Mid-axial longitudinal approach to the patella
1. Introduction
This universal approach can be used for all patellar fractures.
2. Surgical anatomy
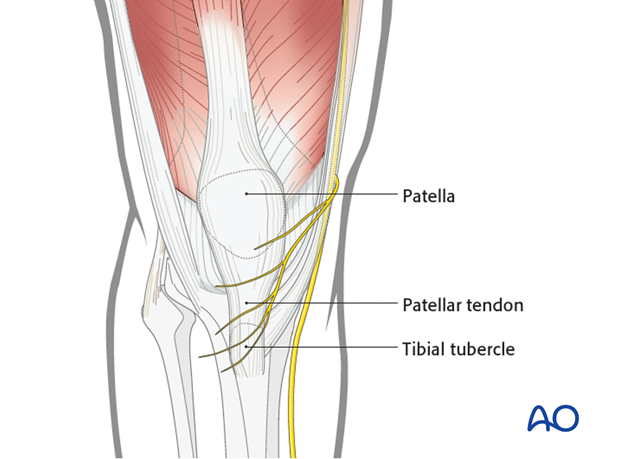
The patella is located within the extensor apparatus of the knee.
Anatomical features include the proximal articular body, with an extraarticular anterior surface and a posterior articular surface, and the extraarticular distal pole.
The rectus femoris and vastus intermedius muscles insert at the superior pole of the body and the vastus medialis and vastus lateralis muscles on either side.
The patellar tendon originates from the inferior pole and inserts into the tibial tuberosity.
The articular surface has the thickest layer of cartilage in the body, up to 5 mm, reflecting the very high resultant loads across the patellofemoral joint, rendering it susceptible to chondromalacia and degenerative joint disease.
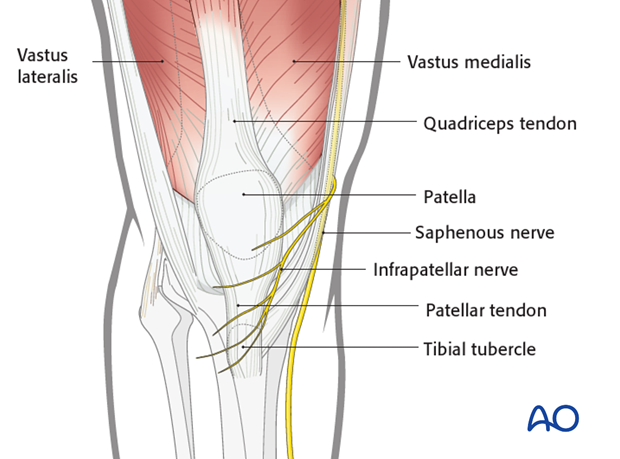
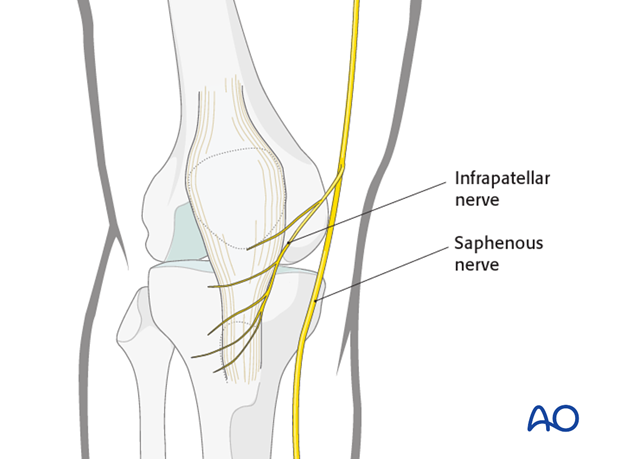
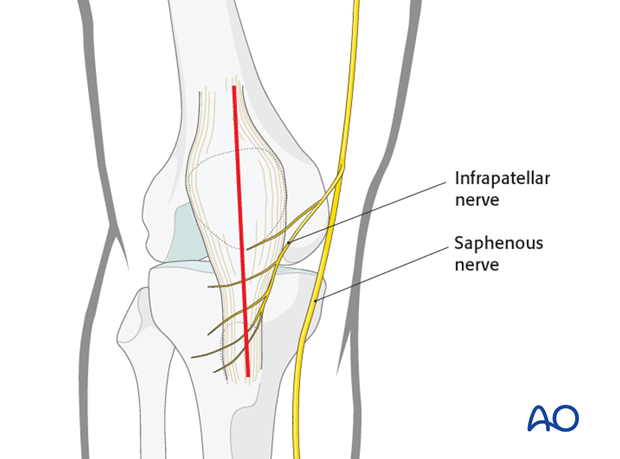
The saphenous nerve runs along the medial aspect of the distal femur. The infrapatellar branches of the saphenous nerve lie on the medial and inferior aspects of the patella and run across to the lateral side. Postoperatively, there is usually minor sensory loss to the lateral side of the scar, but significant saphenous nerve damage is avoidable. Occasionally, there may be postsurgical saphenous nerve neuroma formation which is rarely a significant problem.
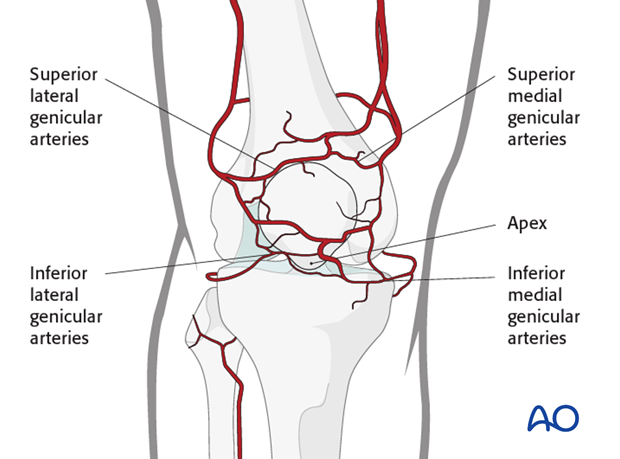
The anterior surface is surrounded by an extraosseous arterial ring, which receives inflow from branches of the genicular arteries. This anastomotic ring supplies the patella through mid-patellar vessels, which penetrate the middle third of the anterior surface, and the polar vessels, which enter the apex.
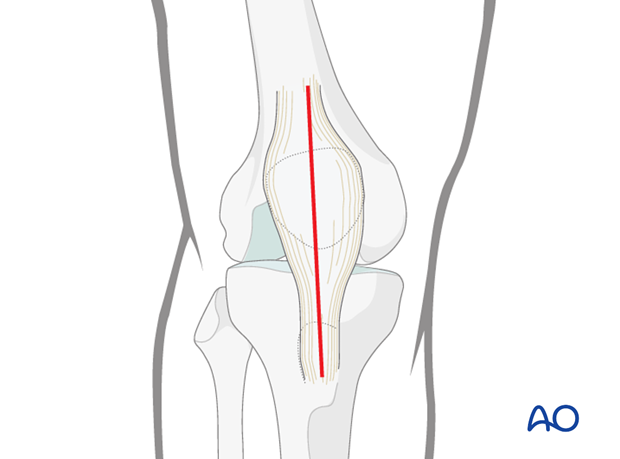
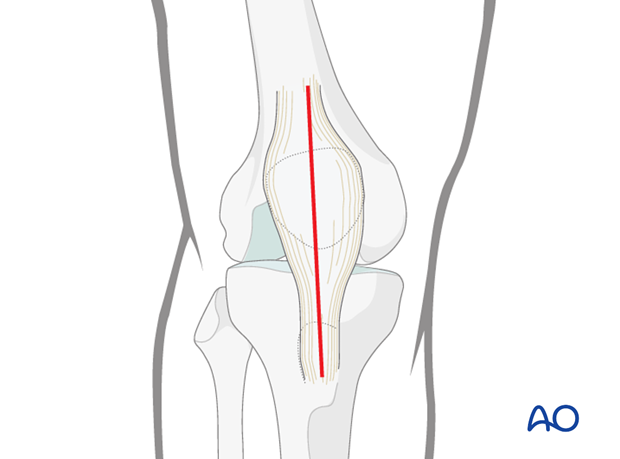
Longitudinal approach
A longitudinal mid-axial incision is the preferred approach because it offers excellent exposure of the fracture site and can be extended proximally or distally. This incision may be re-opened for any further surgery at any stage in the future should it be required.
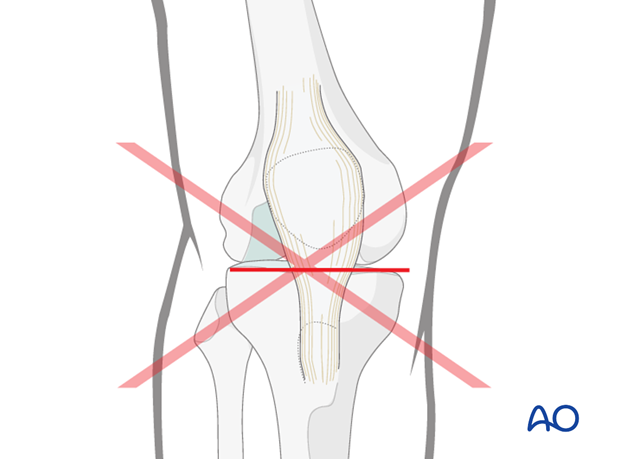
3. Other approaches
In the past some surgeons used a transverse approach to the patella. This is not recommended as wound healing is frequently a problem. Additionally, should reconstructive knee surgery be required later in life, a transverse pre-patellar scar may compromise healing.
Parapatellar incisions are also possible, especially in the case of an open fracture. A medial parapatellar arthrotomy is made if it is necessary to inspect the knee joint and intraarticular surgery can still be performed as needed.
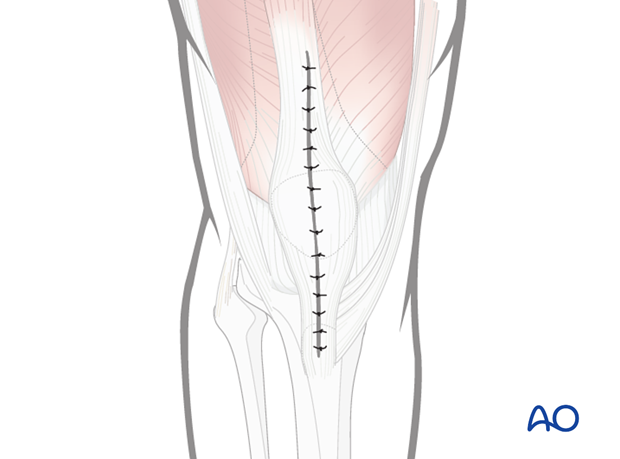
4. Skin incision
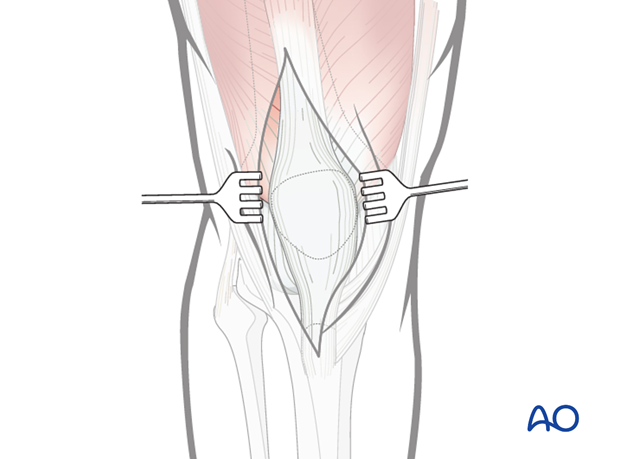
The landmarks are the patella, the patellar tendon and the tibial tubercle, which are easily palpable.
Make a longitudinal mid-axial incision from 5 cm above the superior pole of the patella to the tibial tubercle.
Full thickness flaps should be developed to avoid damage to skin blood supply.
5. Dissection down to the patella
After incision of the superficial fascia, the complete extent of the injury must be identified. There may well be traumatic tears in the lateral and medial retinacula and the knee joint capsule.
In open fractures, or a preexisting chronic bursitis, the prepatellar bursa may be excised.
6. Wound closure
Before closure, irrigate wounds copiously with warm Ringer lactate solution.
Care should be taken to suture any tears in the lateral and medial parapatellar retinacula. The use of suction drains may be considered. Skin closure can be performed according to surgeon's preference.