Compression plate fixation (straight plate)
1. General considerations
Compression plate principles
In some instances, intramedullary wire fixation is not preferred. Absolute stability is achieved using compression plate principles for simple transverse and selected wedge fractures.
Anatomical considerations
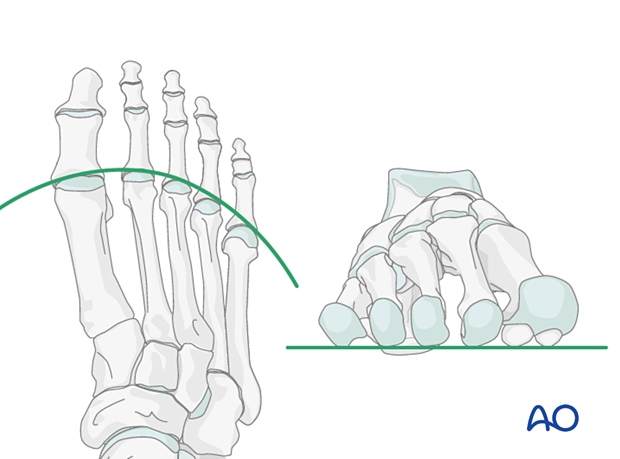
Proper alignment of the metatarsal heads is a critical goal in restoring the forefoot mechanics.
A normal curved “cascade” (Lelièvre’s parabola) appearance, which is symmetric with the other foot, is mandatory on the AP view. See illustration. This symmetry ensures that the normal length of the metatarsal is restored.
It is also critical to restore the metatarsals in their axial or horizontal plane so that all the metatarsal heads are on the same level in the axial view.
Any malalignment, particularly flexion, will recreate focally high pressure during the stance phase and toe-off, resulting in pain and subsequent callus formation.
The sesamoids, rather than the first metatarsal head, bear weight in the first row. Therefore, one must look at the sesamoid level in establishing the alignment in the axial or horizontal plane of the first metatarsal.
Timing of surgery
The timing of surgery is influenced by the soft tissue injury and the patient's physiologic status.

2. Patient preparation
This procedure is typically performed with the patient placed supine with the knee flexed at 90°.

3. Approaches
Fractures of the first metatarsal can be approached through a medial or a dorsal approach:
All other metatarsals are approached through the dorsal approach:
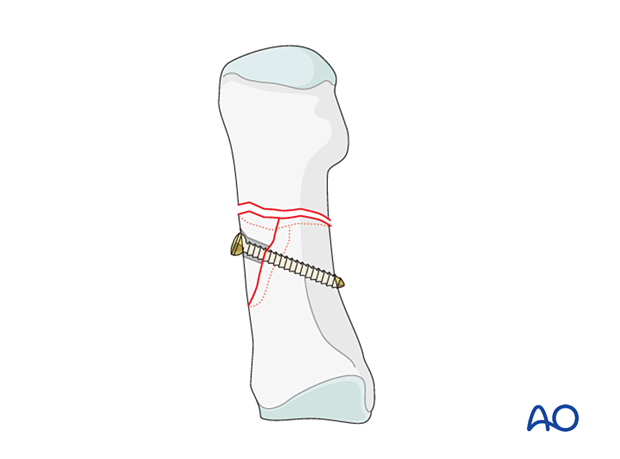
4. Reduction and fixation of the wedge fragment
Exposure of the fracture
Expose the fracture ends with minimal soft-tissue dissection off the bone.
Clean out the debris to allow reduction.
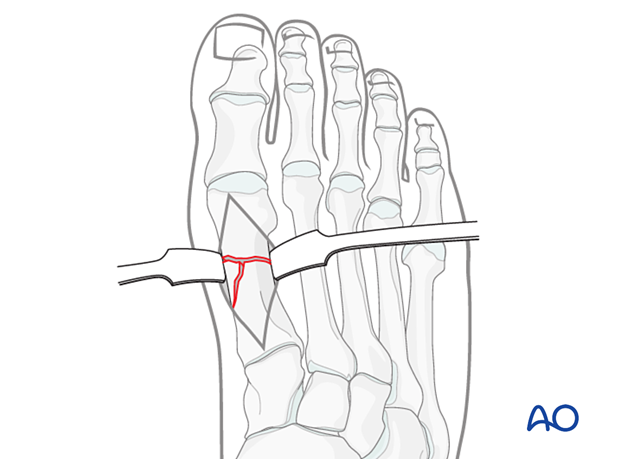
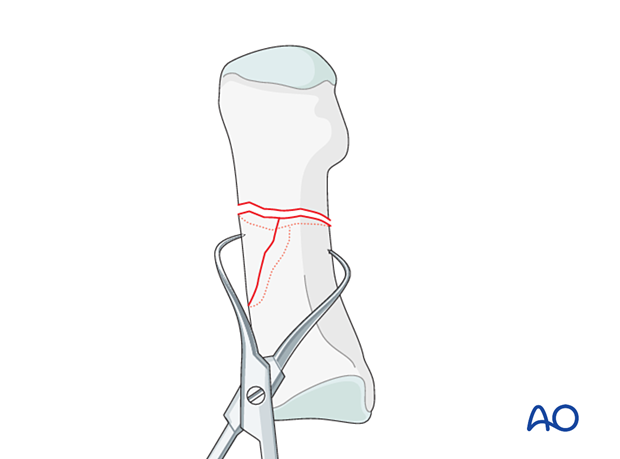
Reduction
Identify the end segment with the more oblique fracture and use pointed reduction forceps to reduce the wedge to that end segment.
Fixation
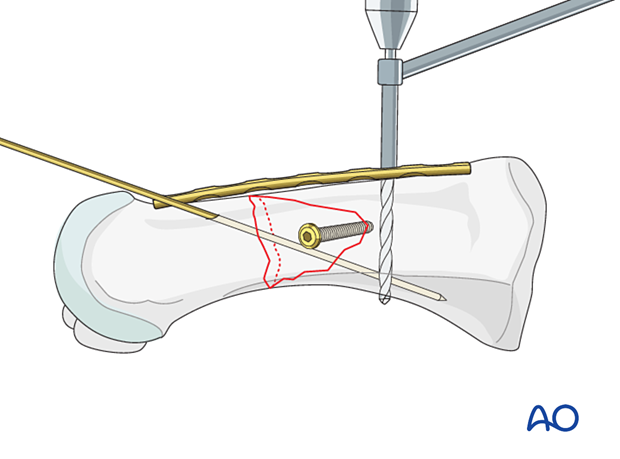
If possible, fix the wedge using a lag screw or, in the case of a small wedge, with a K-wire.
There is typically no room for more than one screw in a wedge fragment in the second to the fifth metatarsal.
The fracture is now simplified to an A-type pattern (simple fracture).
5. Reduction and fixation of the simple fracture
Two pointed reduction forceps can be used for direct reduction.
Alternatively, the plate can be used as a reduction tool instead of two forceps.
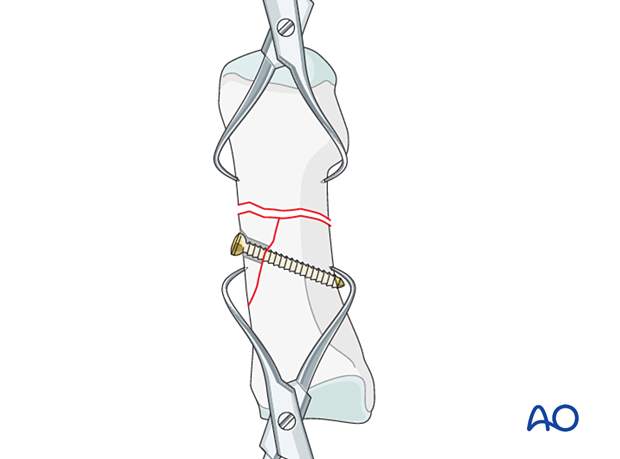
Temporary fixation
Insert a K-wire across the fracture plane for temporary stabilization.
Be aware that the cortical bone in the metatarsals is dense and thick, so the K-wire tip gets very hot. Irrigation during insertion of the K-wire is essential to avoid thermal necrosis of the bone and soft tissue around the wire track.
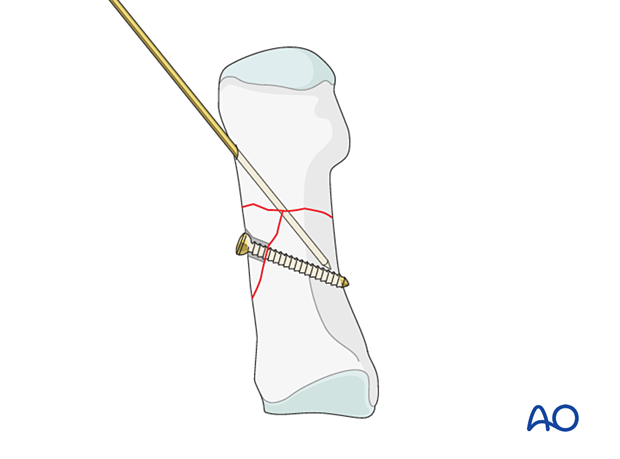
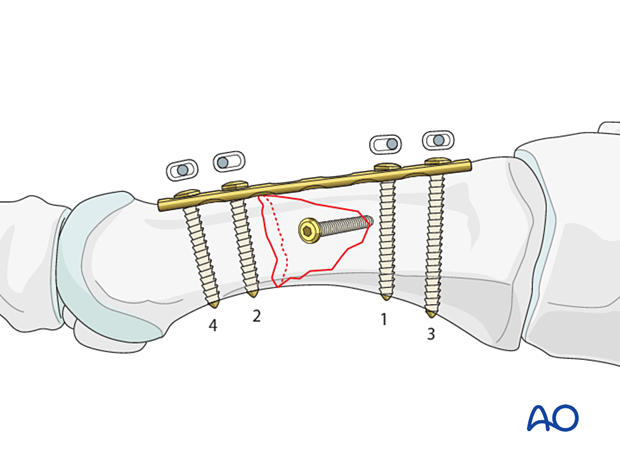
Plate preparation
Contour the plate to fit the dorsal bone surface.
For the first metatarsal, a 3.5 mm plate can be used, which allows for two to three screws in the distal and proximal segments.
For the second through fourth metatarsals, a 2.7 mm plate can be used, allowing two to three screws in each segment.
For very proximal fractures, T-plates may be used.
The plate has to be slightly over contoured to compress the far cortex when axial compression is produced by tightening the screws.
If the plate is not overbent, tightening the screws will result in a gap in the opposite cortex.
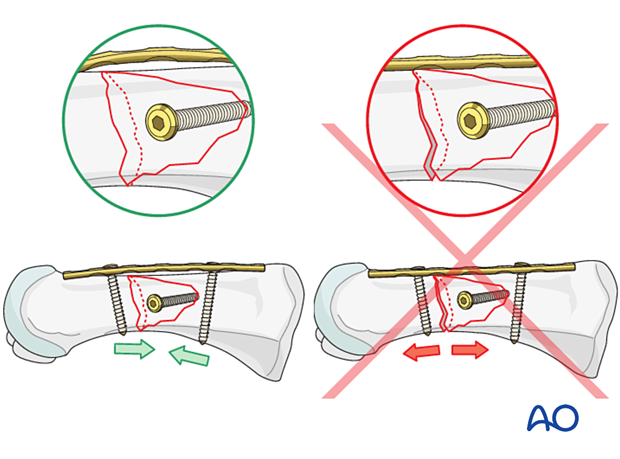
Plate application
The compression plate is applied according to standard techniques.
6. Aftercare
An appropriate well-padded dressing should be applied to protect the surgical incision. Compression will help control swelling.
If present, the skin-pin interface should be similarly well-padded but with dressings that can be readily removed to inspect for pin site infection.
Immediate postoperative treatment is rest, ice, and elevation.
The patient should restrict weight-bearing for six weeks until signs of radiographic healing are present. After this, patients can be weight-bearing as tolerated.
Patients must exercise their ankle and subtalar joints out of the orthosis to prevent stiffness (eg, by stretching their Achilles).
X-ray the metatarsals at six weeks to confirm satisfactory union and remove K-wires if present. Once the fracture is united, the orthosis may be gradually discontinued.
A gastrocnemius release may need to be performed in cases with postoperative gastrocnemius contracture. This occurs more typically in the mid- and hindfoot.
If the gastrocnemius muscle has been released, a splint or cam walker can be used to protect the surgical site.













