Lag screws
1. Principles
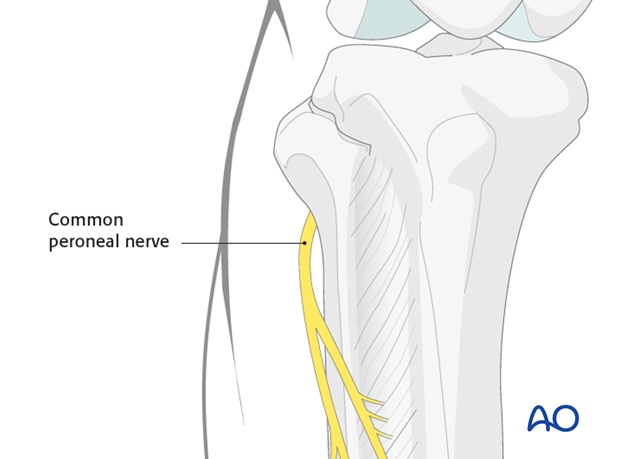
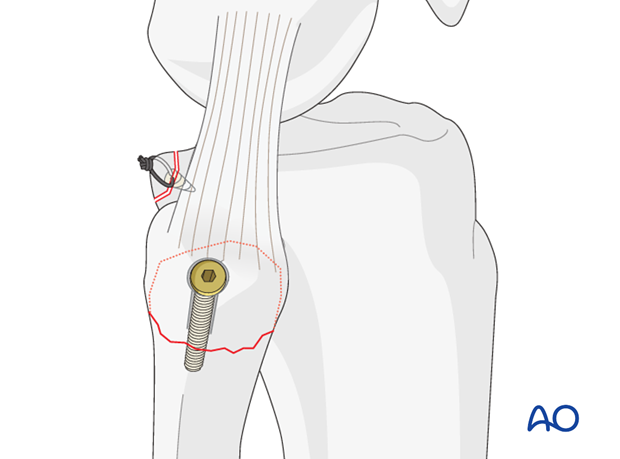
Peroneal nerve
The peroneal nerve runs around the fibular neck. So be careful with the reduction and clamp placement.
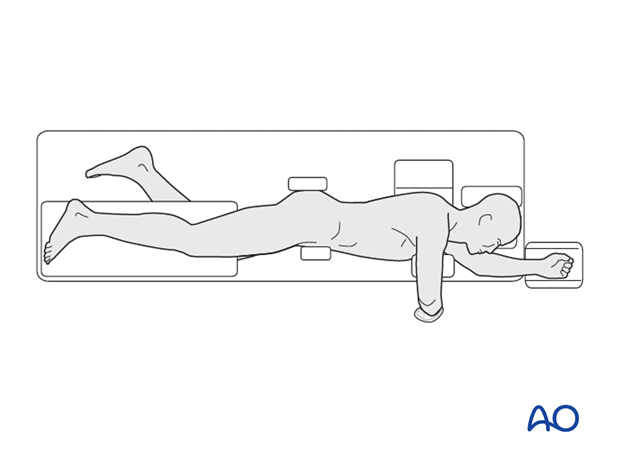
2. Patient preparation
This procedure is normally performed with the patient in a lateral position.
3. Approaches
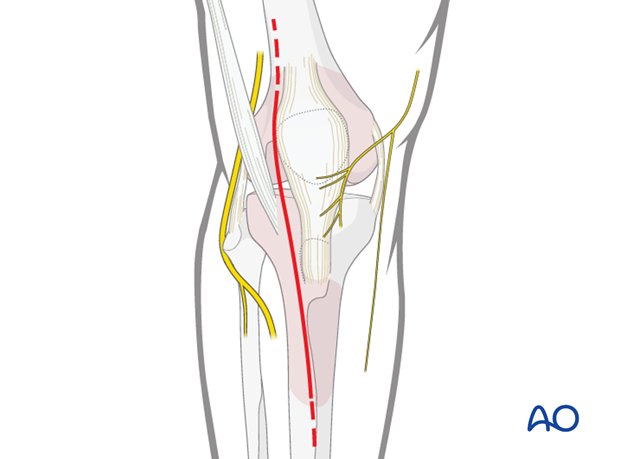
Safe zones for percutaneous instrumentation
Inserting percutaneous instrumentation through safe zones reduces the risk of damage to neurovascular structures.
Anterolateral approach
For open reduction an anterolateral approach is used.
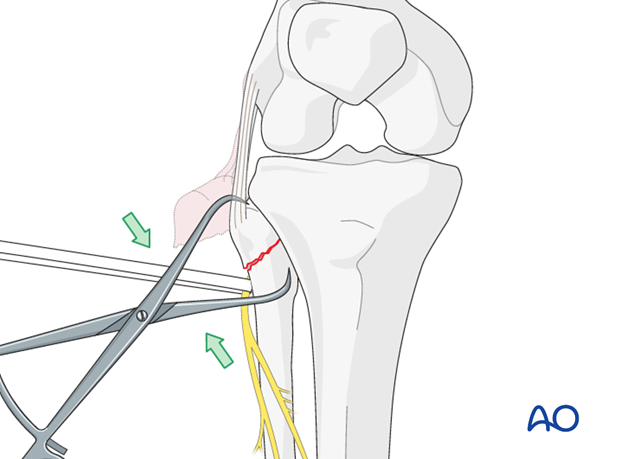
4. Reduction
After direct exposure of ligaments and the avulsed fibular head, reduction may be achieved with the use of a small clamp that is placed on the fibula and the bone fragment. Protect the peroneal nerve which runs below the tendon of biceps femoris and then winds around the fibular neck from back to front in contact with bone.
5. Fixation
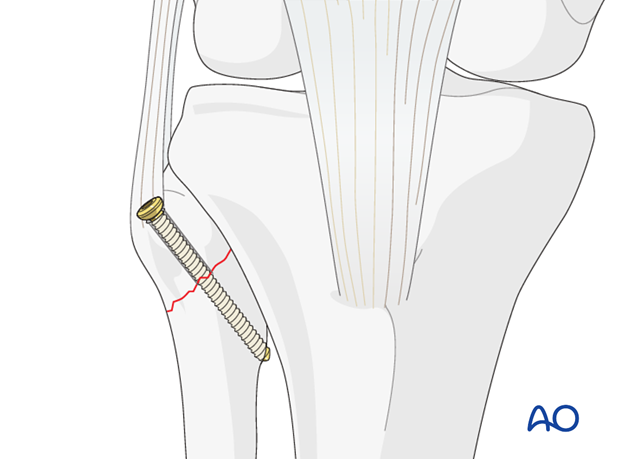
Lag screw application
Optimal fixation is achieved by lag screw fixation in a proximal–lateral to medial–distal direction. The medial cortex of the fibula may be engaged. Usually 3.5 mm cortical screws are used.
Click here for a detailed description of the lag screw technique.
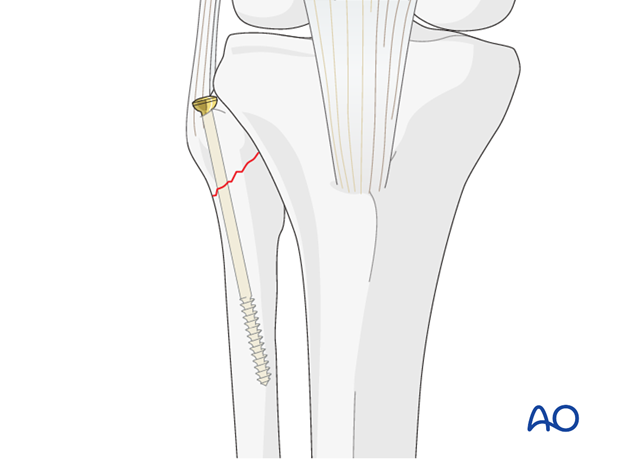
Alternative: lag screw in medullary canal
Alternatively, a lag screw may be inserted at a steeper angle, into the medullary canal of the fibula. 4.0 mm cancellous bone screws can be used.
Any injury to the posterolateral corner should be repaired very early in the healing process. Residual knee instability will be the result if the posterolateral corner is not dealt with definitively at an early stage.
Secondary reconstruction provides worse results than early posterolateral corner repair.
6. Aftercare
The neurovascular status of the extremity must be carefully monitored. Impaired blood supply or developing neurological loss must be investigated as an emergency and dealt with expediently.
Functional treatment
Functional treatment shall be applied for 2 – 3 days with patient still resting in bed starting on postoperative day 1.
The goal of early active and passive range of motion is to achieve a full range of motion within the first 4 – 6 weeks. Maximum stability is achieved at the time of surgery.
In noncompliant patients consider the use of a hinged knee brace.
Weight bearing
The patient can be fully weight bearing but care must be taken not to apply a varus distracting force. For this reason, crutches are advisable as a means of protection.
Follow up
Wound healing should be assessed on a short term basis within the first two weeks. Subsequently, an 8 week follow-up is usually performed.
Implant removal
Implant removal is not mandatory and should be discussed with the patient.













