Sleeve fracture fixation
1. Principles
Treatment goal
The patello-femoral joint is biomechanically very stressed when the knee is loaded. Any compromise of the joint surface is likely to lead to degenerative joint disease.
It is, therefore, highly desirable, in patellar fractures to strive for anatomical reduction of the joint surface and stable fixation. In addition, a treatment goal is restoration of function of the knee extensor mechanism.
Imaging
Sleeve fractures are very rare and may be very subtle on x-rays as the sleeve remaining within the avulsed tendon is thin and is often not apparent on over-penetrated images, whilst at the same time, the lower pole of the patella may have a virtually normal profile.
2. Patient preparation and approach
Patient preparation
This procedure is normally performed with the patient in a supine position with the knee flexed 30°.

Approach
For this procedure a mid-axial longitudinal approach is used.

3. Reduction and fixation
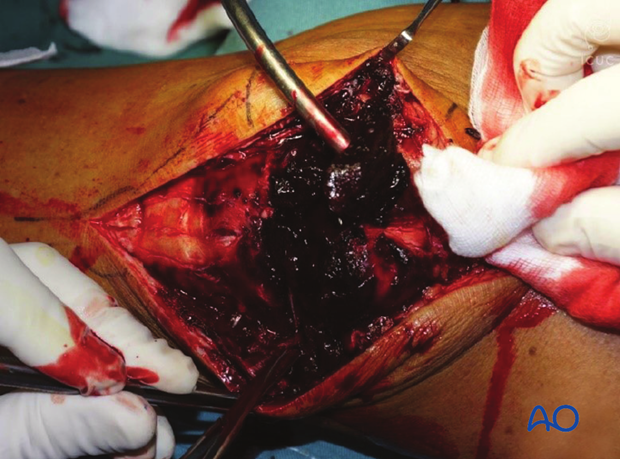
Fracture debridement
The knee joint and fracture lines must be irrigated and cleared of blood clots and small debris to allow exact reconstruction.
Reduction and temporary fixation
A Weber clamp is used to reduce the fracture before fixation.
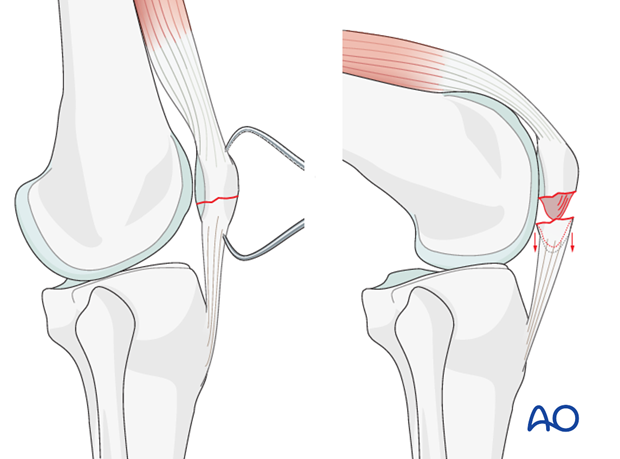
Fixation of avulsion
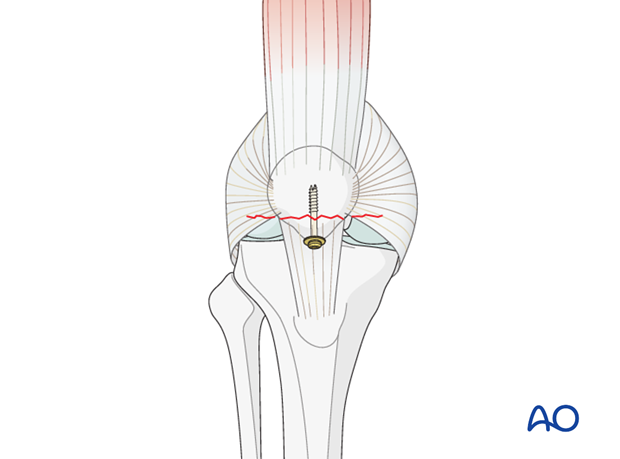
Insert a partially threaded cannulated screw, with a washer, as a lag screw.
The fixation is checked with an image intensifier in AP and lateral planes.
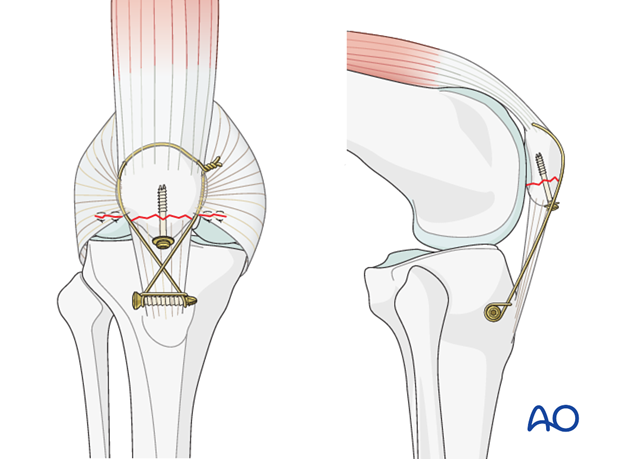
Neutralization of bending forces
As implant pull-out, or failure, is virtually inevitable, the bending distraction forces must be neutralized by additional patellotibial cerclage.
Repair any tears of the lateral and medial patellar retinacula with sutures.
4. Aftercare following patellar sleeve fracture fixation
Introduction
Active knee function requires an intact knee extensor mechanism, a mobile patella, a well-preserved patello-femoral joint and muscle strength.
Knee stiffness and muscle weakness can become a problem after the necessary period of casting. Once deemed to be healed, a regimen of progressive knee mobilization and muscle strengthening must be supervised closely by the rehabilitation team.
Functional treatment
Patellar sleeve fracture fixation may not be completely stable. A period of immobilization in an extension splint is required. Usually the anterior incision is slow to heal as it is over a flexion surface and so it is usually best to leave the knee in extension for at least a week. Static isometric quadriceps exercises should be started on postoperative day 1 in the knee extension splint. At a later stage, special emphasis should be placed on active knee and hip movement continuing protection with a removable knee splint.
Weight bearing
Full weight bearing may be performed with the aid of crutches, or a walker, from postoperative day 1 with the knee extension splint in place. Splintage is usually maintained until about 6-8 weeks postoperatively.
Follow-up
Wound healing should be assessed regularly within the first two weeks. X-rays are of very limited value during follow-up. Clinical parameters (such as pain, tenderness, quadriceps control, active straight-leg raising, etc.) will guide the surgeon and the physical therapist in determining the pace of functional rehabilitation.
Implant removal
Implant removal may be required as the cerclage wire may be prominent under the skin. Patients should be warned that cerclage wires may break during the healing process and may need to be removed.
Thrombo-embolic prophylaxis
Consideration should be given to thrombo-embolic prophylaxis, according to local treatment guidelines.













