Primary fusion of naviculocuneiform joint
1. General considerations
Goal of surgery
The main goals of the surgery are to:
- Retain talonavicular joint function via an anatomic reduction of the navicular fracture and surrounding joints
- Restore the length of the medial column
- Achieve the above without compromising the blood supply of the navicular
Principles
Fusion of the navicular can generally be divided into six main steps.
- Reconstruction of the talonavicular joint surface using lag screws and/or K-wires (if needed)
- Preparation of the cuneiform articular surface for fusion
- Restoration of medial column length
- Application of hardware to secure the reconstruction and maintain column length (if possible)
- Grafting to fill any defects (if needed)
- Temporary bridging to support reconstruction until healing (if badly comminuted)
In the ideal case:
- The articular surface can be reconstructed using lag screws
- The length of the navicular is maintained using a navicular plate without fusion or bridging of any joint
In cases of severe comminution or when the articular fixation is only secured with K-wires or pins, the reconstruction can be protected using a bridging device until the fracture is healed.
A bridging device is also utilized if the articular surface is reconstructed, but a navicular plate cannot be applied to secure the medial column length.
Timing of surgery
The timing of surgery is influenced by the soft tissue injury and the patient's physiologic status.

Talonavicular joint function
It is crucial to retain TN function as loss of motion:
- Results in loss of complex hindfoot circumduction
- Leads to adjacent joint degeneration (DJD)
Retaining even a small amount of motion is thought to protect the adjacent joint function.
Because of its extensive range of motion, the TN joint is also known as the “coxa pedis.”

Maintenance of column length
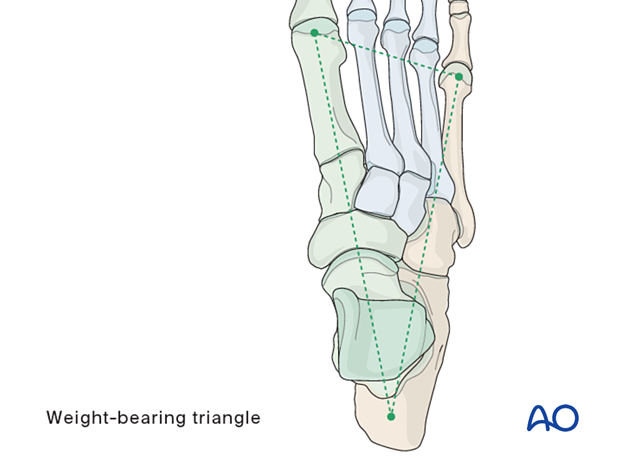
The foot’s form and function depend on the normal relationship between the medial and lateral columns.
Relative shortening of the medial column leads to cavus, whereas relative shortening of the lateral column leads to flat-foot.
If the injury has resulted in comminution with loss of medial or lateral column length, this length and normal geometry must be restored.
Bridging hardware and bone graft will assure proper column length, overall shape, and alignment of the foot.
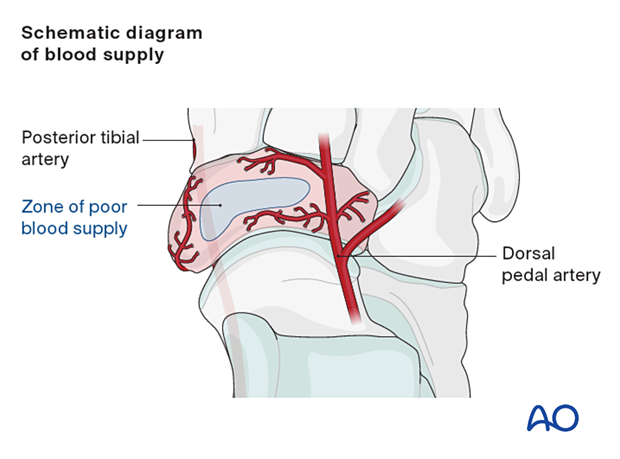
Navicular blood supply
The navicular has an oval shape. Small branches of the posterior tibial and dorsal foot arteries comprise the blood supply of the navicular. The medial and lateral areas are more or less well supplied, while the central section has the most marginal blood supply.
2. Temporizing measures
Medial and lateral external fixation (with a distractor device to restore columnar length) should be applied as soon as possible to stabilize the foot and decrease further injury to the soft tissues.
Temporary percutaneous K-wires can be used to reduce displaced fragments and are left as temporary fixation.
Temporary cross ankle external fixation from the distal tibia to the metatarsals may be needed to allow for any extensive swelling in the foot to subside.
3. Patient preparation and surgical approach
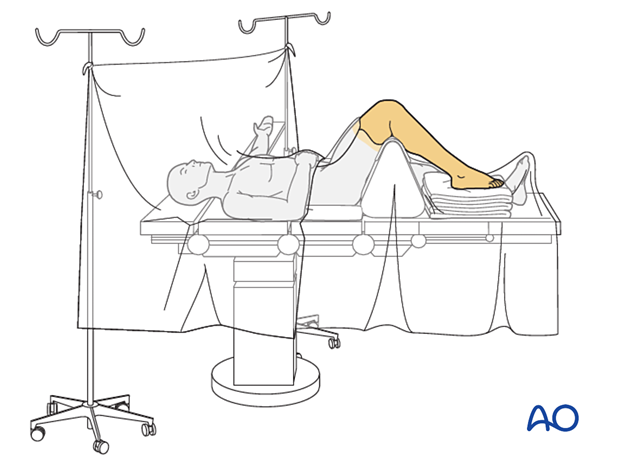
The procedure is performed with the patient placed supine with the knee flexed 90°.
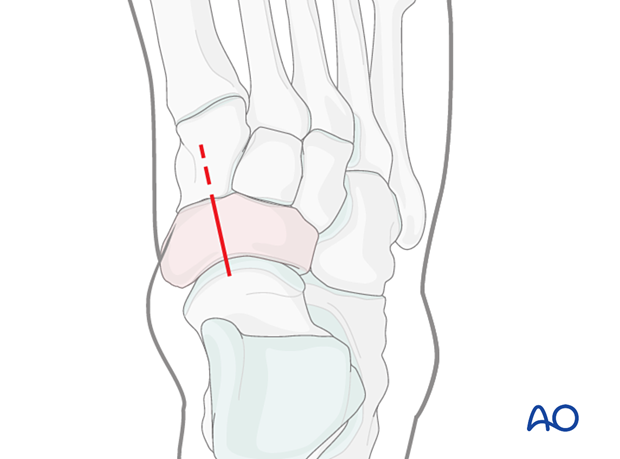
For this procedure, a dorsomedial approach to the navicular is used.
Due to the high-energy injury of these fractures, the soft tissues, including the capsule and periosteum, are disrupted. Care should be taken to minimize soft-tissue stripping during the approach to maintain blood supply to the fragments.
4. Visualization
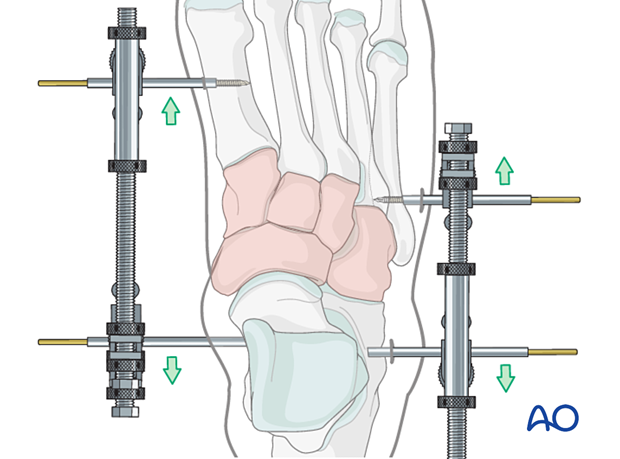
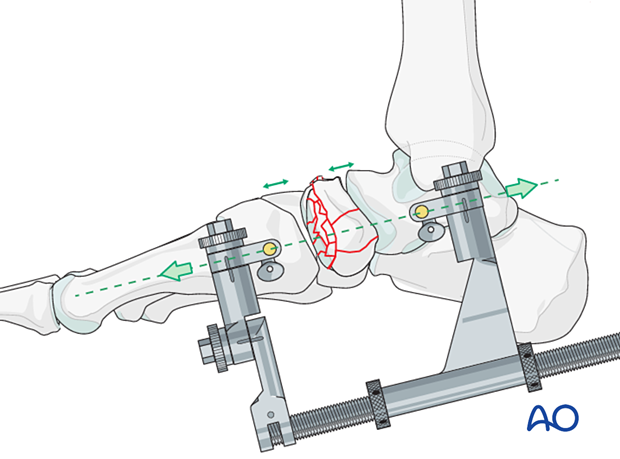
Distraction
Use a medial-column distractor to achieve articular surface visualization needed for accurate reduction and fixation.
Distraction is essential when dealing with comminution or a delay between the injury and the definitive reduction.
The proximal pin is inserted into the neck of the talus through a stab incision. Image intensification can be used to ensure correct pin placement outside the articular surfaces. The correct insertion point is often located 1–2 cm posterior to the navicular tubercle.
The distal pin can either be inserted in the medial cuneiform (and potentially into the middle cuneiform for extra purchase or the first metatarsal.
The distraction vector must be in line with the talus and the first metatarsal in the medial plane to maintain the medial column alignment.
The fracture is distracted to allow complete visualization of either joint surface as needed.
Debridement
Irrigate the fracture site using, eg, a syringe.
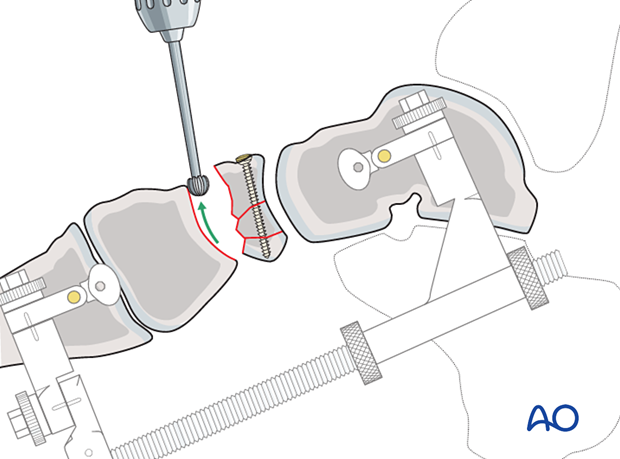
5. Reconstruction of the talonavicular articular surface (if needed)
Use a curved elevator for joint surface reduction and the opposing articular surface(s) as a template.
It may be helpful to have a variety of elevators available to aid reduction.
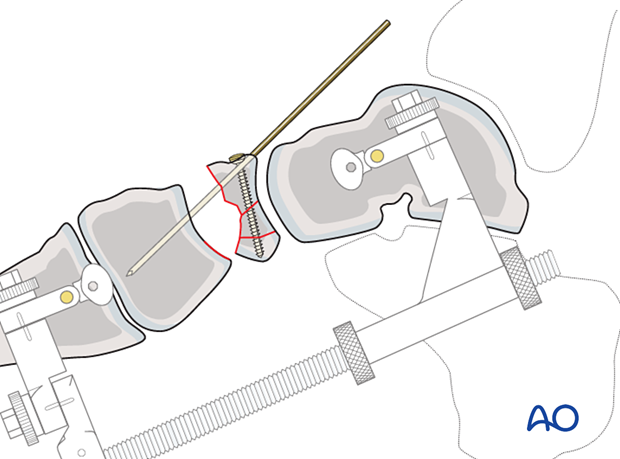
Osteochondral fragments should be salvaged and secured with small lag screws if possible. Before screw fixation, a bone graft can be used to backfill any defect. If screw fixation is not possible, pins or K-wires can be used. K-wires can be cut and left in situ.
Ideally, joint reconstruction should be performed by inserting hardware only into the navicular.
While hardware may be inserted into the cuboid or cuneiforms for added support, mobility of the talonavicular joint should be maintained.
When adjacent joint surfaces are used as a template, verification of the reduction can become problematic if the fragments are fixed with a trans articular K-wire.
While reconstructing the joint surface, frequently check visually and radiographically to ensure no malreduction.
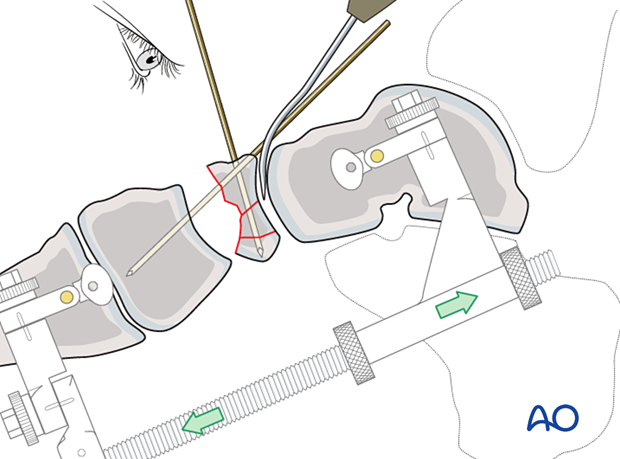
Reduction of dorsal dislocation
When the navicular is dorsally displaced, there will be a lateral plantar “constant” fragment still attached to the “spring ligament.” This fragment serves as a reference point for relocating the dislocated navicular.
The navicular is first reconstructed and then reduced anatomically to the “constant” fragment using reduction forceps. One tine is typically inserted dorsolaterally, and the other is inserted through the medial utility incision above the flexor tendons at the lateral plantar constant fragment. A bone graft can be used to backfill any defect to aid in osteochondral fragment reduction.
Anatomic reduction of a reconstructed navicular to the “constant” fragment ensures the correct reduction of the dorsally displaced navicular fracture.
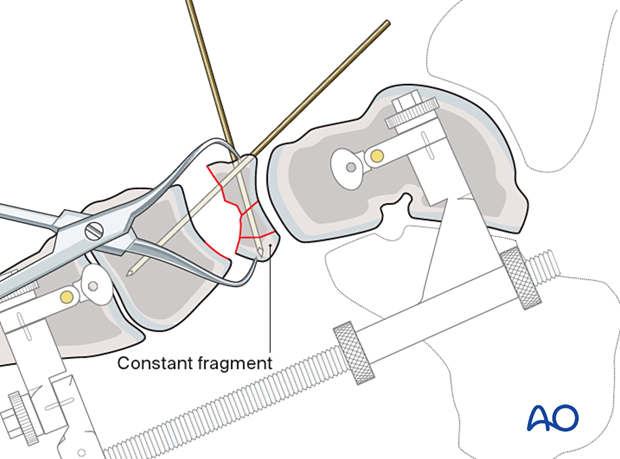
Care must be taken to insert screws through the dorsal reconstructed fragment into the constant plantar lateral fragment.
This is typically the two proximal lateral screws and the distal-most lateral screw. The screws are inserted as position screws.
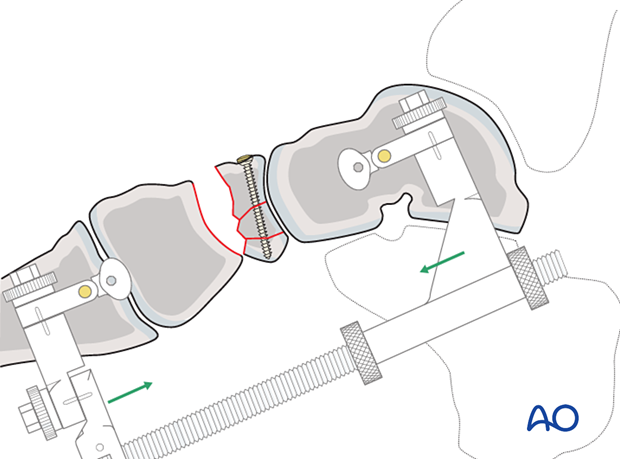
6. Preparation of naviculocuneiform joint for fusion
Once articular surface reconstruction of the talonavicular joint is completed, any fragments with cartilage are removed from the naviculocuneiform joint.
Remove the cartilage of the navicular joint(s) using a curette.
Disrupt the subchondral bone of the cuneiform(s) using a high-speed burr to promote bone growth.
7. Restoration of medial column length
Adjust the distraction to restore the length of the medial column.
It is helpful to have comparative x-rays from the uninjured side, allowing proper length and morphology to be judged.
A bone graft can be used to backfill any defect.
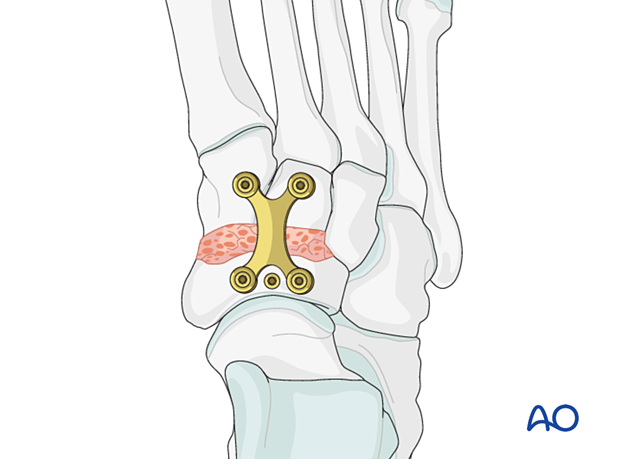
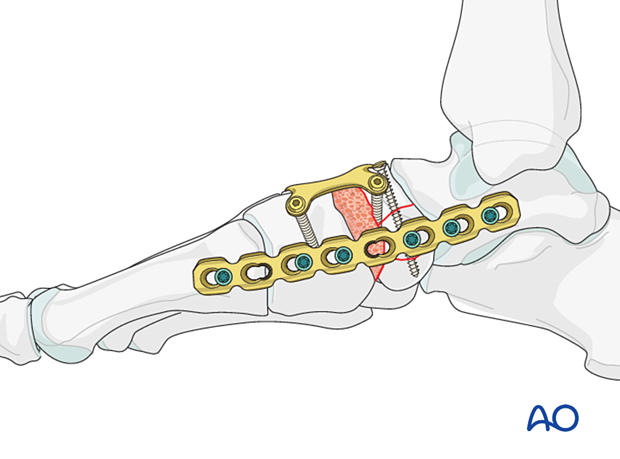
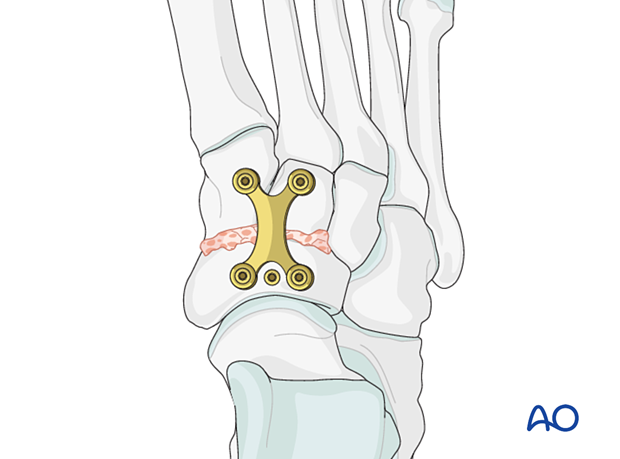
8. Application of fusion plate
A plate is applied between the proximal navicular and the cuneiform.
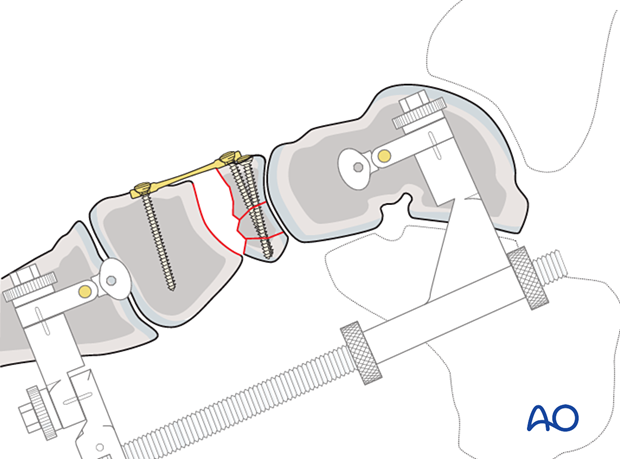
9. Completion of bone grafting
Any remaining bone defect can then be bone grafted using cancellous or corticocancellous bone graft (for structural support) harvested from either the distal or proximal tibia.

Quality control
Using intraoperative imaging, verify:
- Restoration of the appropriate length of the medial column
- Restoration of navicular shape
- Appropriate screw placement and length
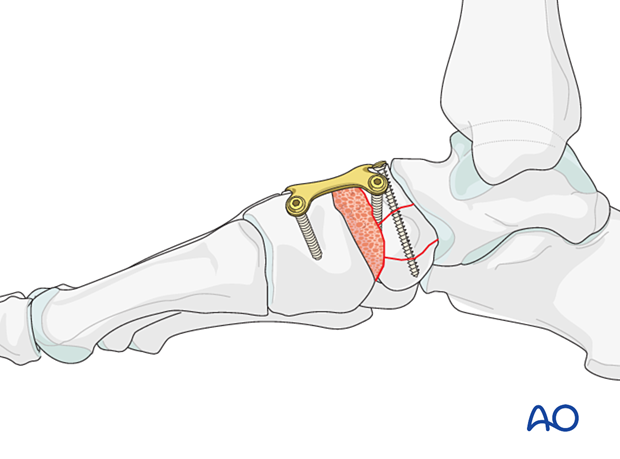
10. Temporary bridging (if needed)
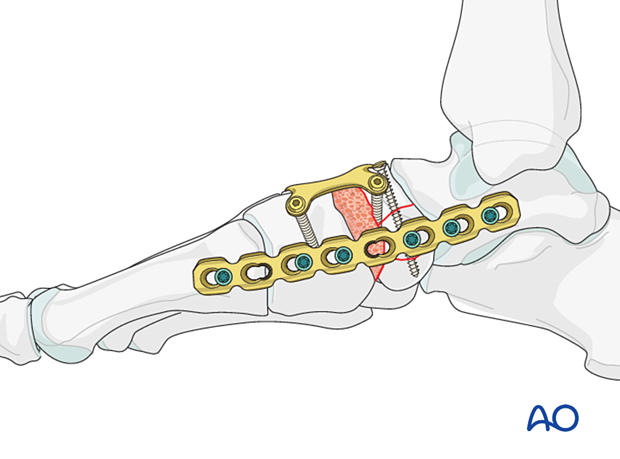
A bridge plate or an external fixator may be used to supplement navicular reconstruction.
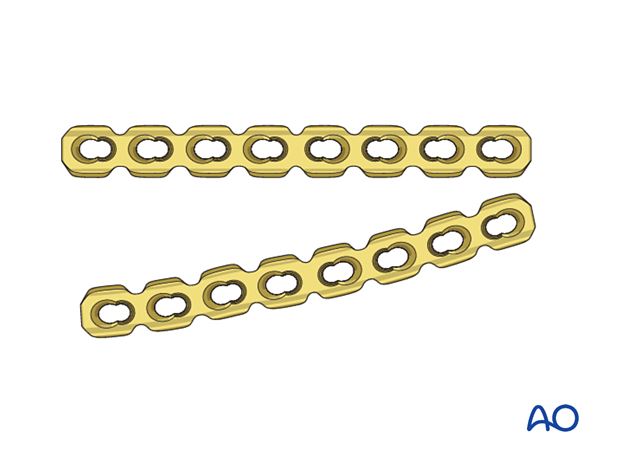
Temporary bridging with a plate
Plating can be performed through the dorsal or medial incision; however, soft-tissue stripping should be avoided.
Extensive dissection can be avoided by sliding the contoured plate subcutaneously along the medial aspect of the foot.

The plate length should allow for fixation using a minimum of two screws both proximally and distally.
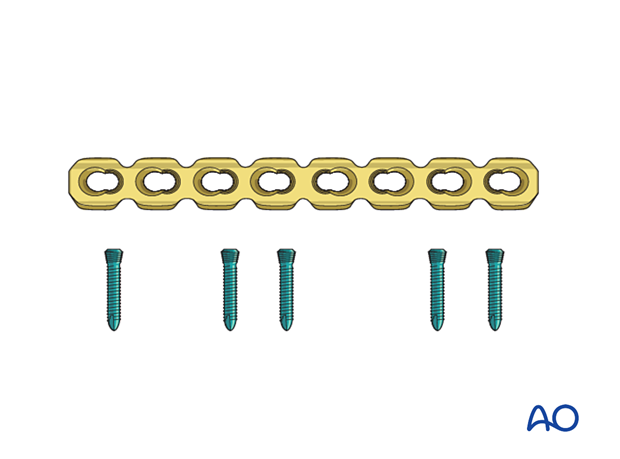
The plate needs to be contoured to achieve a good fit and prevent tenting of the skin.
- In-plane bending to adapt to the arch of the medial foot
- Out of plane bending to adapt to the medial contour of the medial column
- Torquing to fit both the neck of the talus proximally and the medial aspect of the first metatarsal distally
The step-by-step bending procedure is analog to the bending of reconstruction plates.
The plate may be pre-contoured using a saw-bone foot model and fine-tuned in situ as an alternative to using a template.
Fix the bridge plate, using a minimum of two screws proximally (talus) and distally (first metatarsal).
A small medial incision is made to facilitate the insertion of the more proximal screws.
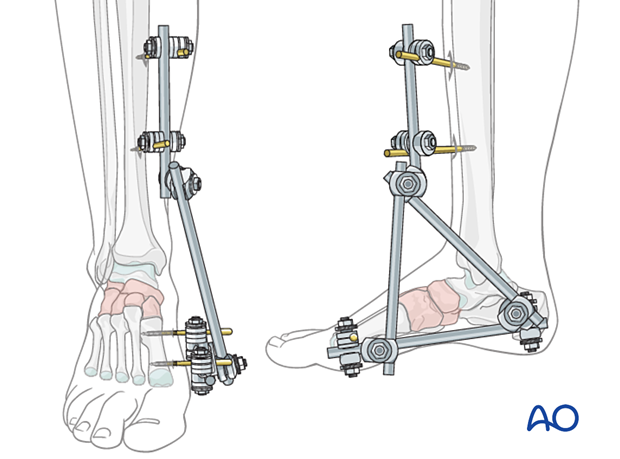
Temporary bridging using an external fixator
The medial column distractor can be replaced with an external fixation construct, which can be left in place while the bone heals instead of bridge plating.
Two bicortical pins are inserted in both the calcaneus and the 1st metatarsal.
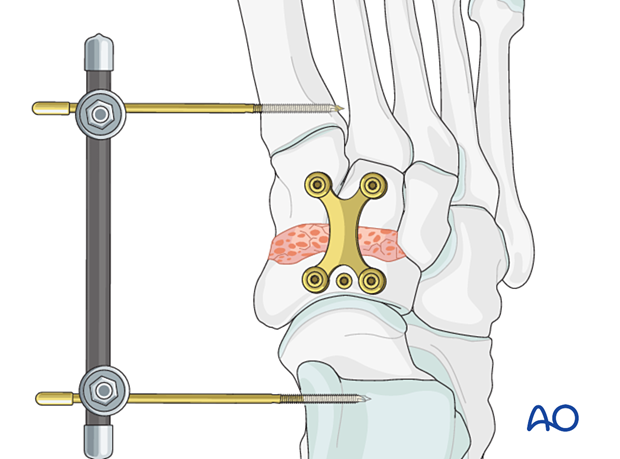
Removal of bridging device
The bridging device should be removed when there is radiographic evidence of navicular healing, typically a minimum of three months.
11. Aftercare
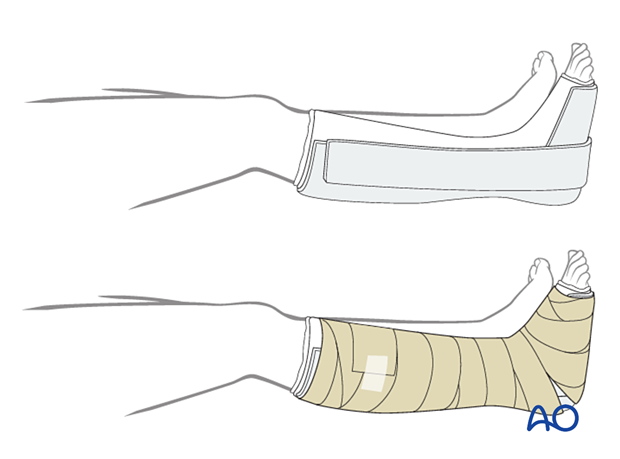
Dressing
The non-adherent antibacterial dressing is applied as a first layer. Sterile undercast padding is placed from toes to knee. Extra side and posterior cushion padding are added.
Immobilization
The foot should be immobilized for the first two weeks, which can be achieved using a three-sided plaster splint. The anterior area is left free of plaster to allow for swelling. Ensure that the splint’s medial and lateral vertical portions do not overlap anteriorly and that the splint does not compress the popliteal space or the calf.
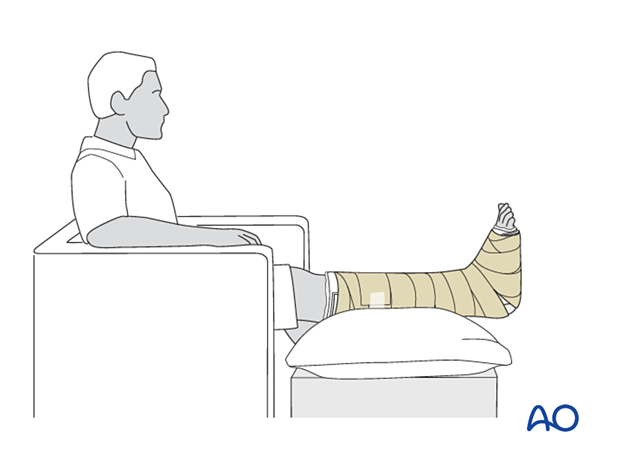
Follow-up
The patient should be counseled to keep the leg on a cushion and elevated. Remember not to elevate the leg too much as it may impede the inflow. The foot’s ideal position is halfway between the waist and the heart when the patient is sitting. While seated, the foot should be on a cushion and elevated, but if badly swollen, the patient must be supine since elevating the foot while seated decreases swelling less effectively.
Avoid direct pressure against the heel during recumbency to prevent decubiti.
The OR dressing is usually left in place and not changed until the first postoperative visit at two weeks when x-rays are obtained once the dressing is removed. If any complication is suspected (eg, infection or compartment syndrome), the dressing must be split and, if necessary, removed to allow full inspection.
The strict non-weight bearing should be maintained until there is evidence of healing and any transfixion K-wires (6–12 weeks) or bridging devices (min 12 weeks) are removed.
Daily toe movement is encouraged.
Formal physical therapy should not begin in the early postoperative period.
A gastrocnemius release may need to be performed in cases with postoperative gastrocnemius contracture. This occurs more typically in the mid and hind-foot.













