Screw fixation
1. Introduction
Screw fixation
These fractures can usually be treated with retrograde screw fixation.
In severely impacted fractures, bone graft harvested from the distal radius may be necessary.
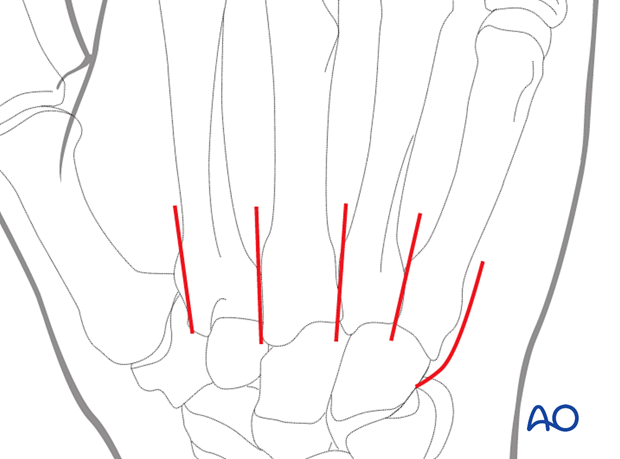
Fracture configuration
The degree of displacement and the number of fragments may be difficult to judge on standard x-rays. CT scans can be helpful in these situations.
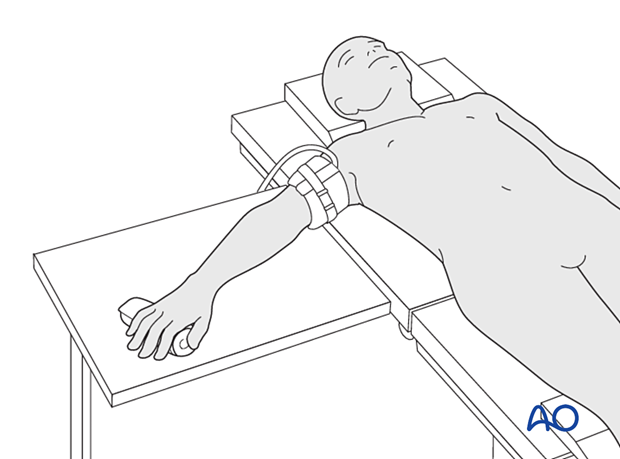
2. Patient preparation
Place the patient supine with the arm on a radiolucent hand table.
3. Approaches
For this procedure, a dorsal approach to the CMC joint can be used.
Alternatively, the proximal end of the following approaches can be used:
4. Reduction
Reduction tools
Manipulate the articular fragments with a dental pick, small K-wires, or a small periosteal elevator.
Small K-wires can also be used for preliminary fixation. Depending on fracture configuration, pointed forceps may be useful for reduction.
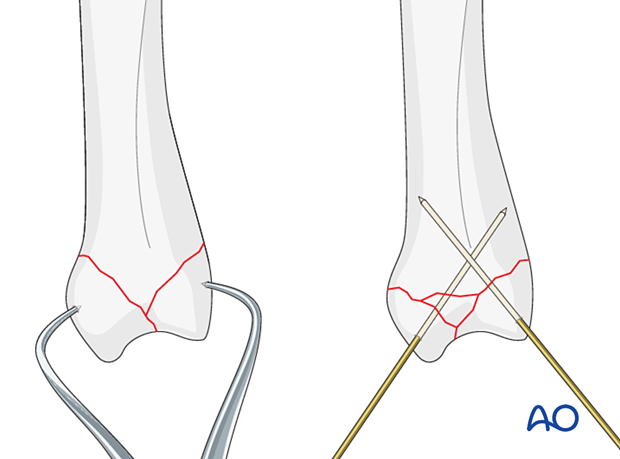
Confirming anatomical reduction
Check anatomical reduction of the joint surface under direct view.
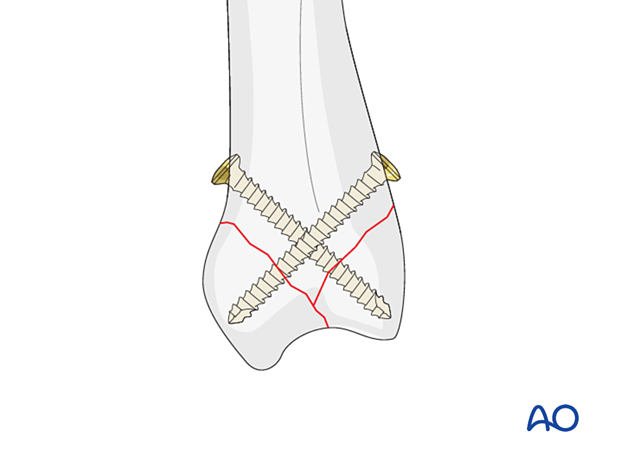
5. Screw fixation
Screw size selection
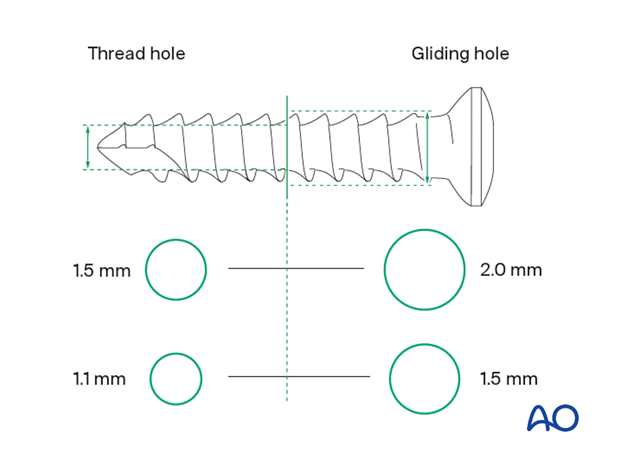
The exact size of the diameter of the screws used will be determined by the fragment size and the fracture configuration.
The various gliding and thread hole drill sizes for different screws are illustrated here.
Screw insertion
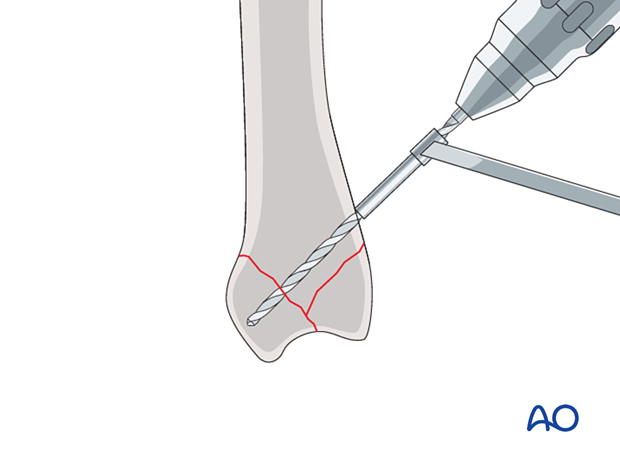
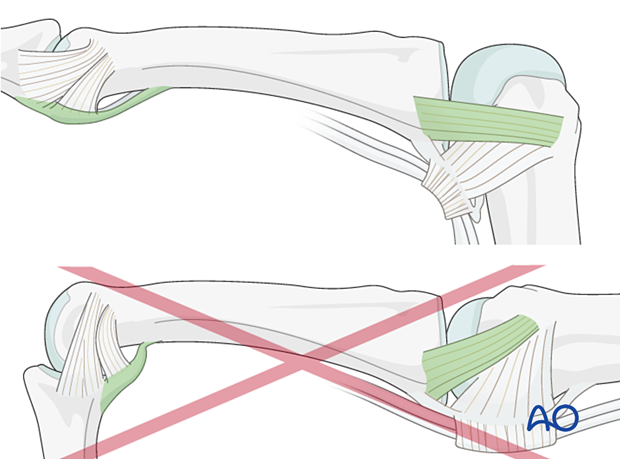
Insert lag screws in a retrograde manner, avoiding compromise of the joint.
Drill very carefully not to perforate the articular cartilage. If necessary, drilling is performed under image intensification. Drill at low speed and without exerting pressure.
As the screws do not engage the opposite cortex, they are inserted as position screws, ie, they are threaded in both fragments.
If the fragments extend to the metaphyseal region, bicortical lag screws can be used.
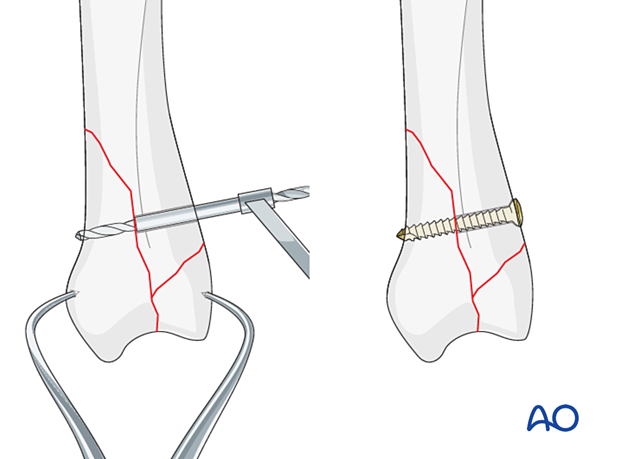
Carefully insert the screw without displacing the reduced fragments. Confirm correct screw insertion with an image intensifier.
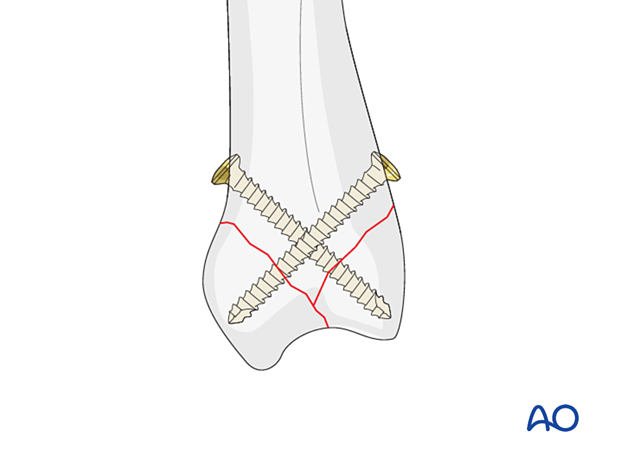
Insert additional screws in a similar manner.
6. Final assessment
Confirm correct rotational alignment by clinical examination.
Image intensification may be used to confirm anatomical reduction and correct placement of implants in two views.
7. Aftercare
Postoperative phases
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.
Postoperative treatment
If there is swelling, the hand is supported with a dorsal splint for a week. This would allow for finger movement and help with pain and edema control. The arm should be actively elevated to help reduce the swelling.
The hand should be splinted in an intrinsic plus (Edinburgh) position:
- Neutral wrist position or up to 15° extension
- Metacarpophalangeal (MCP) joint in 90° flexion
- Proximal interphalangeal (PIP) joint in extension
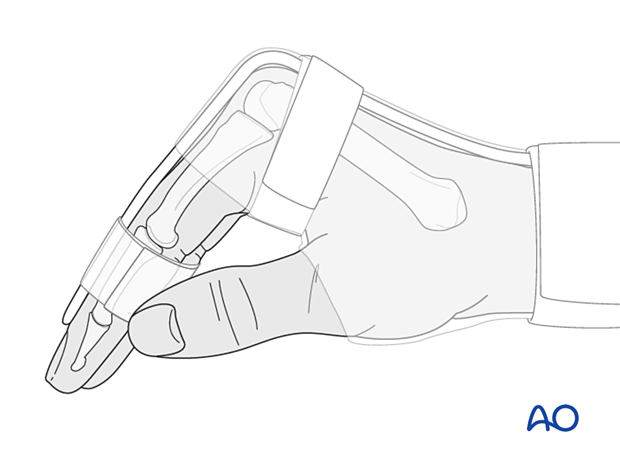
The reason for splinting the MCP joint in flexion is to maintain its collateral ligament at maximal length, avoiding scar contraction.
PIP joint extension in this position also maintains the length of the volar plate.
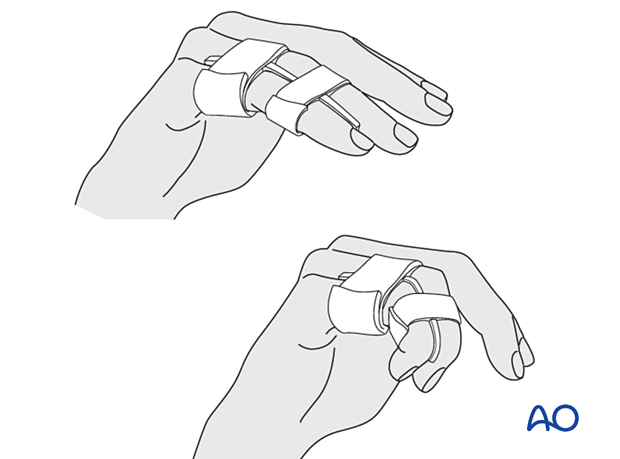
After subsided swelling, protect the digit with buddy strapping to a neighboring finger to neutralize lateral forces on the finger.
Functional exercises
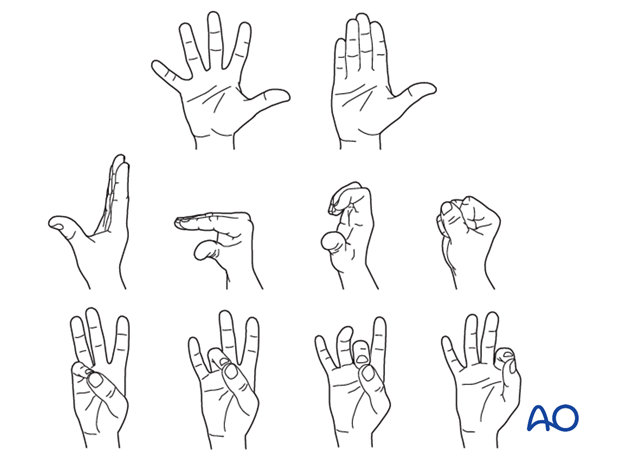
To prevent joint stiffness, the patient should be instructed to begin active motion (flexion and extension) immediately after surgery.
Follow-up
See the patient after 5 and 10 days of surgery.
Implant removal
The implants may need to be removed in cases of soft-tissue irritation.
In case of joint stiffness or tendon adhesion restricting finger movement, arthrolysis or tenolysis may become necessary. In these circumstances, the implants can be removed at the same time.













