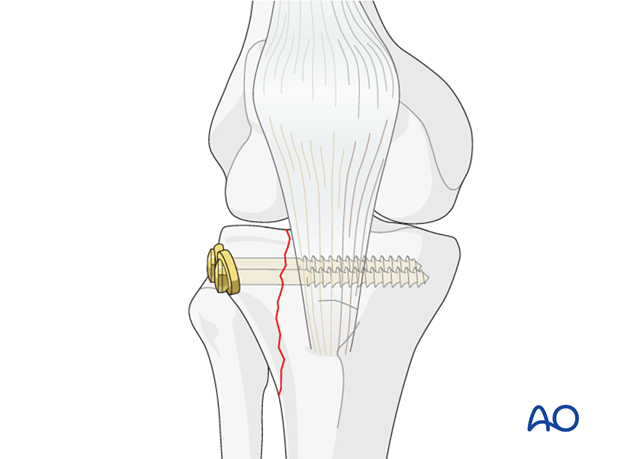
Lag screw application
Once anatomic reduction of the fracture is obtained fixation follows with two cancellous screws with washer. In young people screw fixation is enough. In older individuals a buttress plate should be added to prevent displacement.
Use image intensification to check the length and position of the implants.
The cortex in the lateral tibial head is thin. Therefore, the use of washers is needed in the majority of the patients.
Click here for a detailed description of the lag screw technique.
5. Aftercare
Compartment syndrome and nerve injury
Close monitoring of the tibial compartments should be carried out especially during the first 48 hours after surgery to rule out compartment syndrome.
The neurovascular status of the extremity must be carefully monitored. Impaired blood supply or developing neurological loss must be investigated as an emergency and dealt with expediently.
Functional treatment
Unless there are other injuries or complications, mobilization may be performed on post OP day 1. Continuous passive motion (CPM) splints are very helpful in the early phase of rehabilitation. Static quadriceps exercises with passive range of motion of the knee should be encouraged. Afterwards special emphasis should be given to active knee and ankle movement.
Following any injury, and also after surgery, the neurovascular status of the extremity must be carefully monitored. Impaired blood supply or developing neurological loss must be investigated as an emergency and dealt with expediently. The goal of early active and passive range of motion is to achieve as full range of motion as possible within the first 4 - 6 weeks. Optimal stability should be achieved at the time of surgery, in order to allow early range of motion exercises.
Weight bearing
No weight bearing in the treatment of articular fractures for a minimum of 10 – 12 weeks.
Follow up
Wound healing should be assessed on a short term basis within the first two weeks. Subsequently a 6 and 12 week follow-up is usually performed. If a delayed union is recognized, further surgical care will be necessary and should be carried out as soon as possible.
Implant removal
Implant removal is not mandatory and should be discussed with the patient.













