Open reduction internal fixation
1. Introduction
The severity of these injuries should not be underestimated. Although the radiographic findings can be subtle, the combination of medial and lateral injury can lead to recurrent elbow instability.
Principles
Fractures of the anteromedial facet of the coronoid are usually associated with LCL injuries and subluxation, but not dislocation of the elbow. If the trochlea subluxates into the coronoid defect, the elbow will become arthritic.
Compliant patients with small fractures and a congruent elbow joint can be treated nonoperatively. If there is any sign of subluxation, the bias should be towards surgical repair: Buttress plate fixation of the coronoid fracture and reattachment of the LCL to the lateral condyle.
Variations of the injury
- In some variations of these injuries the olecranon is fractured.
- Some elbow dislocations are associated with small anteromedial facet fractures. These can be very unstable elbow dislocations and the role fixation of the coronoid vs external fixation of the elbow is unclear.
2. Positioning
The patient is placed in a supine position with the arm on the table. If available, a sterile tourniquet may be advantageous as it increases the surgical field.
3. Approaches
Either a medial or posterior skin incision can be used.
The best exposure of the anteromedial facet of the coronoid is to split the flexor carpi ulnaris, which fully exposes the ulnar nerve.
4. Fixation
Sequence of repair
Whether to fix the bone or ligament first is surgeon’s choice.
Coronoid repair
Most fractures are fixed with a buttress plate. Smaller fragments can be secured with a suture lasso.
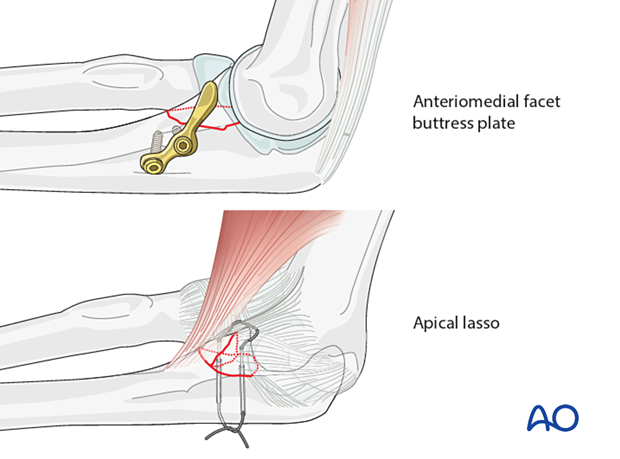
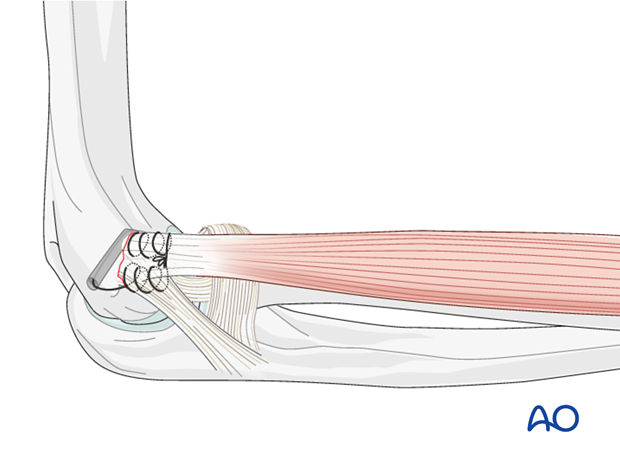
Ligament repair
The LCL can be repaired with either sutures or anchors depending on the pathoanatomy and surgeon's preference.
5. Final assessment
Check for joint instability or any sign of residual subluxation.
6. Postoperative treatment following ORIF
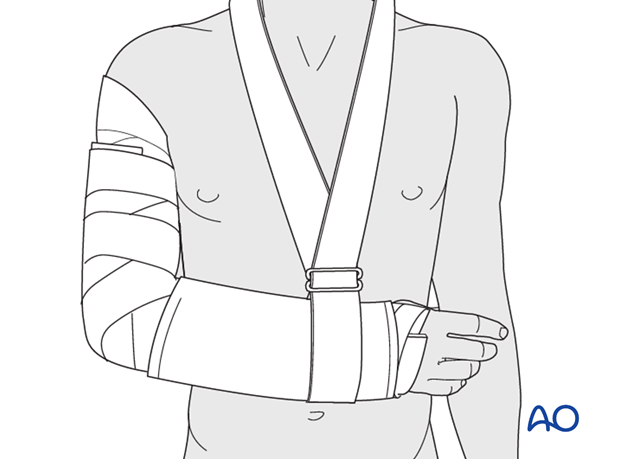
Postoperatively, the elbow may be placed for a few days in a posterior splint for pain relief and to allow early soft tissue healing, but this is not essential. To help avoid a flexion contracture, some surgeons prefer to splint the elbow in extension.
If drains are used, they are removed after 12–24 hours.
Mobilization
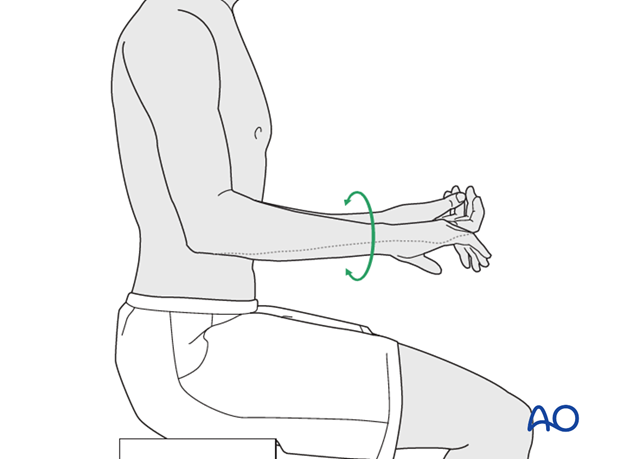
Active assisted motion is encouraged within the first few days including gravity-assisted elbow flexion and extension. Encourage the patient to move the elbow actively in flexion, extension, pronation and supination as soon as possible. Delay exercises against resistance until healing is secure.
Use of the elbow for low intensity activities is encouraged, but should not be painful.
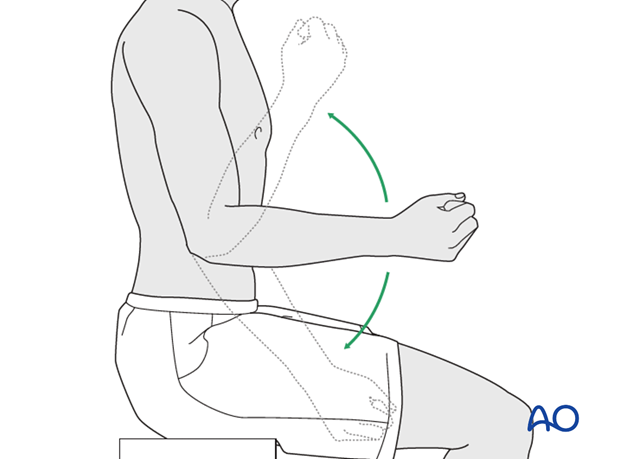
Range of motion must be monitored to prevent soft tissue contracture.
Prevent loading of the elbow for 6–8 weeks.
Monitor the patient to assess and encourage range of motion, and return of strength, endurance, and function, once healing is secure.
Follow up
The patient is seen at regular intervals (every 10–20 days at first) until the fracture has healed and rehabilitation is complete.
Implant removal
As the proximal ulna is subcutaneous, bulky plates and other hardware may cause discomfort and irritation. If so, they may be removed once the bone is well healed, 12–18 months after surgery, but this is not essential.













