Patellar tendon repair
1. Principles
There exist circumstances in which the patellar fragments cannot be reduced adequately and when function of the extensor apparatus remains compromised. Patella tendon repair can produce acceptable results. The secret is attention to operative detail by a skilled surgeon.
2. Patient preparation and approach
Patient preparation
This procedure is normally performed with the patient in a supine position with the knee flexed 30°.

Approach
For this procedure a mid-axial longitudinal approach is used.

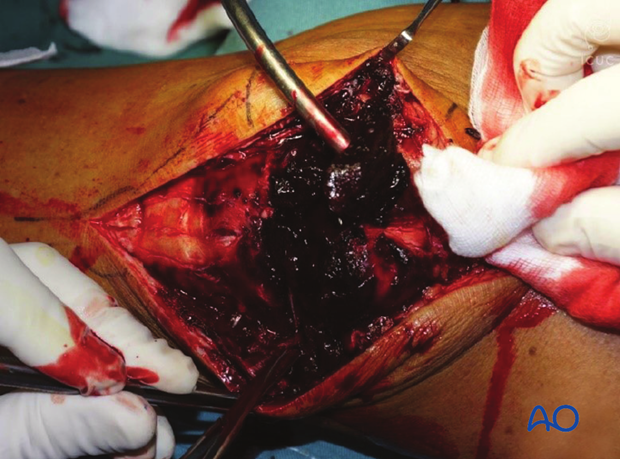
3. Debridement
The knee joint and fracture lines must be irrigated and cleared of blood clots and small debris to allow exact reconstruction.
4. Patellar tendon repair and augmentation
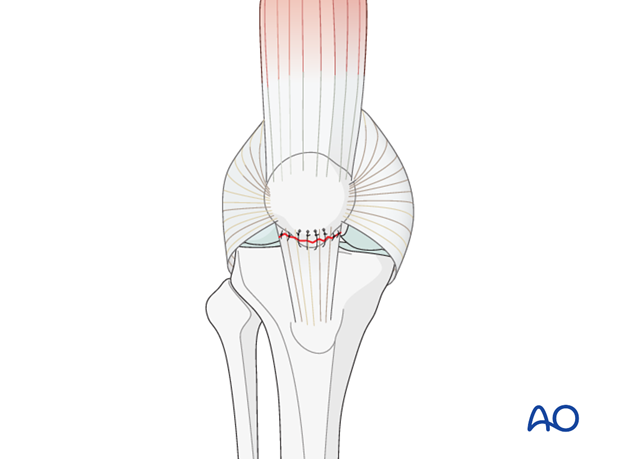
Patellar tendon repair
If the patellar tendon has been torn from the distal pole of the patella the extensor mechanism must be repaired, to regain active knee extension.
Suture the patellar tendon to the patella with 5 nonabsorbable transosseous sutures.
This repair needs augmentation with a patello-tibial wire because it is never strong enough to sustain knee flexion extension forces.
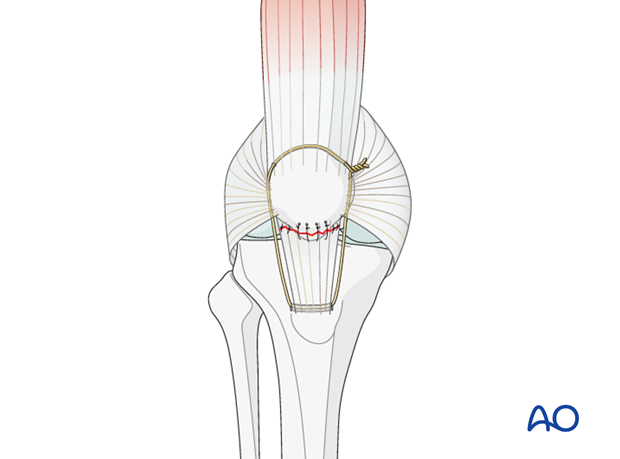
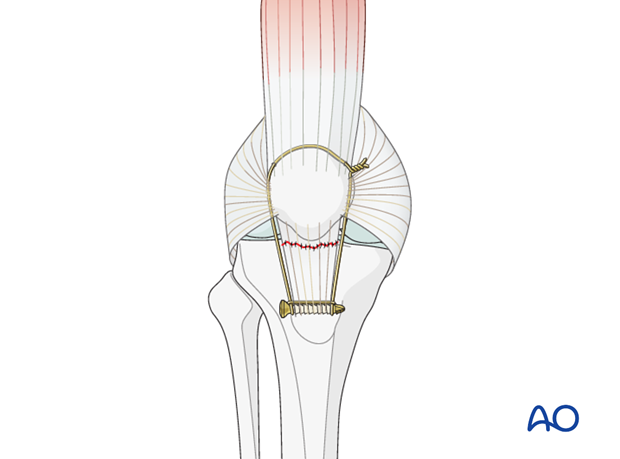
Augmentation using cerclage wire around the patella
After the patellar tendon has been repaired, or if fixation of the patellar tendon origin is inadequate, because of multiple, small fragments, the transosseous sutures must be protected with a cerclage wire between patella and tibial tuberosity.
The anchoring at the tuberosity can be achieved with a simple figure-of-zero cerclage wire through a transverse drill hole just below the tibial tuberosity.
When tightening the loop, it is necessary to ensure that the knee can flex at least to 90°. This means that in full extension there will be some laxity of the cerclage wire.
The same technique can also be used in very small avulsion fractures.
Protection wire in place postoperatively in a patient with a multifragmentary inferior pole of patella where the tendon was stitched back to the patella. The wire protects the soft tissue repair.
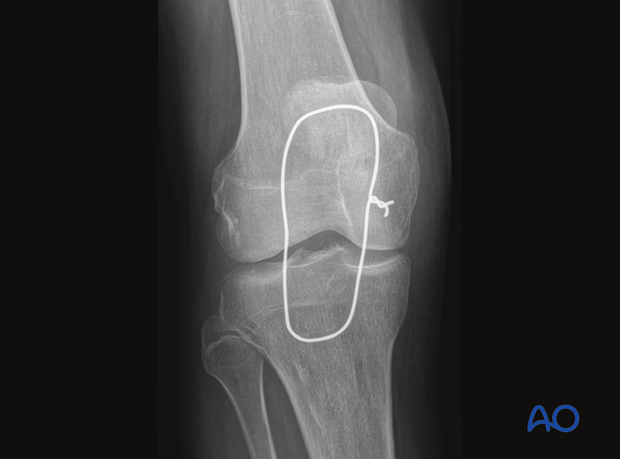
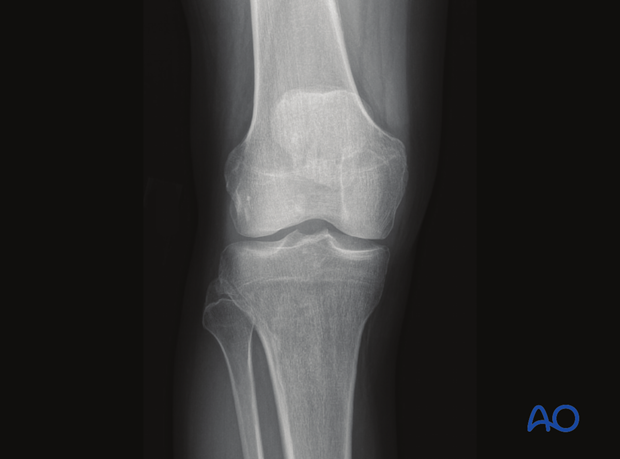
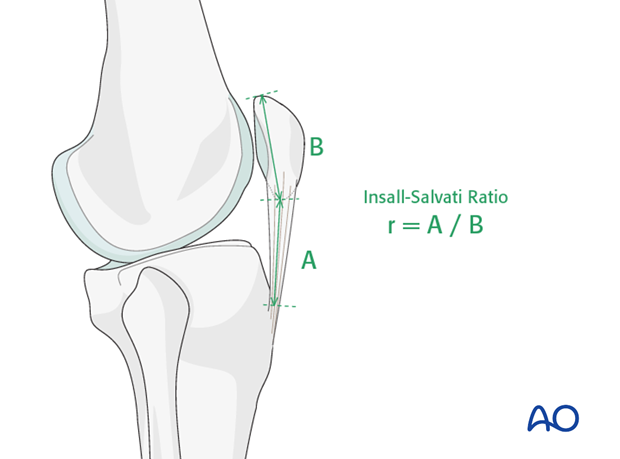
This image shows the inferior multifragmentary pole of patella has been removed. The tendon has been stitched with the appropriate of patella height using the Salvati ratio.
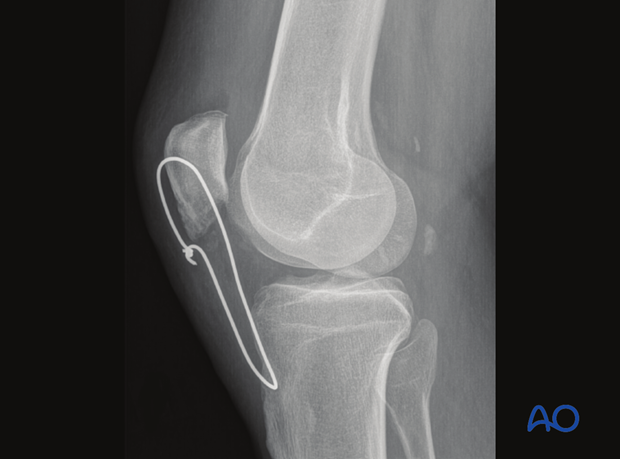
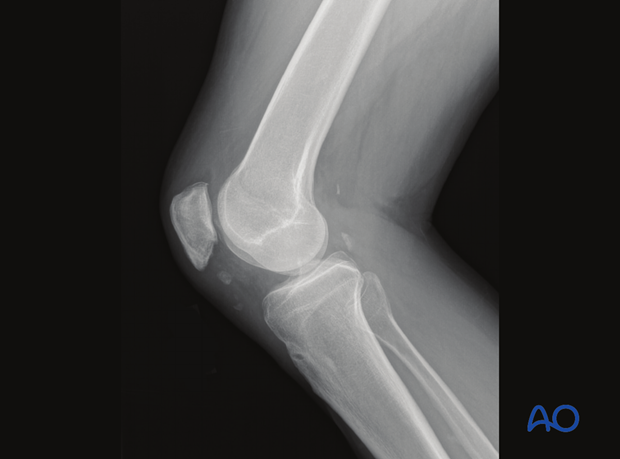
Three months later the wire was removed with the healed tendon ready to take more biologic forces without protection.
Three months lateral X-ray showing a well-positioned patella after patellar tendon reconstruction and protection wire placement (wire has been removed at three months).
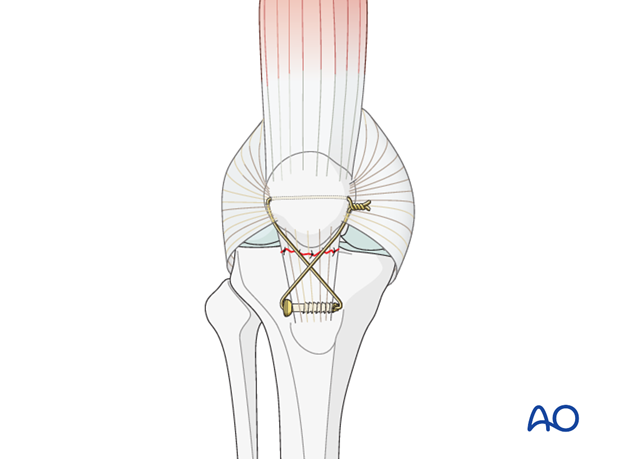
As an alternative in osteoporotic bone, the anchorage at the tuberosity can be achieved around a 3.5 mm cortex screw, or through the hole of a cannulated screw.
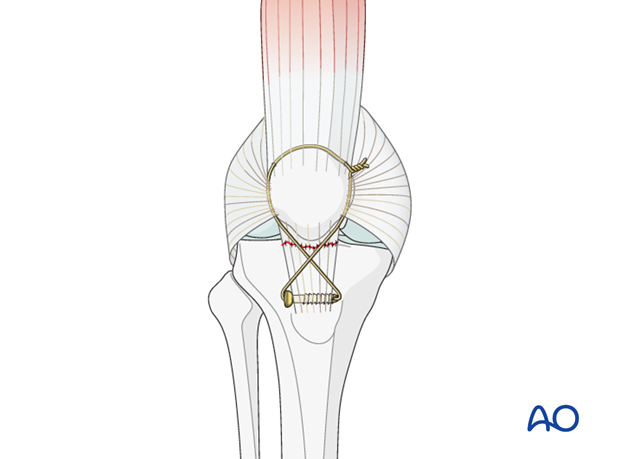
It is the surgeon’s decision whether a figure-of-zero, or figure-of-eight, loop is made, based on personal experience and preference.
Pitfall: If the cerclage wire is tensioned too tightly it will not be possible to flex the knee and a patella baja will occur.
This complication must be avoided as it can cause severe limitation of knee flexion and anterior knee pain. If there is need for a cerclage wire to protect the patellar tendon, a patella baja can be produced by misjudging the exact length of the patellar tendon. The opposite knee will indicate the correct position of the patella, as revealed by x-ray evaluation.
Augmentation using cerclage wire through the patella
Use a patellotibial cerclage wire between the patella and tibial tuberosity to augment the repair. The anchoring at the tuberosity can be achieved around a 3.5 mm cortex screw, or through the hole of a cannulated screw. When tightening this, ensure that the knee is able to flex to 90°. This means that in full extension there will be some laxity of the cerclage wire.
Pearl: One way to ensure that the patellofemoral biomechanics are restored to more functional normality is to position the cerclage wire in a more anatomical position. It is preferable to pass the cerclage wire transversely through the middle, or lower, third of the patella. If the cerclage wire is passed over the proximal pole of the patella this tends to cause increased patellofemoral flexion load, which may lead to anterior knee pain.
5. X-ray control
The result is checked in the AP and lateral planes using an image intensifier.
After a patellar tendon repair, a lateral X-ray should be taken and compared to the normal knee to ensure patellar height is very similar to the uninjured knee.
6. Aftercare following suture anchor fixation
Introduction
Active knee function requires an intact knee extensor mechanism, a mobile patella, a well-preserved patello-femoral joint and muscle strength.
After satisfactory reduction and fixation of patellar fractures, early controlled range of motion exercises are combined with static quadriceps strengthening exercises. The progressive increase in loading of the patello-femoral joint depends on many factors and requires planned individual programs, designed by the surgeon and physical therapists.
Functional treatment
Static isometric quadriceps exercises should be started on postoperative day 1 with the splint in place.
The fixation between the patellar tendon and the patella is not as stable as bony fixation. Because of this tenous fixation, generally with this condition, the knee is kept in full extension for at least four weeks. If the knee is mobilized too quickly then the soft tissue repair is at risk for loosening and patella alta is the result. After four weeks the knee is carefully removed from the extension splint and flexion is begun.
Afterwards, special emphasis should be given on active knee and hip movement.
Weight bearing
A full extension knee splint is applied and worn until at least four weeks. Full weight bearing may be performed with a straight knee, using crutches or a walker, from postoperative day 1.
Follow-up
Wound healing should be assessed regularly during the first two weeks. X-rays should be taken at 2, 6 and 12 weeks. A longer period may be required if tendon healing is delayed.
Knee flexion will return as long as 90° is obtained by three months.













