Lag-screw fixation
1. General considerations
Introduction
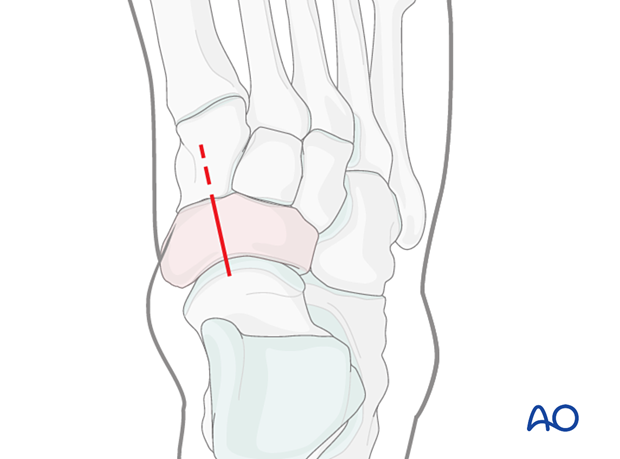
The typical simple navicular fracture is longitudinal split.
Goal of surgery
The main goals of the surgery are to:
- Retain talonavicular joint function
- Restore the length of the medial column
- Achieve the above without compromising the blood supply of the navicular
Timing of surgery
The timing of surgery is influenced by the soft tissue injury and the patient's physiologic status.

2. Screw selection
For the procedure, a range of screws can be utilized:
- Cannulated screws
- Non-cannulated screws
- Headless compression screws
We will here demonstrate the use of cannulated and non-cannulated screws.

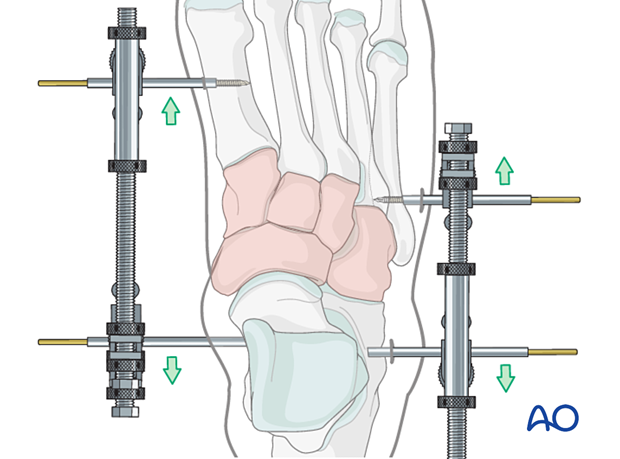
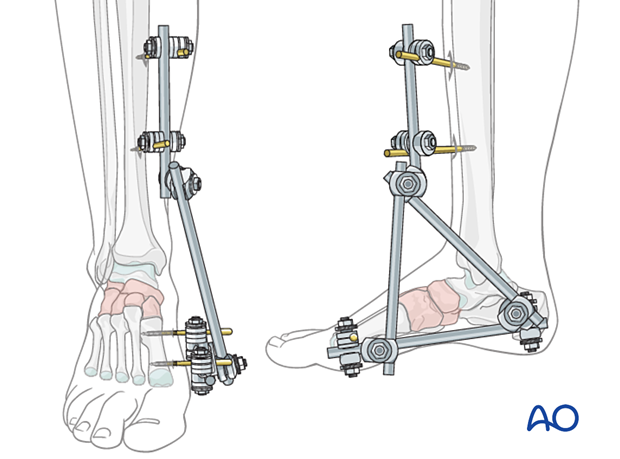
3. Temporizing measures
Medial and lateral external fixation (with a distractor device to restore columnar length) should be applied as soon as possible to stabilize the foot and decrease further injury to the soft tissues.
Temporary percutaneous K-wires can be used to reduce displaced fragments and are left as temporary fixation.
Temporary cross ankle external fixation from the distal tibia to the metatarsals may be needed to allow for any extensive swelling in the foot to subside.
4. Patient preparation and surgical approach
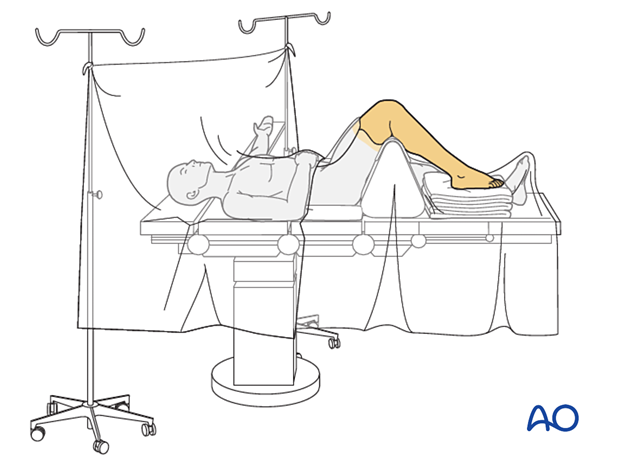
The procedure is performed with the patient placed supine with the knee flexed 90°.
A limited dorsomedial approach is made directly over the fracture without peripheral dissection and undermining, maintaining the blood supply.
The fracture is entered directly and dealt with as necessary.
5. Reduction
Distraction
Both articular surfaces require visualization for accurate reduction and fixation.
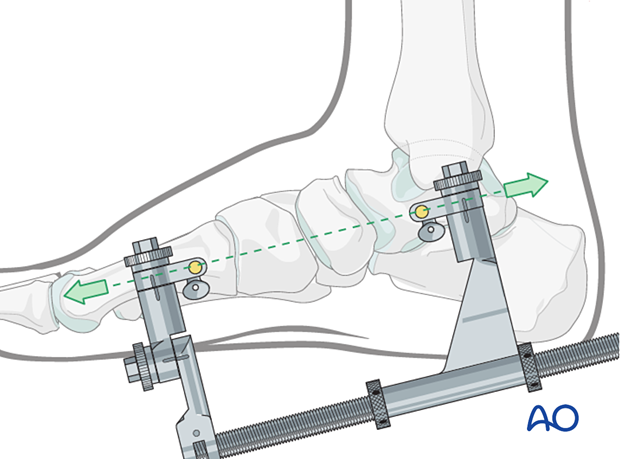
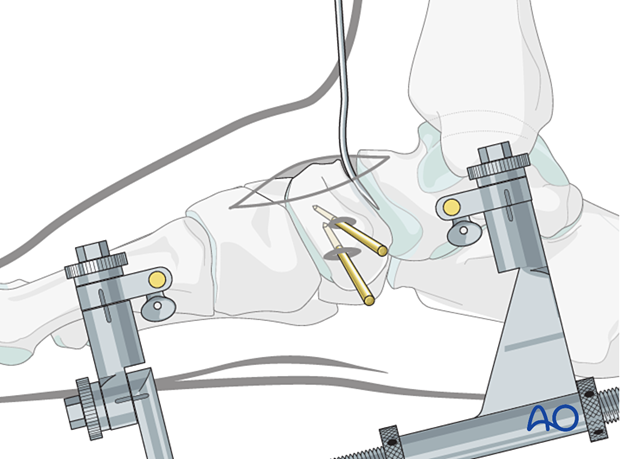
A medial-column distractor can be used.
The proximal pin is inserted into the neck of the talus through a stab incision. Image intensification can be used to ensure correct pin placement outside the articular surfaces. The correct insertion point is often located 1–2 cm posterior to the navicular tubercle.
The distal pin is inserted in the first metatarsal.
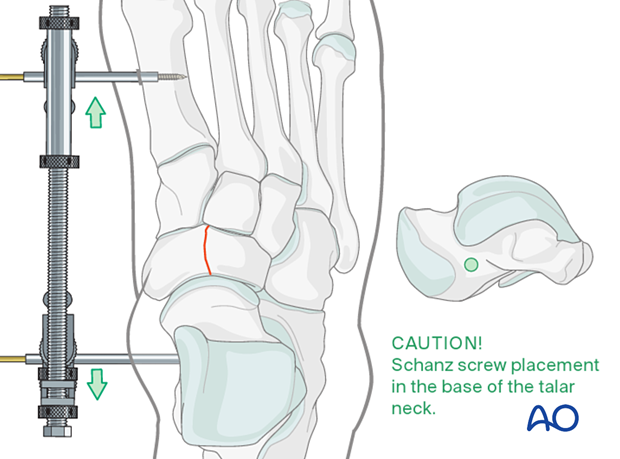
The distraction vector needs to be in line with the talus and the first metatarsal in the medial plane.
Reduction
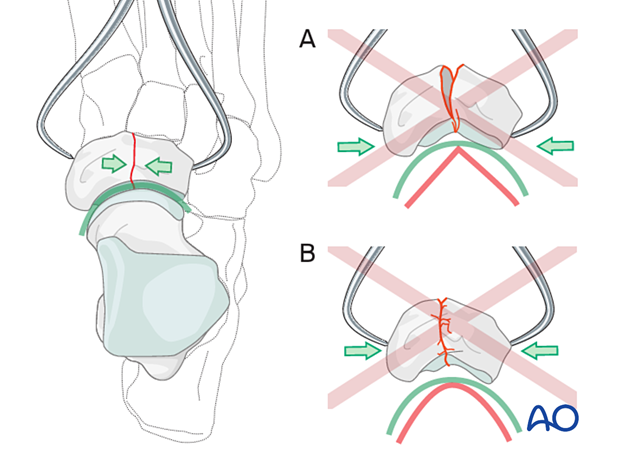
Insert the pointed reduction forceps through two small stab incisions placed dorsomedially and dorsolaterally.
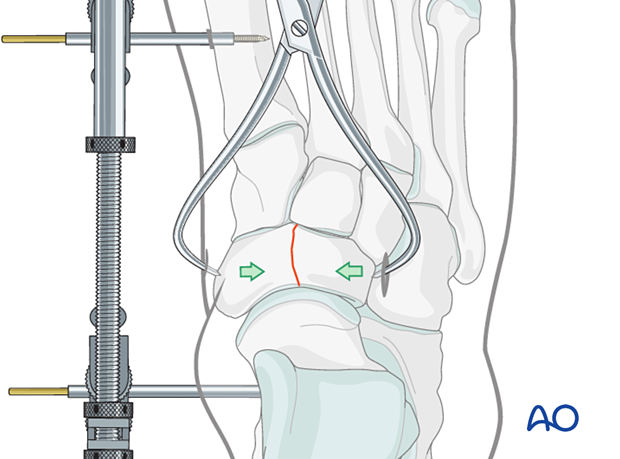
When treating fractures of the navicular, it is essential to pay attention to its concavity.
The reduction forceps tips should be positioned in such a way as to provide even compression across the fracture. Proximal positioning of the tips may lead to malreduction (A).
Reduce the fracture carefully. Do not overcompress since this will destroy the anatomical concavity of the joint surface (B).
Preliminary K-wire fixation
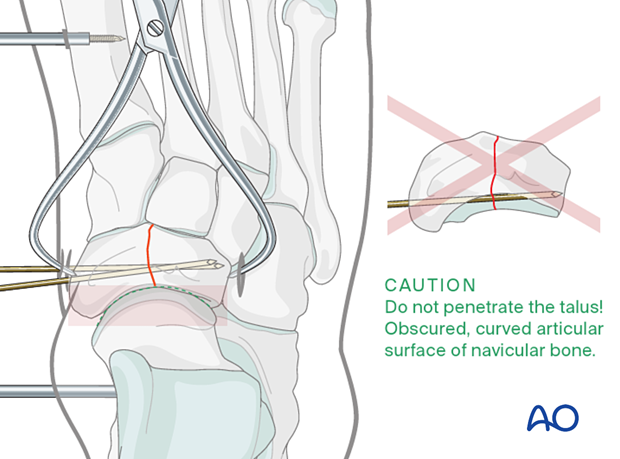
Often provisional K-wire fixation is necessary since the tip of the reduction clamp is placed precisely where you want to insert the lag screw.
If cannulated screws are used, the guide wires can be used for provisional fixation. Care must be taken in terms of K-wire trajectory to avoid joint penetration of the concave articular surface of the navicular.
If solid screws are to be used, be sure to place the K-wires so that they will not interfere with the subsequent screw placement.
Check reduction
Ensure that the joint is anatomically reduced. The reduction can be inspected under direct vision if the joint has been correctly distracted.
The articular surface congruity can be palpated with an elevator inserted dorsally if direct vision is impossible.
Also, use image intensification to check your reduction.
The resolution of the image intensifier may not be sufficient to appreciate small joint incongruities. If in doubt, get intraoperative x-rays.
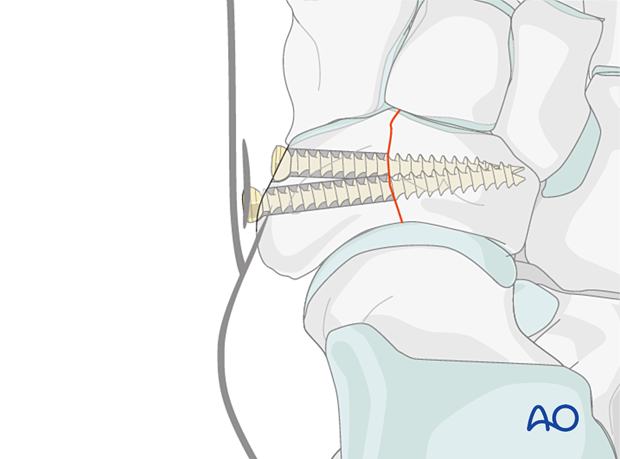
6. Fixation
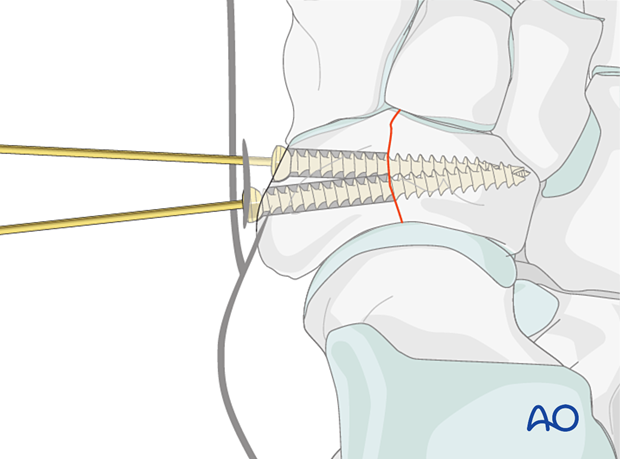
Use an image intensifier to verify the appropriate screw length.
Insert the proximal lag screw according to the standard technique. In contrast to lag screws inserted in the diaphysis, these lag screws will typically not penetrate the far cortex, as this would damage the opposite articular surface.
Afterward, insert a second lag screw in the same fashion.
The screws may be non-cannulated, cannulated, or headless compression screws.
If the bone is osteoporotic, insert a washer under the screw head to prevent it from sinking into the bone.
Remove the K-wires.
7. Aftercare
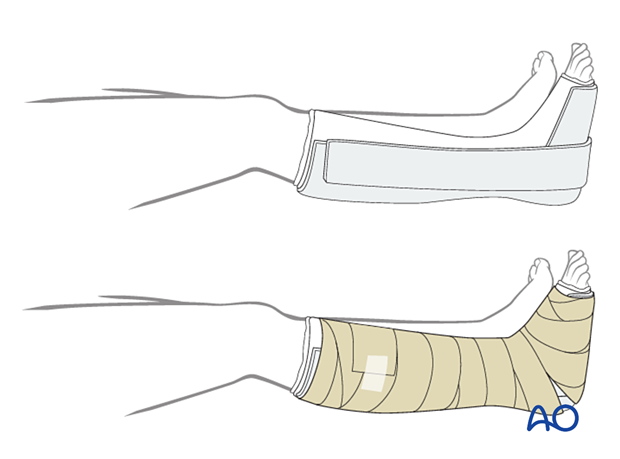
Dressing
The non-adherent antibacterial dressing is applied as a first layer. Sterile undercast padding is placed from toes to knee. Extra side and posterior cushion padding are added.
Immobilization
The foot should be immobilized for the first two weeks, which can be achieved using a three-sided plaster splint. The anterior area is left free of plaster to allow for swelling. Ensure that the splint’s medial and lateral vertical portions do not overlap anteriorly and that the splint does not compress the popliteal space or the calf.
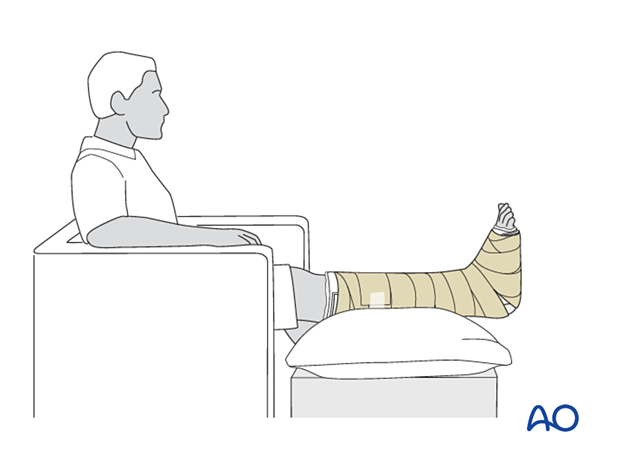
Follow-up
The patient should be counseled to keep the leg on a cushion and elevated. Remember not to elevate the leg too much as it may impede the inflow. The foot’s ideal position is halfway between the waist and the heart when the patient is sitting. While seated, the foot should be on a cushion and elevated, but if badly swollen, the patient must be supine since elevating the foot while seated decreases swelling less effectively.
Avoid direct pressure against the heel during recumbency to prevent decubiti.
The OR dressing is usually left in place and not changed until the first postoperative visit at two weeks when x-rays are obtained once the dressing is removed. If any complication is suspected (eg, infection or compartment syndrome), the dressing must be split and, if necessary, removed to allow full inspection.
The strict non-weight bearing should be maintained until there is evidence of healing and any transfixion K-wires (6–12 weeks) or bridging devices (min 12 weeks) are removed.
Daily toe movement is encouraged.
Formal physical therapy should not begin in the early postoperative period.
A gastrocnemius release may need to be performed in cases with postoperative gastrocnemius contracture. This occurs more typically in the mid and hind-foot.













