Lag-screw fixation
1. General considerations
The goal of the treatment
The goal of the treatment is bone healing with appropriate intra- and extraarticular reduction to maintain lateral column length.
Timing of surgery
The timing of surgery is influenced by the soft tissue injury and the patient's physiologic status.

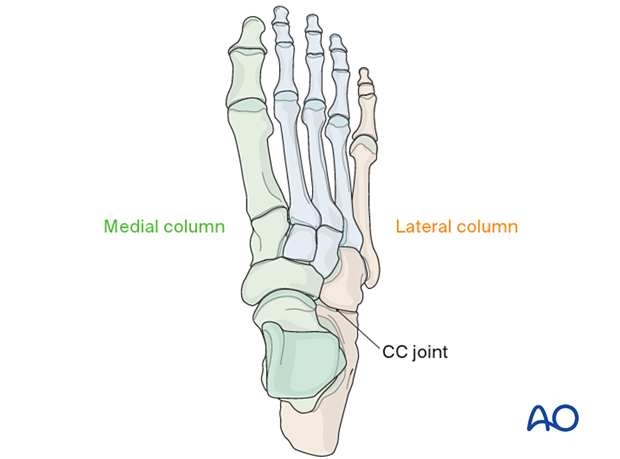
Anatomic function
The calcaneocuboid joint and the talonavicular joints are responsible for complex hindfoot circumduction.
Lateral column length is critical to maintaining the shape and function of the foot. Therefore, the cuboid length must be maintained.
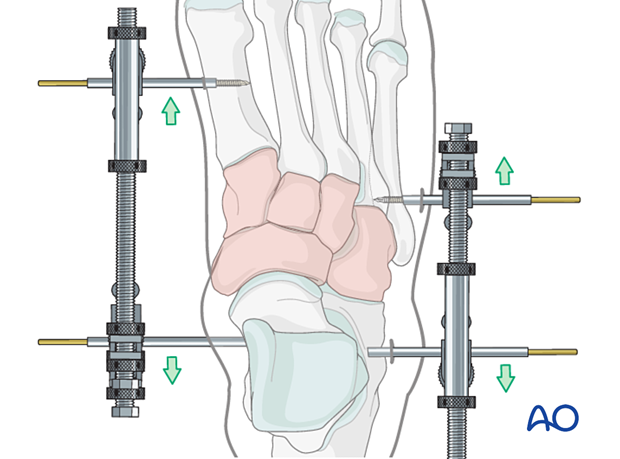
2. Temporizing measures
Medial and lateral external fixation (with a distractor device to restore columnar length) should be applied as soon as possible to stabilize the foot and decrease further injury to the soft tissues.
Temporary percutaneous K-wires can be used to reduce displaced fragments and are left as temporary fixation.
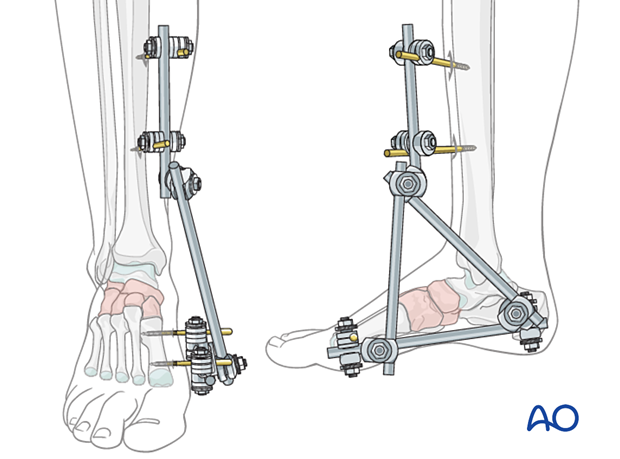
Temporary cross ankle external fixation from the distal tibia to the metatarsals may be needed to allow for any extensive swelling in the foot to subside.
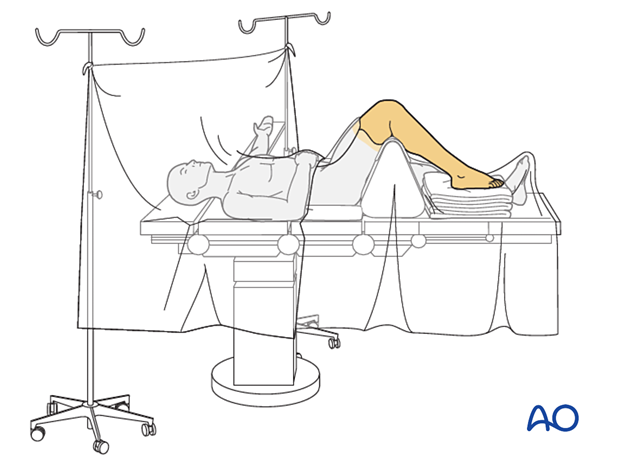
3. Patient preparation and surgical approach
The procedure is performed with the patient placed supine with the knee flexed 90°.
Fractures of the cuboid are best approached through the dorsolateral approach to the cuboid.
The soft tissues, including capsule and periosteum, are often disrupted. Care should be taken to minimize soft-tissue stripping during the approach, which will help maintain the blood supply to the fragments.
4. Reduction and temporary fixation
Debridement
Irrigate and debride the fracture site using a syringe or a curette.
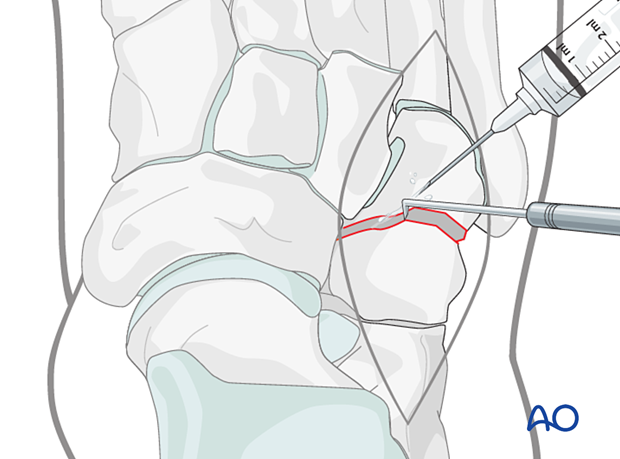
Reduction
Reduce the fracture using small pointed reduction forceps.
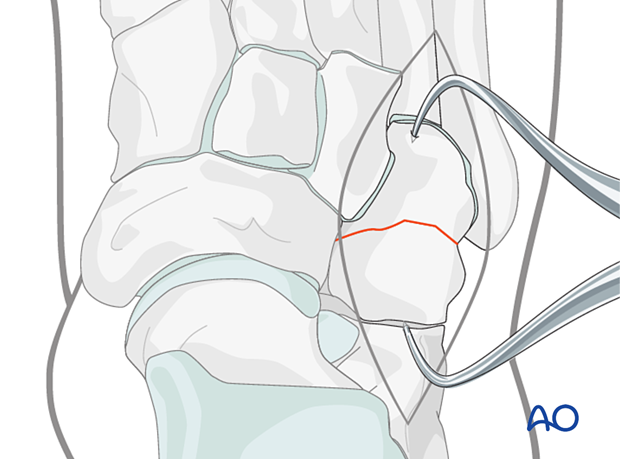
Temporary fixation
Insert two K-wires to secure the reduction.
If cannulated screws are used, the guide wires can be used for provisional fixation.
If solid screws are to be used, be sure to place the K-wires so that they will not interfere with the subsequent screw placement.
5. Fixation
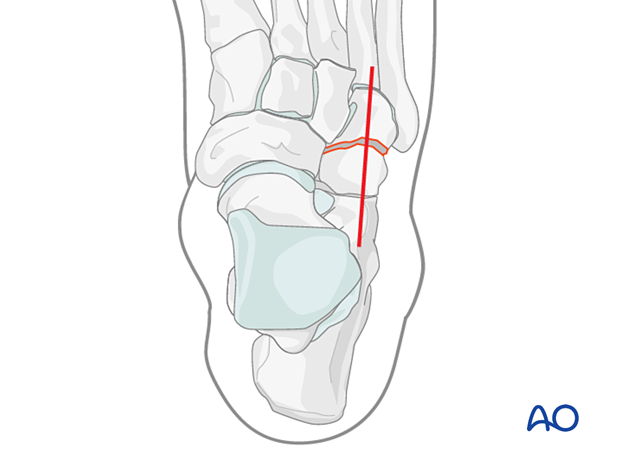
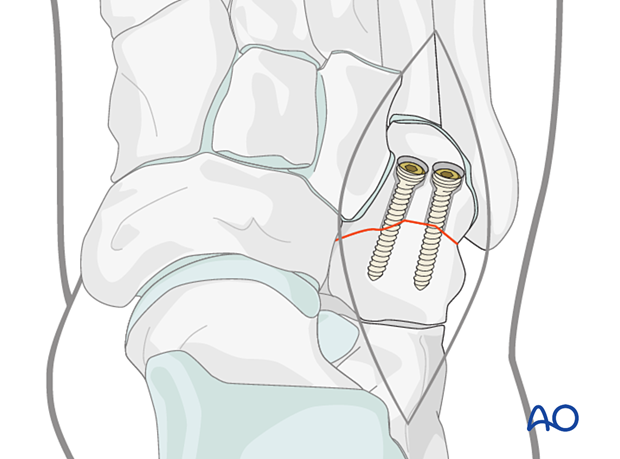
Screw trajectories
Given the cuboid’s shape, the choice of screw trajectory is limited, and it may not be possible to insert the lag screw perpendicular to the fracture plane.
These fractures can be fixed with crossing screws, usually from distal to proximal.
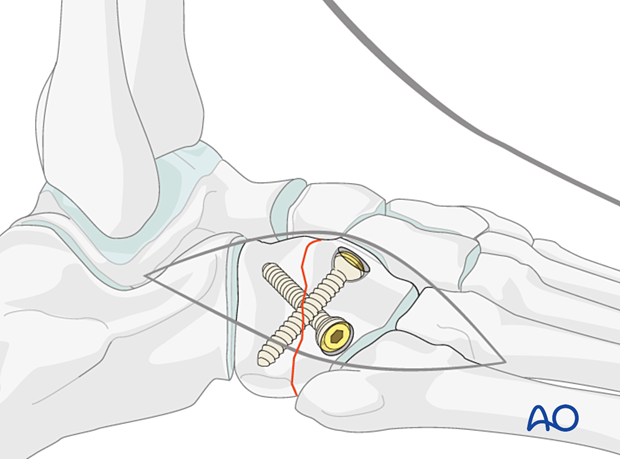
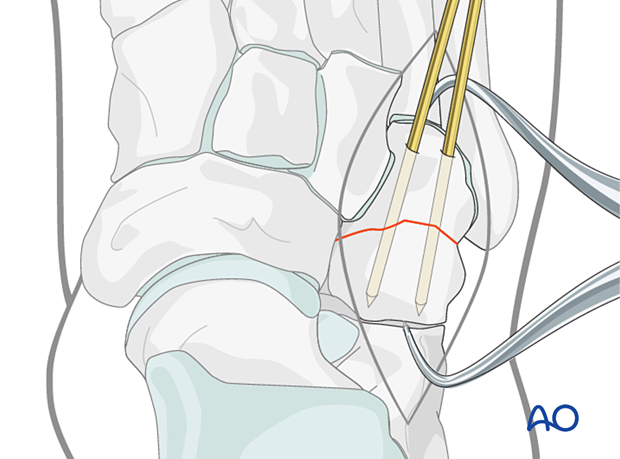
Fixation
Following the standard technique, insert two screws into the planned screw trajectory.
They may be non-cannulated, cannulated, or headless compression screws.
In contrast to lag screws inserted in the diaphysis, these lag screws will typically not penetrate the far cortex, as this would damage the opposite articular surface. Screw holes should be countersunk to prevent prominent hardware and interference with applying a neutralization plate.
Do not fully tighten the lag screws.
6. Aftercare
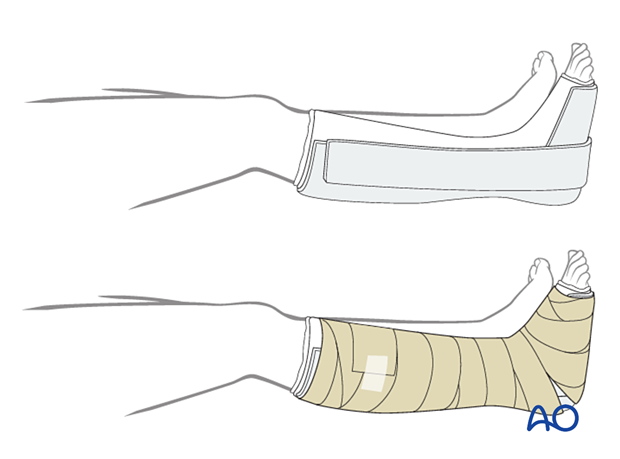
Dressing
The non-adherent antibacterial dressing is applied as a first layer. Sterile undercast padding is placed from toes to knee. Extra side and posterior cushion padding are added.
Immobilization
The foot should be immobilized for the first two weeks, which can be achieved using a three-sided plaster splint. The anterior area is left free of plaster to allow for swelling. Ensure that the splint’s medial and lateral vertical portions do not overlap anteriorly and that the splint does not compress the popliteal space or the calf.
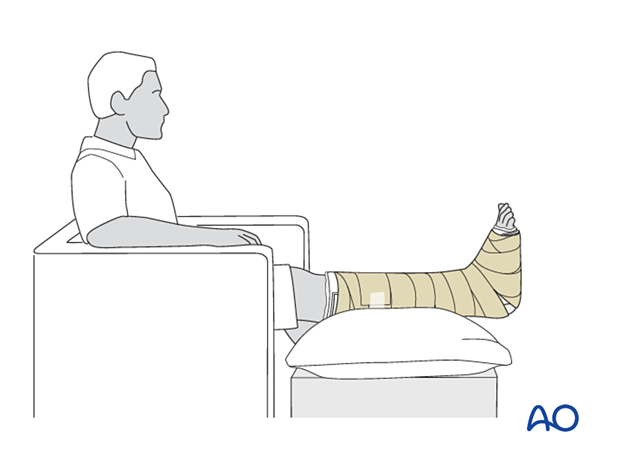
Follow-up
The patient should be counseled to keep the leg on a cushion and elevated. Remember not to elevate the leg too much as it may impede the inflow. The foot’s ideal position is halfway between the waist and the heart when the patient is sitting. While seated, the foot should be on a cushion and elevated, but if badly swollen, the patient must be supine since elevating the foot while seated decreases swelling less effectively.
Avoid direct pressure against the heel during recumbency to prevent decubiti.
The OR dressing is usually left in place and not changed until the first postoperative visit at two weeks when x-rays are obtained once the dressing is removed. If any complication is suspected (eg, infection or compartment syndrome), the dressing must be split and, if necessary, removed to allow full inspection.
The strict non-weight bearing should be maintained until there is evidence of healing and any transfixion K-wires (6–12 weeks) or bridging devices (min 12 weeks) are removed.
Daily toe movement is encouraged.
Formal physical therapy should not begin in the early postoperative period.
A gastrocnemius release may need to be performed in cases with postoperative gastrocnemius contracture. This occurs more typically in the mid and hind-foot.













