Lag screws
1. Principles
Treatment goal
The patellofemoral joint is biomechanically very stressed when the knee is loaded. Any compromise of the joint surface is likely to lead to degenerative joint disease. It is, therefore, highly desirable, in vertical patellar fractures to strive for anatomical reduction of the joint surface and stable fixation with interfragmentary compression.
Combination of techniques
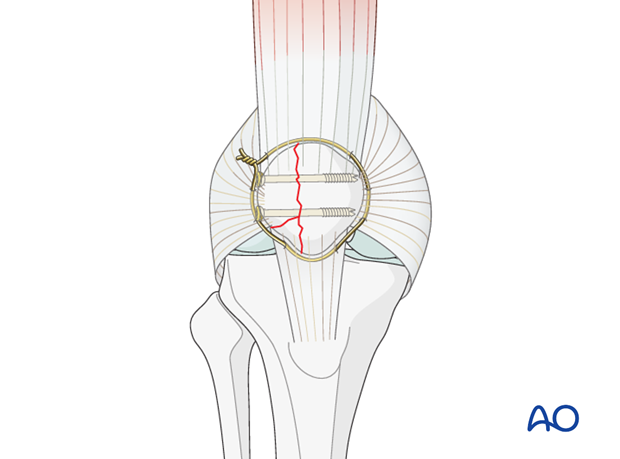
In fragmentary partial articular sagittal fractures, lag screw fixation alone, following anatomical reduction, provides absolute stability of the main fragments.
The addition of cerclage wiring is not necessary as the longitudinal integrity of the extensor mechanism is not disrupted. However, a cerclage wire may be added to fix any small fragment.
Screw size
Historically 4.5 screws were used but have been found to be too large. Now it is more common to use 3.5 or 2.7 screws.
Verification of reduction
Anatomical reduction of the articular surface is monitored by palpating the joint from inside, as neither inspection nor the x-ray will reveal a minor step off. This will require creation of a small arthrotomy.
Nevertheless, an image intensifier or X-ray should always be available, so that the reduction can be checked in the AP and lateral planes if needed.

2. Patient preparation and approach
Patient preparation
This procedure is normally performed with the patient in a supine position with the knee flexed 30°.

Approach
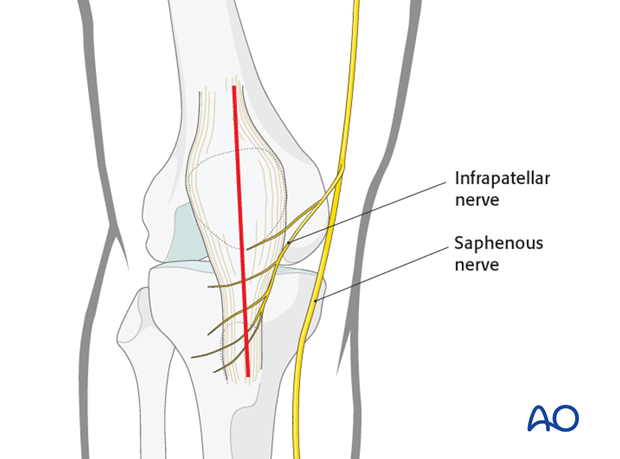
For this procedure a mid-axial longitudinal approach is used.
3. Reduction and fixation
Fracture debridement
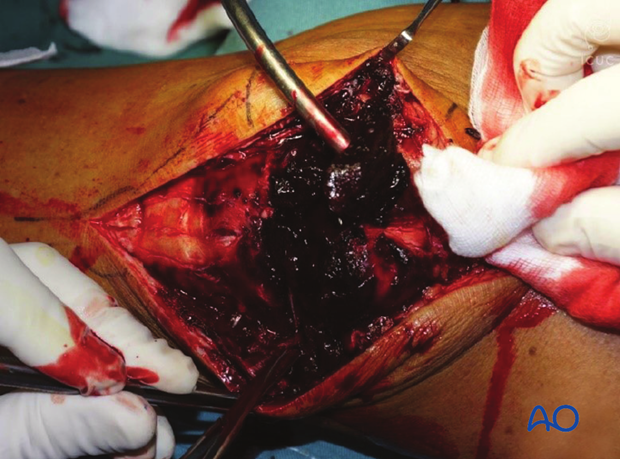
The knee joint and fracture lines must be irrigated and cleared of blood clots and small debris to allow exact reconstruction.
Reduction
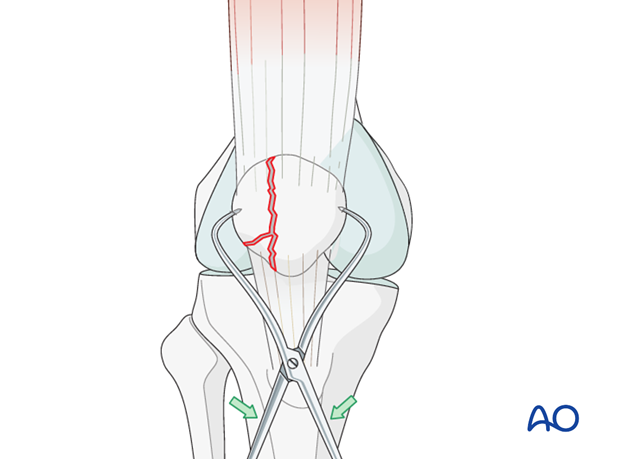
With the knee in flexion, reduce the major fracture fragments using a pointed bone reduction forceps tenaculum.
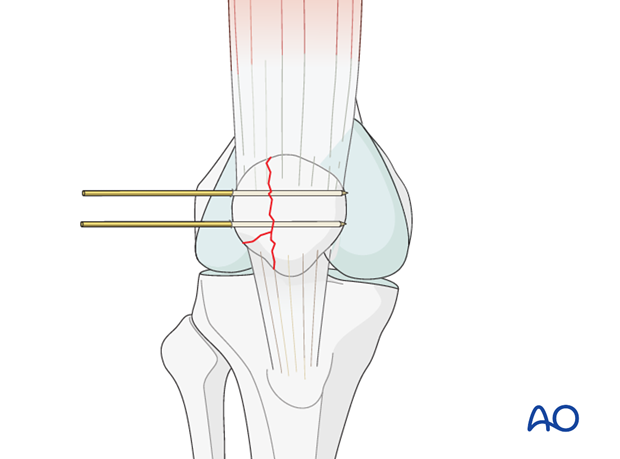
Temporary fixation
Two K-wires are inserted through the planned screw trajectory with the fracture reduced
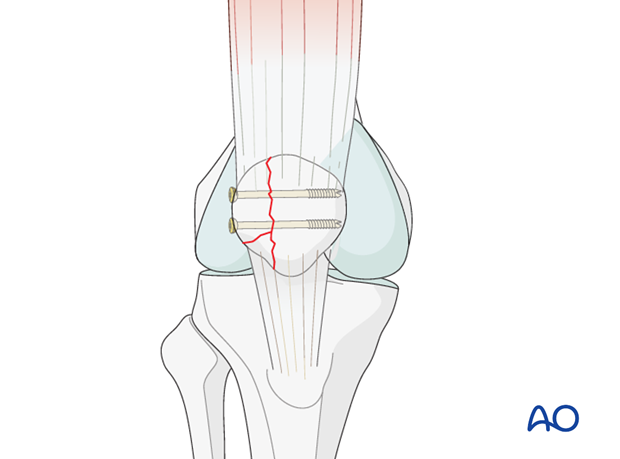
Fixation
Insert two partially threaded cannulated lag screws over the K-wires.
Alternatively, a fully threaded screw may be inserted using the appropriate technique.
Anatomical restoration of the articular surface is verified by palpation if possible.
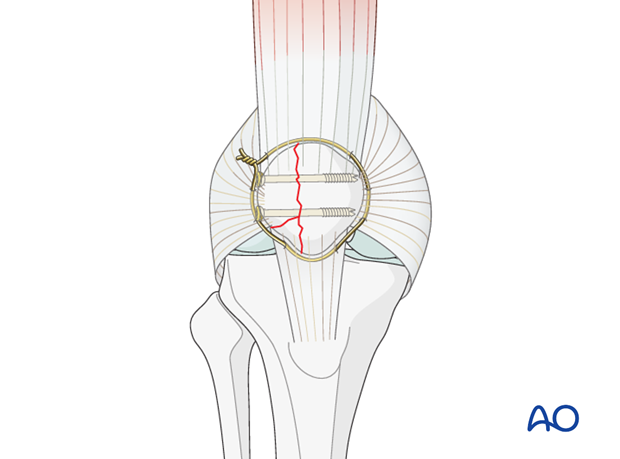
Fixation of small fragment with cerclage wire
Preliminarily fix the small fragment with bone reduction forceps.
Use a circular cerclage wire to secure its reduction after the lag screw insertion.
4. Aftercare following cerclage compression wiring/lag screw/plate fixation of the patella
Introduction
Active knee function requires an intact knee extensor mechanism, a mobile patella, a well-preserved patello-femoral joint and muscle strength.
After satisfactory reduction and fixation of patellar fractures, early controlled range of motion exercises are combined with static quadriceps strengthening exercises. The progressive increase in loading of the patello-femoral joint depends on many factors and requires planned individual programs, designed by the surgeon and physical therapists.
Functional treatment
Patellar fixation is generally quite stable. Early progressive, active mobilization is beneficial after surgery. Despite, wearing a splint to protect against never losing complete extension, range of motion is done throughout the day with the splint off. Static isometric quadriceps exercises should be started on postoperative day 1 with the splint in place. Usually the anterior incision is slow to heal as it is over a flexion surface and so it is usually best to leave the knee in extension for at least a week.
Afterwards, special emphasis should be given on active knee and hip movement.
Weight bearing
A removable full extension knee splint is applied and worn until good quadriceps control is regained. Full weight bearing may be performed with a straight knee, using crutches or a walker, from postoperative day 1.
Follow-up
Wound healing should be assessed regularly during the first two weeks. X-rays should be taken at 2, 6 and 12 weeks. A longer period may be required if fracture healing is delayed.
Implant removal
Implant removal may be required, as the wires may be prominent under the skin. Implant removal should not be undertaken until a minimum of 1 year postoperatively.
Thrombo-embolic prophylaxis













