Patellar plating
1. Principles
The patello-femoral joint is biomechanically very stressed when the knee is loaded. Any compromise of the joint surface is likely to lead to degenerative joint disease. It is, therefore, highly desirable, in patellar fractures to strive for anatomical reduction of the joint surface and stable fixation.
An additional treatment goal is restoration of function of the knee extensor mechanism and allow early range of motion of the knee.
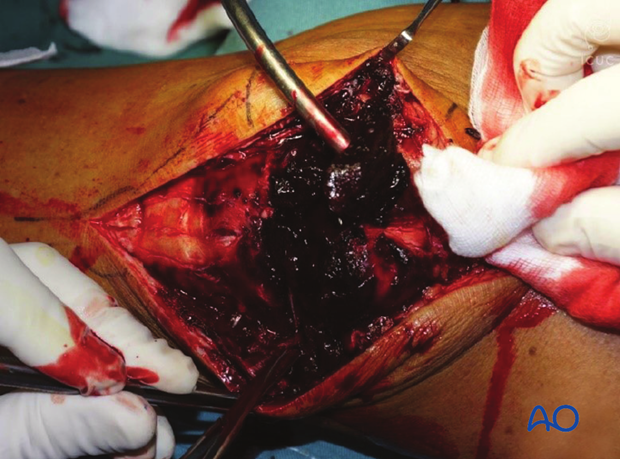
Debridement
The knee joint and fracture lines must be irrigated and cleared of blood clot and small debris to allow exact reconstruction.
2. Patient preparation and approach
Patient preparation
This procedure is normally performed with the patient in a supine position with the knee flexed 30°.

Approach
For this procedure a mid-axial longitudinal approach is used.

3. Reduction and fixation
Reduction and temporary fixation
The reduction of this fracture requires careful planning.
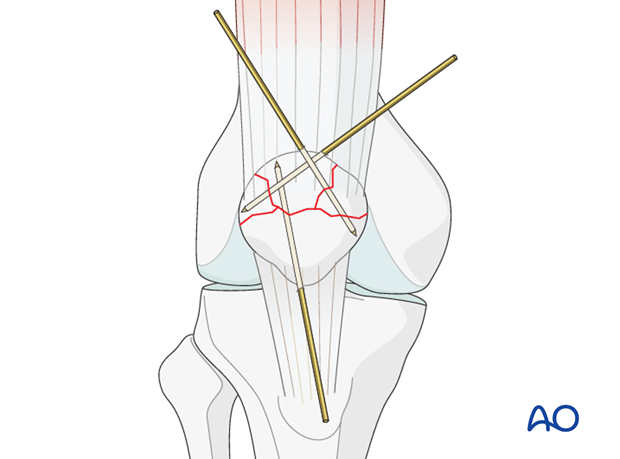
The largest fragments are reduced and temporary fixed with K-wires.
In frontal/coronal (transverse) fractures, reduction is easier with the knee extended.
Sagittal fractures are more easily reduced with the knee flexed.
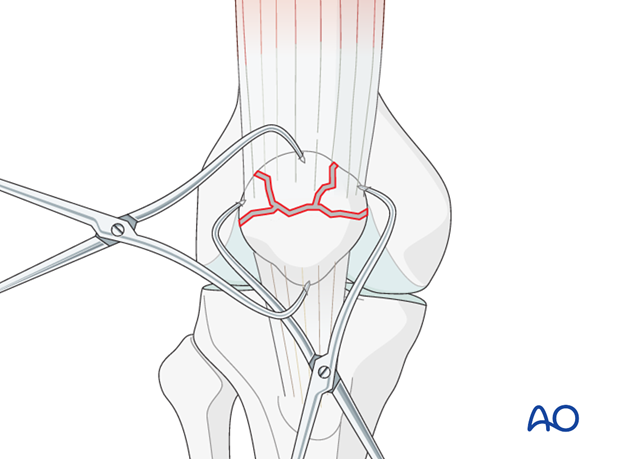
Frequently, the use of several K-wires is required to hold smaller fragments to the larger fragments.
Verify the reduction by palpation of the retropatellar surface.

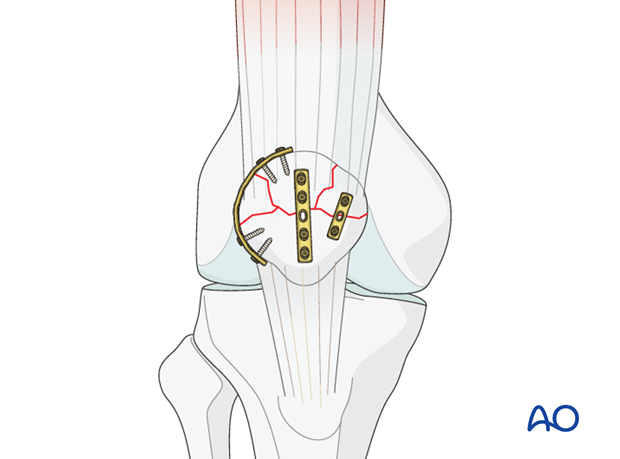
Plate application
Non-locking 2.4 and 2.7 plates are typically used for the patella. They are small and very malleable which facilitates contouring to the patella surface.
The plates can be used circumferentially around the patella, in a similar fashion to a cerclage wire, or across the surface to resist distraction forces.
Each piece of the comminuted patella will require at least one point of fixation if not more.
The resulting construct should be strong enough for early motion to be started.
Care should be taken to prevent screw penetration into the joint.
Reduction should be verified by careful intraoperative X-ray and finger palpation.
Additional stability
To achieve a satisfactory stability, the combination with multiple techniques including lag screws, lag screws through a plate, and K-wire fixation with or without cerclage may be needed.
4. Case
These are preoperative X-rays in a 25-year-old female injured in a motorcycle crash.
Note the extensive multifragmentary fracture pattern on the AP.

The multifragmentary pattern can also be seen in the lateral view.

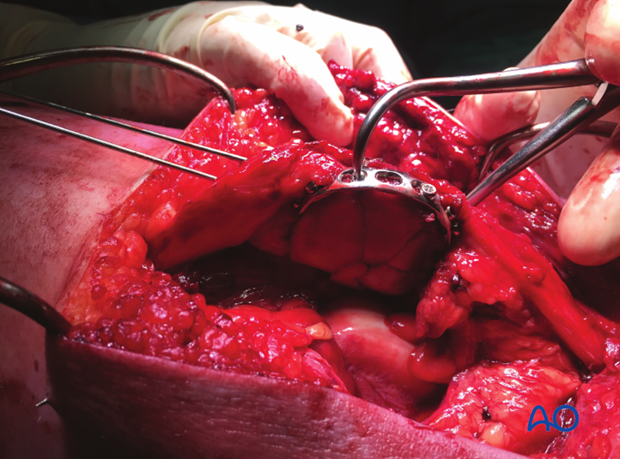
This clinical picture is in the middle of the operating procedure. Note the stellate fracture pattern on the undersurface of the patella as this fracture is approached from the lateral parapatellar approach.
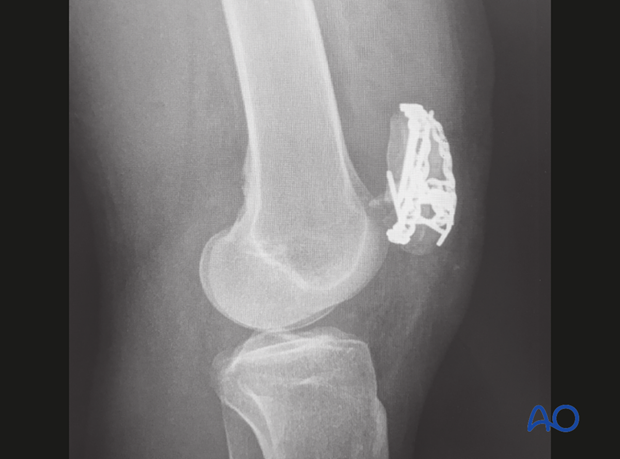
AP postoperative X-ray image demonstrating dorsal and circumferential plating of the multifragmentary patella fracture.

The same patient with the lateral image demonstrating multiple plates and the best possible articular reconstruction for this multifragmentary fracture.
Clinical video of 25-year-old patient three months after patellar plating, demonstrating excellent function of the extensor mechanism.
5. Aftercare following cerclage compression wiring/lag screw/plate fixation of the patella
Introduction
Active knee function requires an intact knee extensor mechanism, a mobile patella, a well-preserved patello-femoral joint and muscle strength.
After satisfactory reduction and fixation of patellar fractures, early controlled range of motion exercises are combined with static quadriceps strengthening exercises. The progressive increase in loading of the patello-femoral joint depends on many factors and requires planned individual programs, designed by the surgeon and physical therapists.
Functional treatment
Patellar fixation is generally quite stable. Early progressive, active mobilization is beneficial after surgery. Despite, wearing a splint to protect against never losing complete extension, range of motion is done throughout the day with the splint off. Static isometric quadriceps exercises should be started on postoperative day 1 with the splint in place. Usually the anterior incision is slow to heal as it is over a flexion surface and so it is usually best to leave the knee in extension for at least a week.
Afterwards, special emphasis should be given on active knee and hip movement.
Weight bearing
A removable full extension knee splint is applied and worn until good quadriceps control is regained. Full weight bearing may be performed with a straight knee, using crutches or a walker, from postoperative day 1.
Follow-up
Wound healing should be assessed regularly during the first two weeks. X-rays should be taken at 2, 6 and 12 weeks. A longer period may be required if fracture healing is delayed.
Implant removal
Implant removal may be required, as the wires may be prominent under the skin. Implant removal should not be undertaken until a minimum of 1 year postoperatively.
Thrombo-embolic prophylaxis













