Joint reconstruction of central impaction fracture
1. Principles
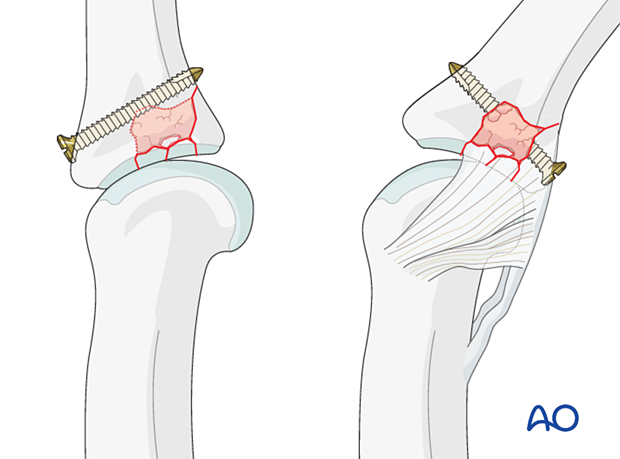
Central impaction fractures need reduction of subchondral fragments. Bone graft and a subchondral screw should be added to support the articular surface.
The palmar avulsion fragment can be stabilized with a position screw if large enough.
Another option is the addition of an antiglide or buttress plate on the volar surface.
The recovery process after such injuries is slow. Advise the patient to expect 6–8 months for full recovery.
2. Patient preparation
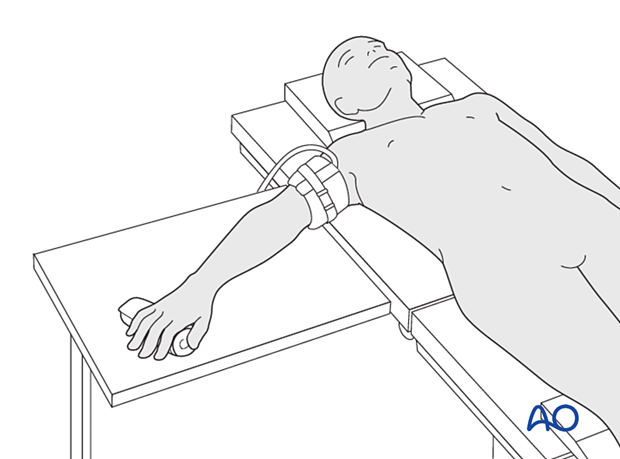
Place the patient supine with the arm on a radiolucent hand table.
3. Approach
For this procedure, a palmar approach to the PIP joint is normally used.
4. Reduction of dislocation
Closed reduction
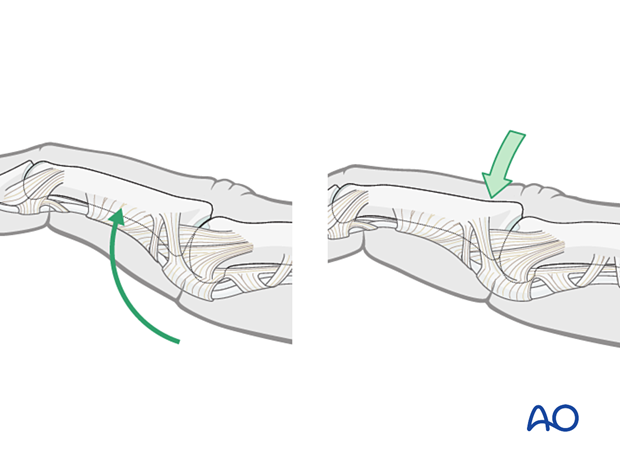
Dislocation usually presents as an extension displacement with dorsal deformity.
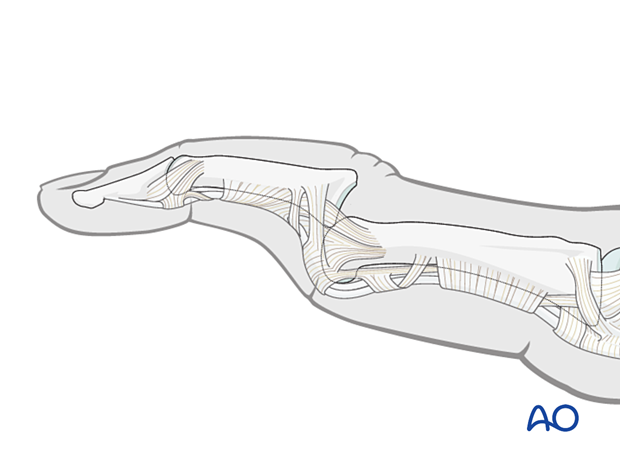
This can be reduced by increasing the deformity with gentle dorsally applied pressure on the middle phalanx to reduce the joint. This keeps the palmar structures in tension and reduced the risk of soft-tissue interposition.
5. Fracture reduction
The reduction of the articular fragments can be achieved in different ways depending on the fracture pattern:
- Closed by distraction
- Directly through the fracture
- Directly through a remote entry window
Reduction of the depressed articular fragments
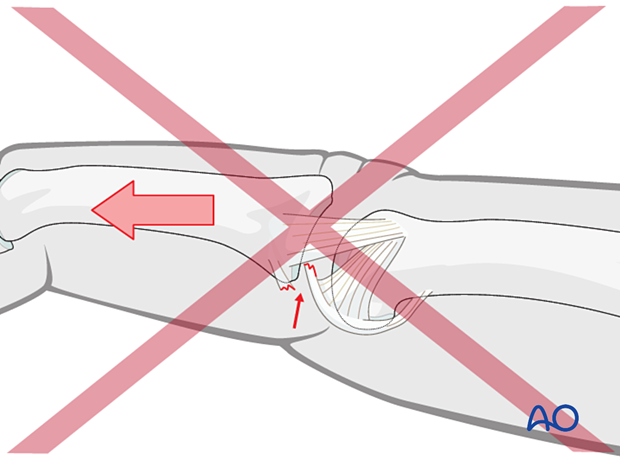
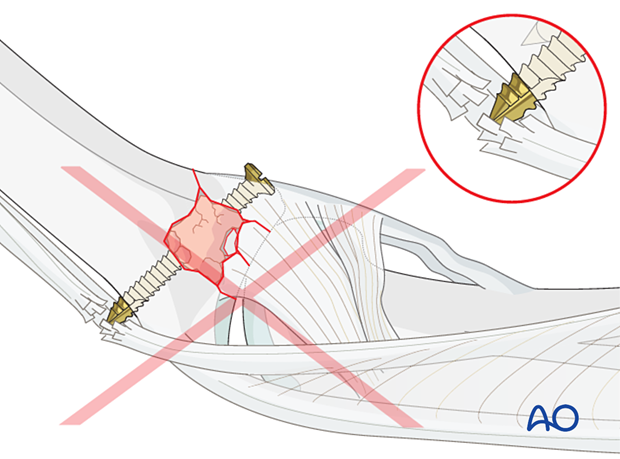
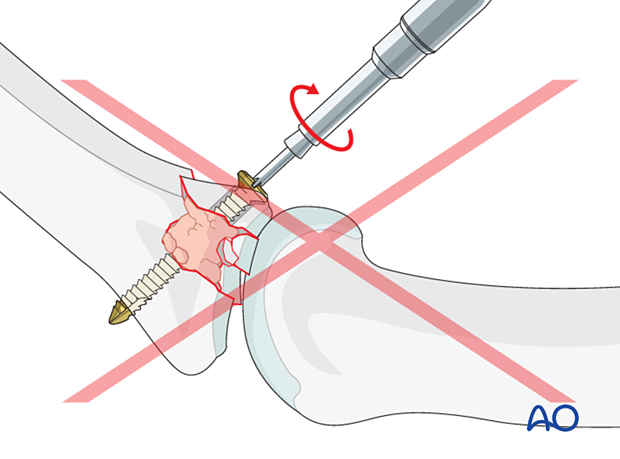
Compression fractures are not reducible by ligamentotaxis, as the centrally impacted fragments are devoid of soft-tissue attachments.
Direct reduction is thus necessary.
The key to fixing compression fractures is restoring the joint surface to as close to normal as possible (anatomically) and supporting the reduction with bone graft if needed.
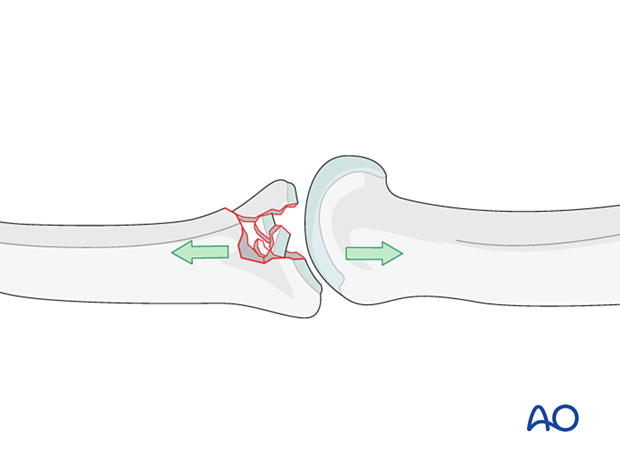
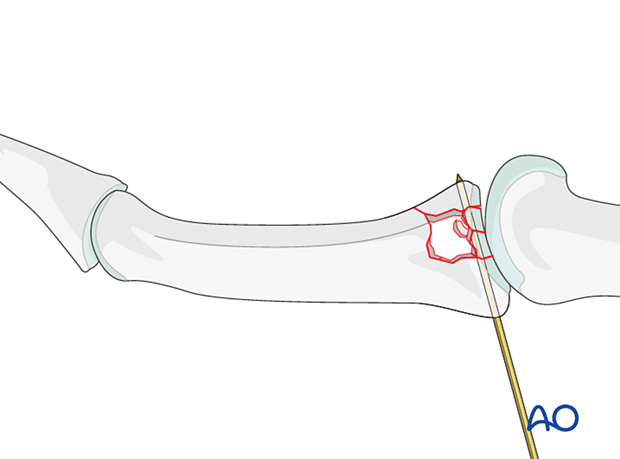
Use a K-wire, a dental pick, or a small curette to push the depressed fragments towards the head of the proximal phalanx, which should be used as a template to restore congruity of the articular surface of the middle phalanx to reduce the risk of later degenerative joint disease.
If a cartilage step-off remains, degenerative joint disease is likely to follow.
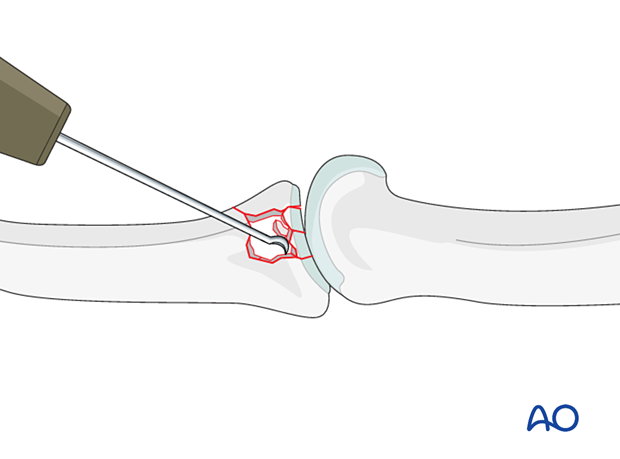
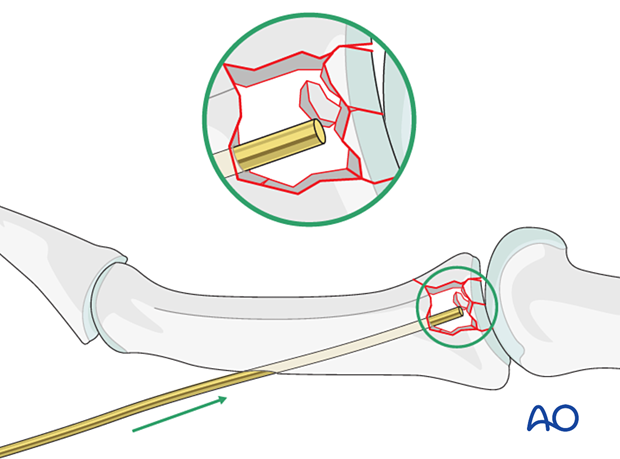
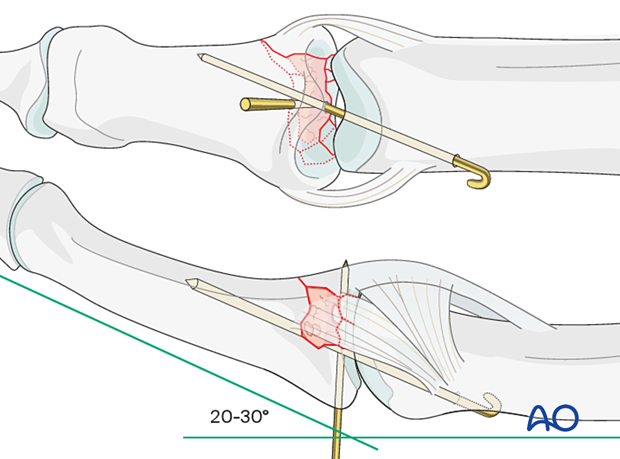
Optionally, for reduction, a K-wire may be inserted through the shaft and the medullary canal up to the subchondral region.
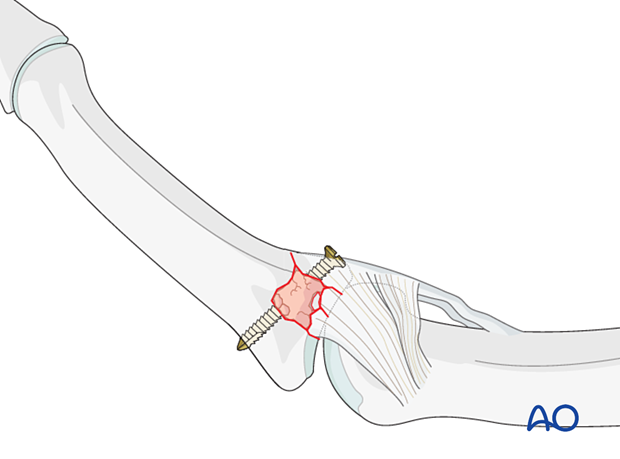
Stabilization of articular fragments
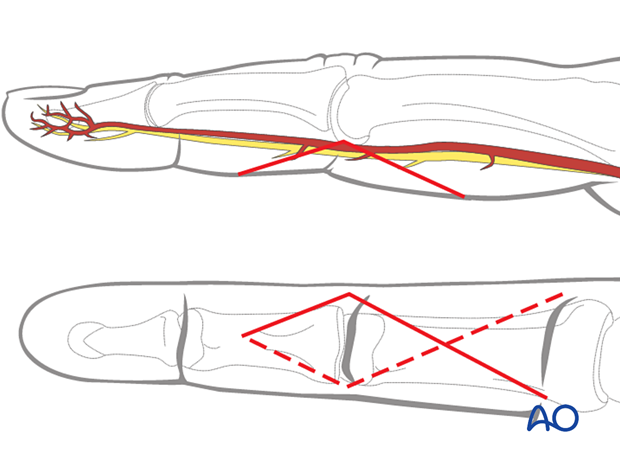
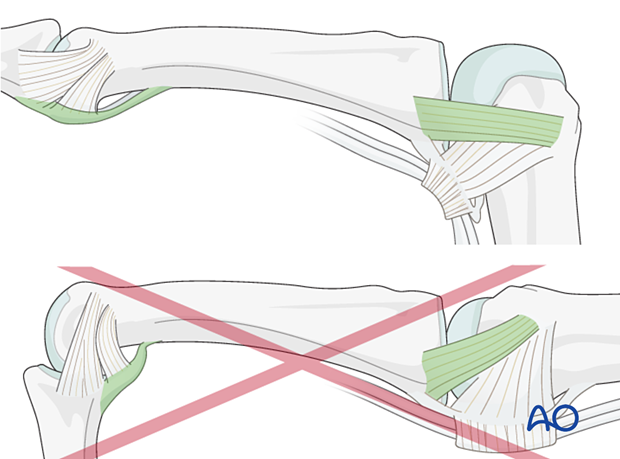
Insert one or more K-wires preferably from dorsal to palmar to stabilize the reduction of the articular fragments. This can be left until fracture consolidation.
Insertion from palmar to dorsal may damage neurovascular bundle and flexor tendons.
6. Adding bone graft
Since the subchondral cancellous bone is impacted, a void may remain following reduction of the articular fragments.
This jeopardizes fracture healing:
- Very unstable situation in which the fragments may easily redisplace (collapse)
- Delayed healing process
Therefore, bone grafting is recommended to provide support to the subchondral bone and increase the potential for bone regeneration and healing.
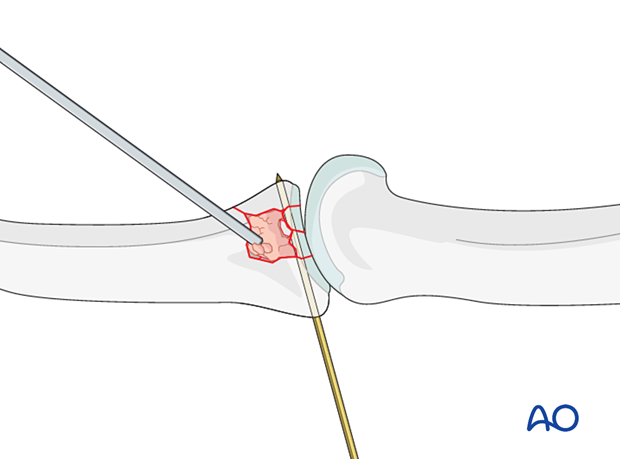
Use a pusher instrument to fill the whole fracture cavity and impact the bone graft.
Confirm reduction with an image intensifier.
7. Fixation
Position screw fixation
If a large palmar fragment is present, maintain its reduction using a position screw (a bicortical cortex screw without lag compression). If the fragment is not large enough, a K-wire may be used, preferably from dorsal to avoid injury to the volar plate.
Maintaining the reduction with slight pressure from a drill guide, drill a threaded hole using the corresponding drill.
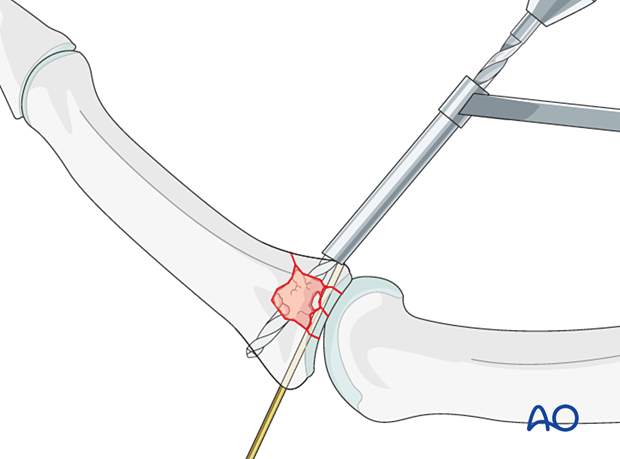
Insert the screw and carefully tighten it just enough to hold the reduction. The screw should just penetrate the opposite cortex.
Check joint congruity using image intensification. Reduction must be anatomical.
8. Protection of articular reconstruction
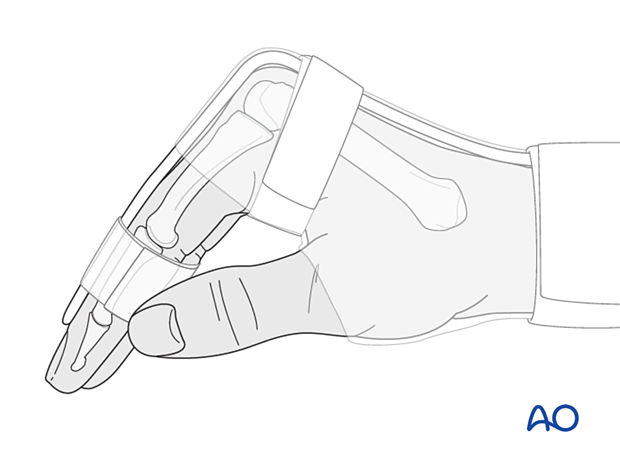
Dynamic external fixator
A dynamic external fixator may be added for 4 weeks to keep the PIP joint to length and to allow for early mobilization.

Joint transfixation with K-wire
Following articular reconstruction, if joint instability persists, the PIP joint may be transfixed with a K-wire obliquely, with the joint in 20°–30° of flexion to protect the ligament reattachment. This has a high risk of joint stiffness.
Leave the end of the K-wire outside of the skin for later removal.
The K-wire can be removed after 3–4 weeks.
9. Final assessment
Check joint congruity using image intensification or x-ray. Reduction must be anatomical.
10. Aftercare
Postoperative phases
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.
Postoperatively
If the joint reconstruction has been supported with a dynamic external fixator, additional splinting is not necessary. Early controlled joint mobilization is encouraged.
If joint transfixation has been applied, the hand is immobilized with a dorsal splint for 3–4 weeks. This should permit movement of the unaffected fingers. The arm should be actively elevated to help reduce the swelling.
The hand should be immobilized in an intrinsic plus (Edinburgh) position:
- Neutral wrist position or up to 15° extension
- MCP joint in 90° flexion
- PIP joint in extension
The MCP joint is splinted in flexion to maintain its collateral ligaments at maximal length to avoid contractures.
The PIP joint is splinted in extension to maintain the length of the volar plate.
Follow-up
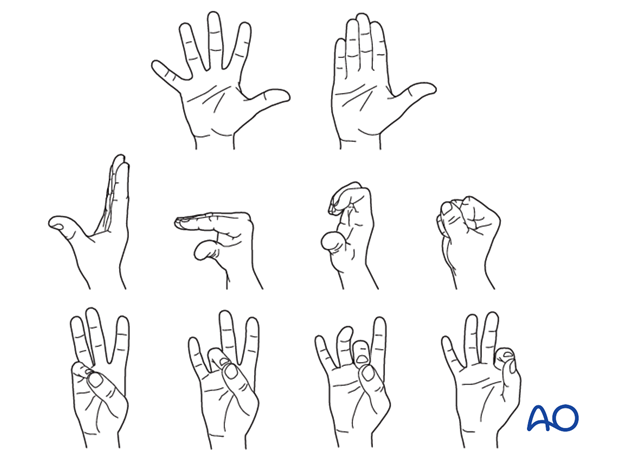
The patient is reviewed frequently to ensure progression of hand mobilization.
In the middle phalanx, the fracture line can be visible in the x-ray for up to 6 months. Clinical evaluation (level of pain) is the most important indicator of fracture healing and consolidation.
Remove the splint and K-wire after 3–4 weeks and protect the finger with buddy strapping to a neighboring finger to neutralize lateral forces on the finger.
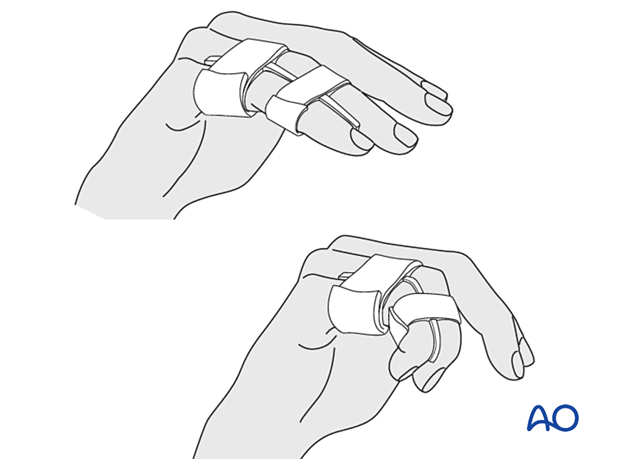
Mobilization
If the fixation is stable enough, the patient is encouraged to take off the splint 2–3 times daily, and to commence with gentle active exercises, provided no transarticular K-wire has been used or has already been removed.
After 4 weeks, the splint (and any K-wire or dynamic external fixator) is removed, and unrestricted active flexion and extension are permitted.
Implant removal
The implants may need to be removed in cases of soft-tissue irritation.
In case of joint stiffness or tendon adhesion restricting finger movement, arthrolysis or tenolysis may become necessary. In these circumstances, the implants can be removed at the same time.
11. Case
AP and oblique x-ray showing central/palmar impaction fractures of the middle phalangeal base of the 3rd and 4th finger

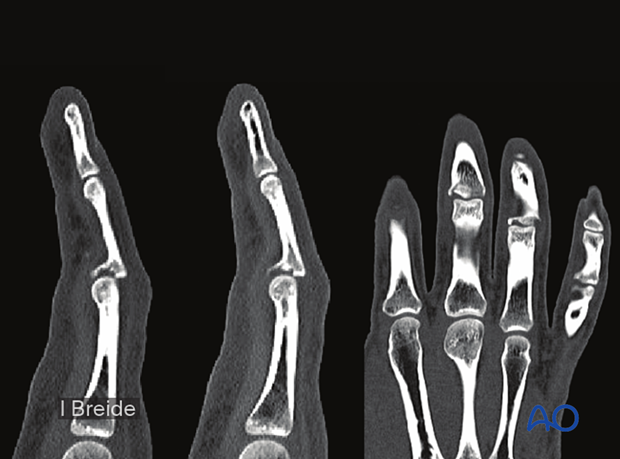
CT of the same case
Postoperative lateral and AP x-ray after screw stabilization in the 3rd middle phalanx and buttress plating in the 4th middle phalanx.














