Lag-screw and plate fixation
1. General considerations
Introduction
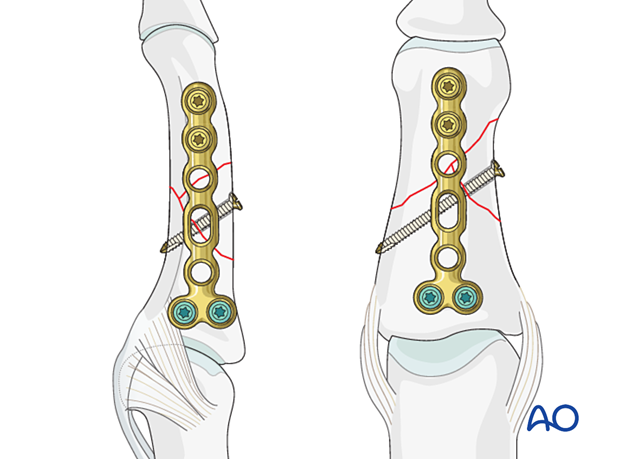
A wedge fragment may be fixed to both end segments with lag screws if the fractures are sufficiently oblique and the wedge fragment large enough. The plate may be applied laterally or dorsally. The lateral application is preferred as it avoids disturbance of the extensor mechanism insertion.
This technique is useful to gain more stability if only nonlocking plates are available.
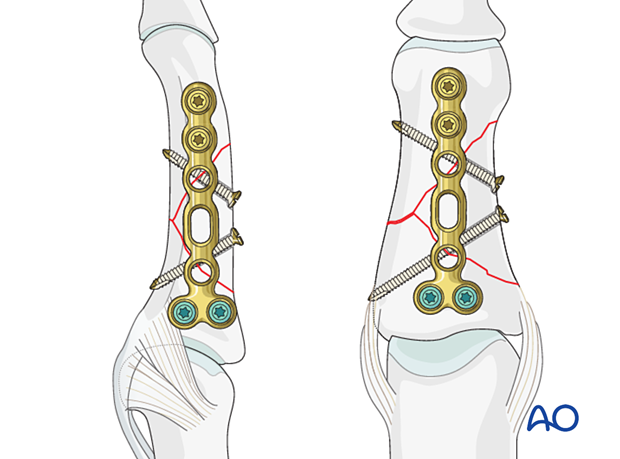
If the fracture morphology allows only one lag screw, fracture stabilization is completed with a lateral or dorsal bridge plate.
Smaller lag screws (1.0 or 1.3 cortical) should be used to avoid vascular compromise and further fragmentation. In doubt, bridge plating should be considered.
Lag-screw planning
Obliquity of the wedge fracture is possible either in the plane visible in the AP view or the lateral view. Always confirm the fracture configuration with views in both planes.
In this procedure, an oblique wedge fracture visible in the lateral view is shown with lag screw fixation protected with a lateral plate.
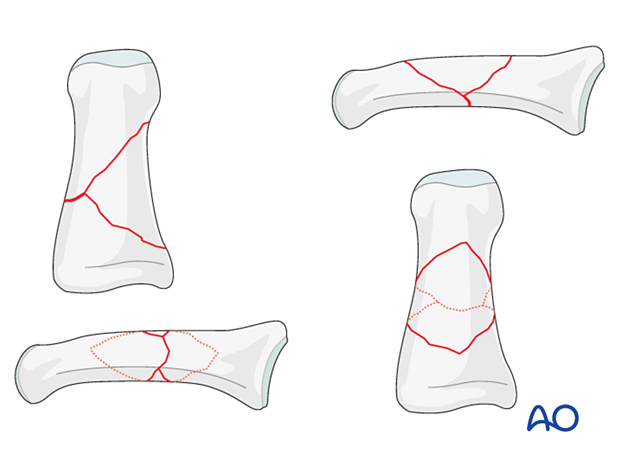
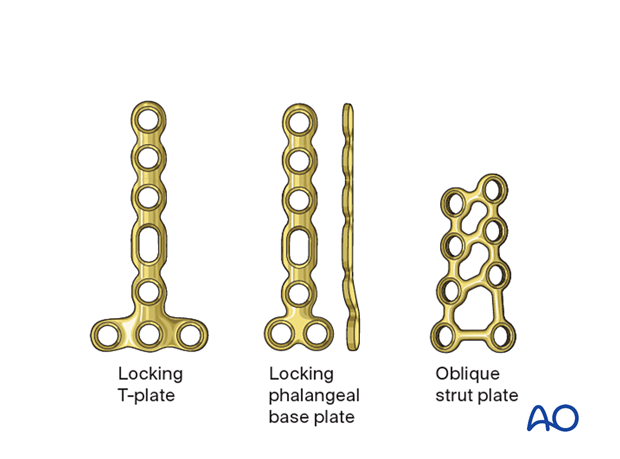
Plate selection
Several plate types (low profile) may be used:
- T-plate; dorsal
- Strut plate; dorsal
- Phalangeal base plate; lateral
The selection of the plate depends on the fracture pattern and should allow for at least two screws in the proximal and distal main fragment.
In this procedure, plate fixation with a lateral phalangeal base plate is shown.
If an anatomical plate is not available, a conventional minicondylar plate may be used.
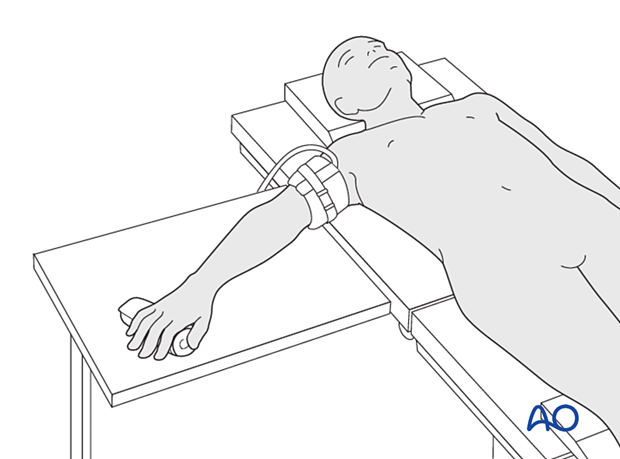
2. Patient preparation
Place the patient supine with the arm on a radiolucent hand table.
3. Approaches
For this procedure the following approaches may be used:
4. Reduction
Gaining length
Length can be gained by traction applied either manually or with pointed reduction forceps.
Confirm length and rotation clinically and with an image intensifier.
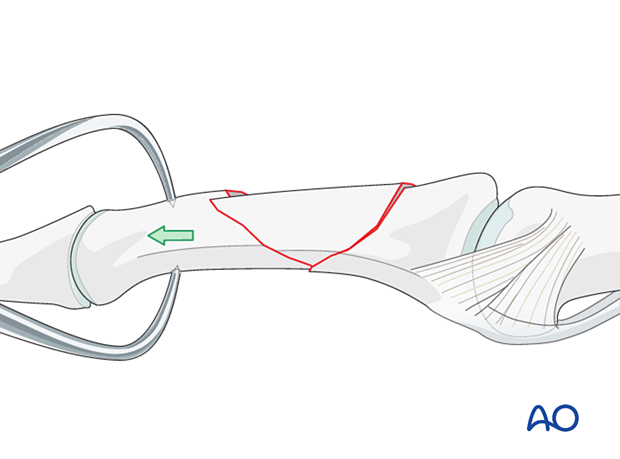
Reducing rotation and angulation
Manipulate the fragments with pointed reduction forceps to reduce rotation and restore correct angulation.
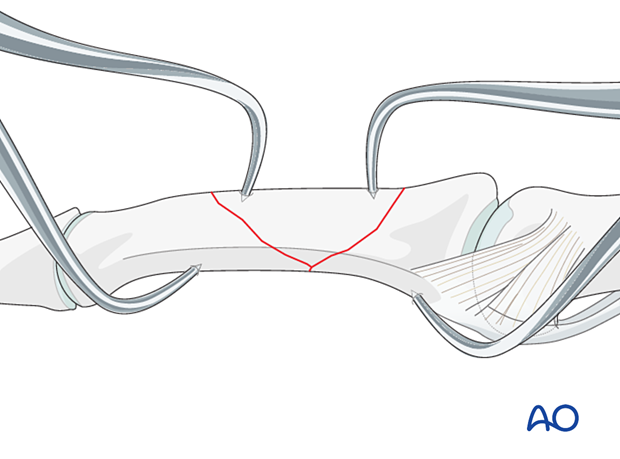
Preliminary fixation
Preliminarily secure the reduction with K-wires or reduction forceps.
Alternatively, hold the reduction with reduction forceps designed for percutaneous technique. Impingement of soft tissues should be avoided.
5. Checking alignment
Identifying malrotation
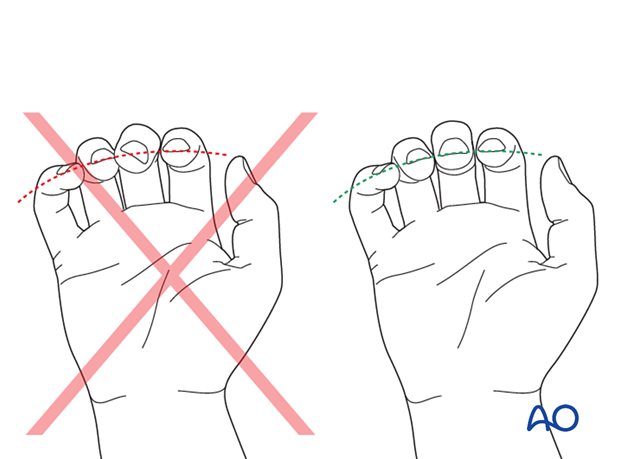
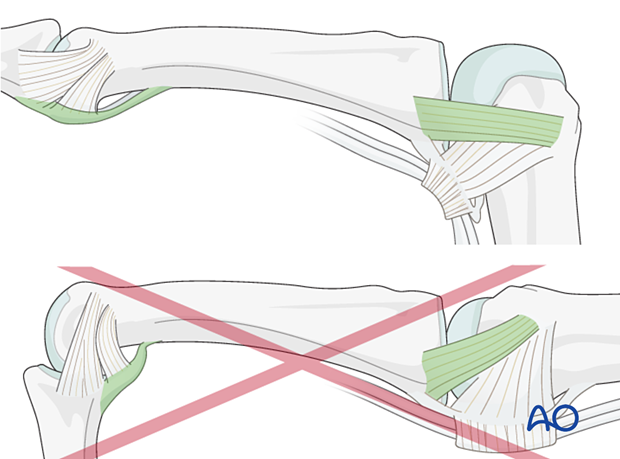
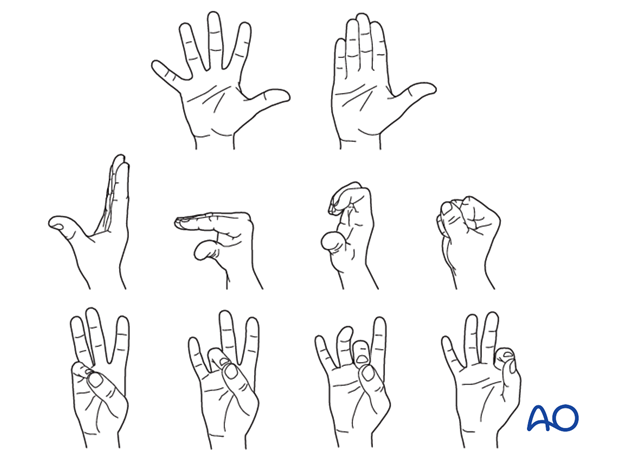
At this stage, it is advisable to check the alignment and rotational correction by moving the finger through a range of motion.
Rotational alignment can only be judged with the fingers in a degree of flexion, and never in full extension. Malrotation may manifest itself by overlap of the flexed finger over its neighbor. Subtle rotational malalignments can often be judged by tilting of the leading edge of the fingernail when the fingers are viewed end-on.
If the patient is conscious and the regional anesthesia still allows active movement, the patient can be asked to extend and flex the finger.
Any malrotation is corrected by direct manipulation and later fixed.
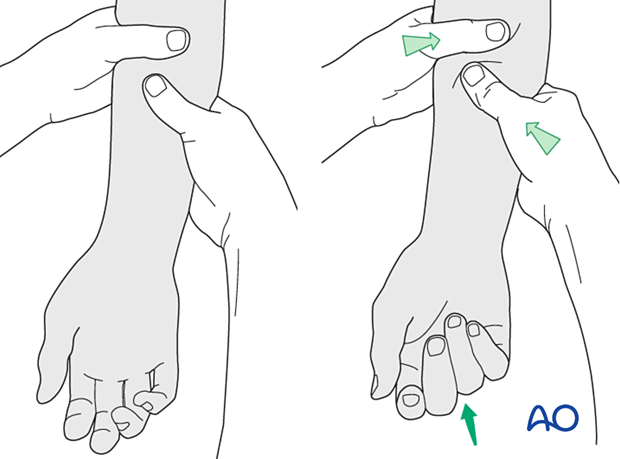
Using the tenodesis effect when under anesthesia
Under general anesthesia, the tenodesis effect is used, with the surgeon fully flexing the wrist to produce extension of the fingers and fully extending the wrist to cause flexion of the fingers.
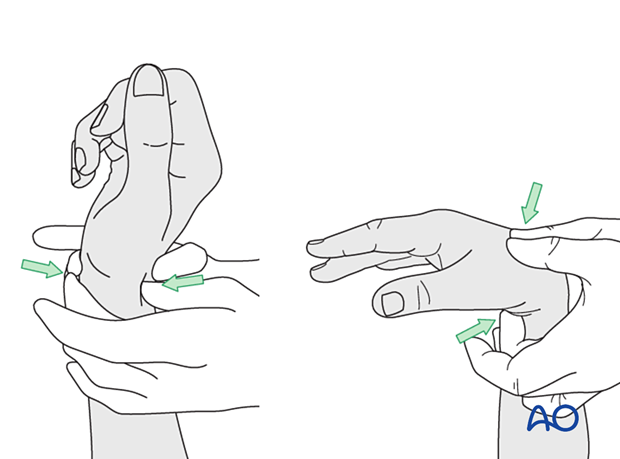
Alternatively, the surgeon can exert pressure against the muscle bellies of the proximal forearm to cause passive flexion of the fingers.
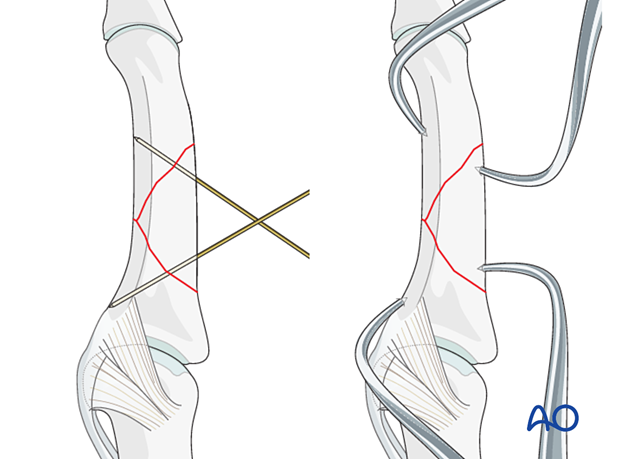
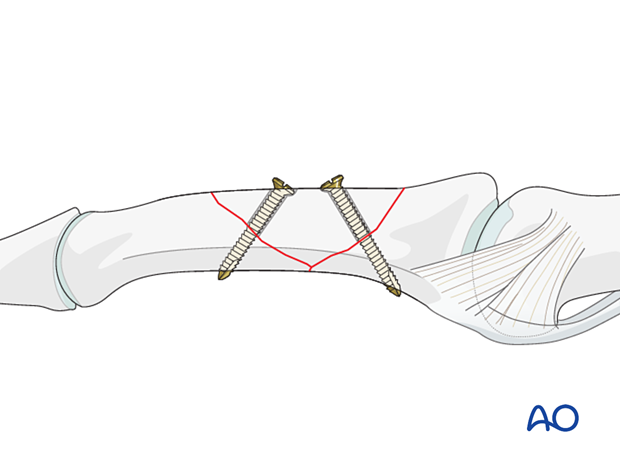
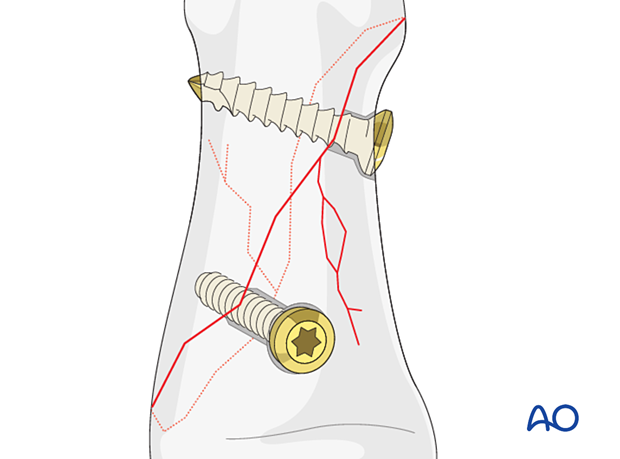
6. Lag-screw fixation
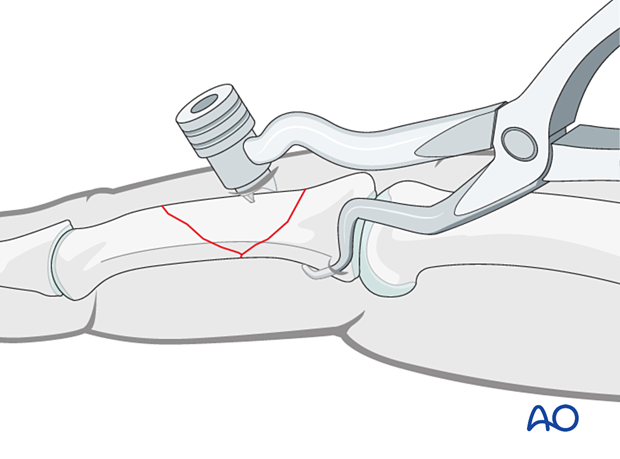
The lag screw should be inserted centered on and as perpendicularly to the fracture plane as possible and from the dorsal surface. The obliquity of the fracture plane dictates the exact position and direction of the lag screw.
Countersinking is not necessary and risks iatrogenic fractures.
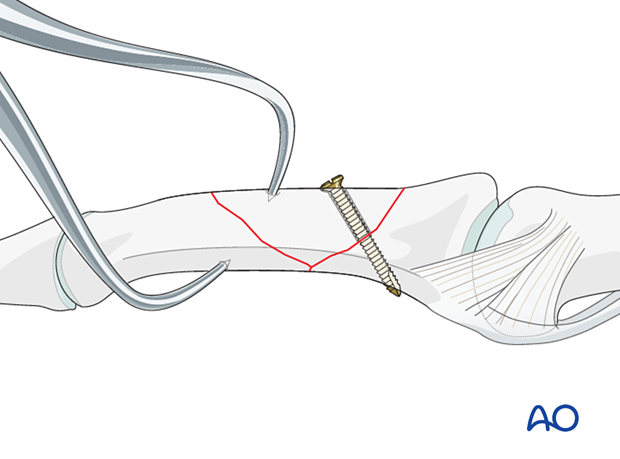
Fix the wedge fragment to the other end segment with another lag screw if the size of the wedge fragment and the fracture plane allow it.
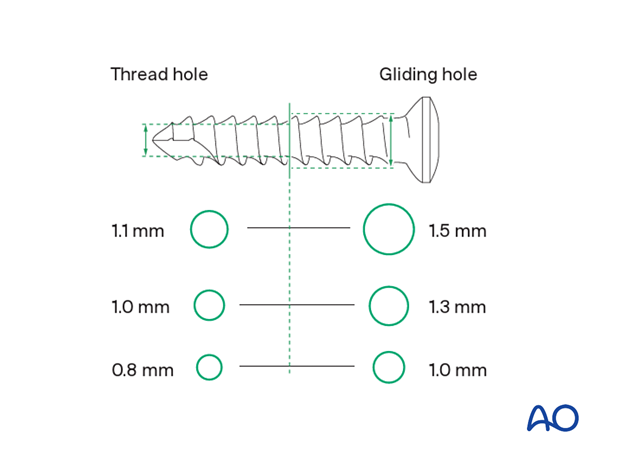
Screw size
The exact size of the diameter of the screws used will be determined by the fragment size and the fracture configuration.
The various gliding and thread hole drill sizes for different screws are illustrated here.
Screw length pitfalls
- Too short screws do not have enough threads to engage the cortex properly. This problem increases when self-tapping screws are used due to the geometry of their tip.
- Too long screws endanger the soft tissues, especially tendons and neurovascular structures. With self-tapping screws, the cutting flutes are especially dangerous, and great care has to be taken that the flutes do not protrude beyond the cortical surface.
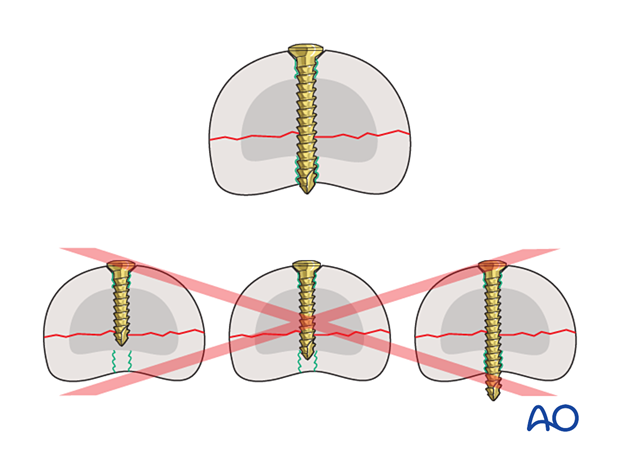
Pitfall: screw too close to the fracture
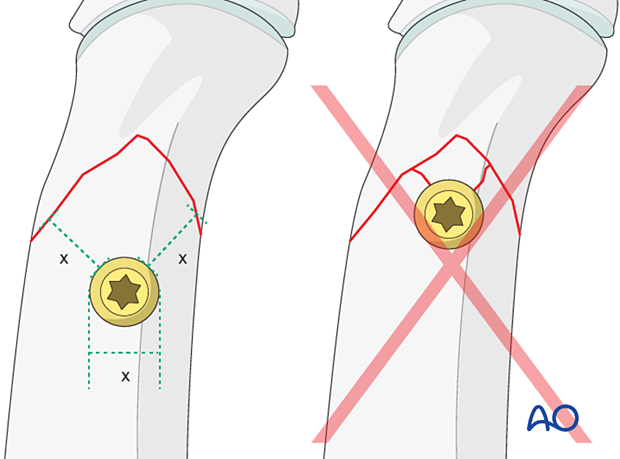
Pitfall: beware of fissure lines
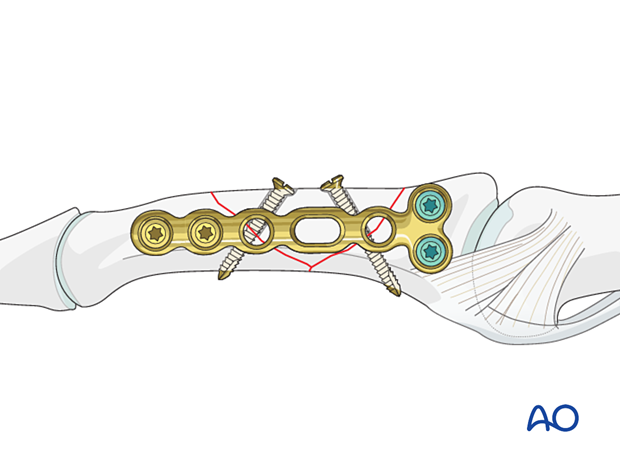
7. Plate application
Apply a neutralization plate depending on the fracture plane and the lag screw positions, either dorsally or laterally.
Insert at least two screws proximally and distally to the fracture in neutral mode.
Plate trimming
Adapt the plate length to fit the length of the middle phalanx. Avoid sharp edges, which may be injurious to the tendons. At least two screws need to be inserted on either side of the fracture zone.
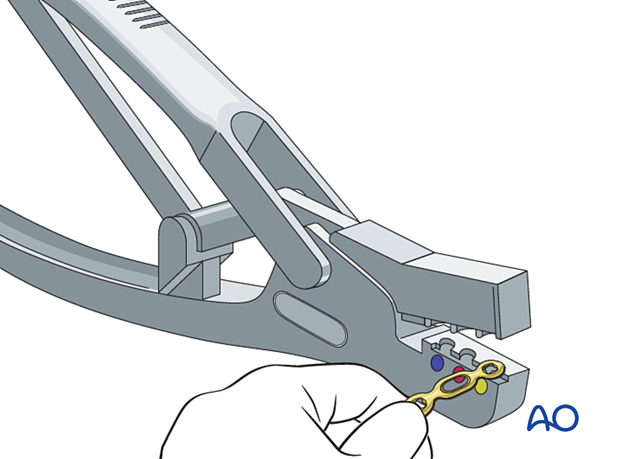
Plate positioning
Place the plate slightly dorsal to the midaxial line of the bone, allowing at least two screws in both main fragments.
Make sure the plate is perfectly aligned with the long axis of the proximal phalanx in the lateral view.
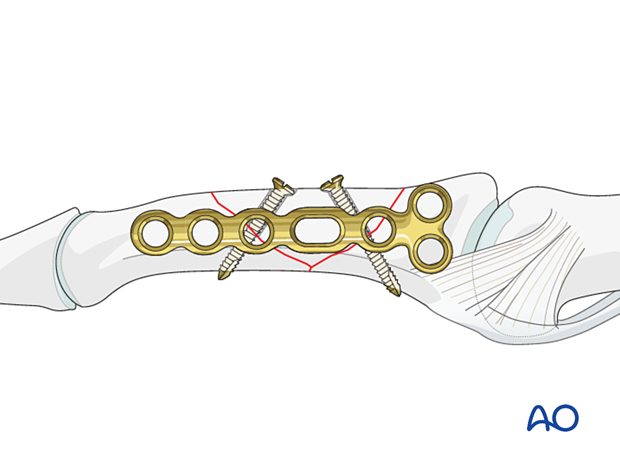
Insertion of screws
Insert locking-head screws in the base and cortical screws in the distal end of the plate.
Take care not to violate the joint surface.
Confirm reduction and implant position with an image intensifier.
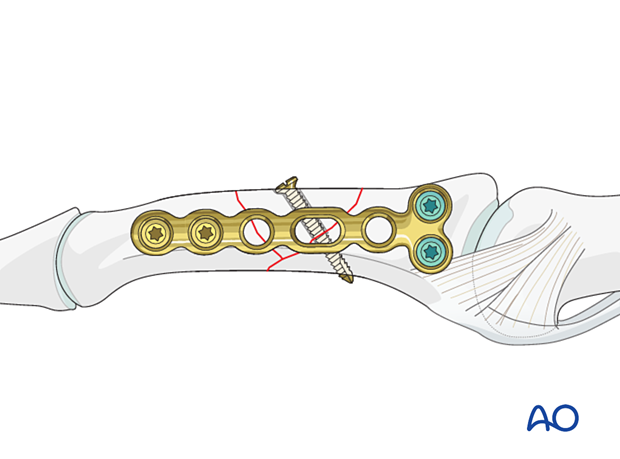
Bridge plate
If the wedge fragment can only be fixed to one end segment, apply the plate in bridging mode. Compression may be applied with caution and if the fracture configuration and stability allows.
Cover the plate with periosteum to avoid adhesion between the tendon and the implant leading to limited finger movement.
8. Final assessment
Confirm fracture reduction and stability and implant position with an image intensifier.
9. Aftercare
Postoperative phases
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.
Postoperative treatment
If there is swelling, the hand is supported with a dorsal splint for a week. This should allow for movement of the unaffected fingers and help with pain and edema control. The arm should be actively elevated to help reduce the swelling.
The hand should be immobilized in an intrinsic plus (Edinburgh) position:
- Neutral wrist position or up to 15° extension
- MCP joint in 90° flexion
- PIP joint in extension
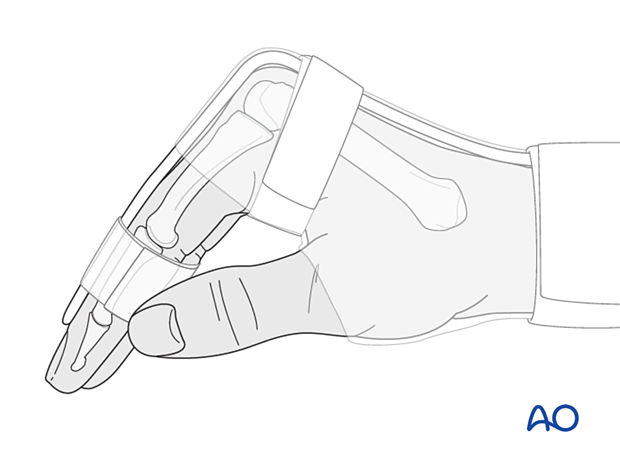
The MCP joint is splinted in flexion to maintain its collateral ligaments at maximal length to avoid contractures.
The PIP joint is splinted in extension to maintain the length of the volar plate.
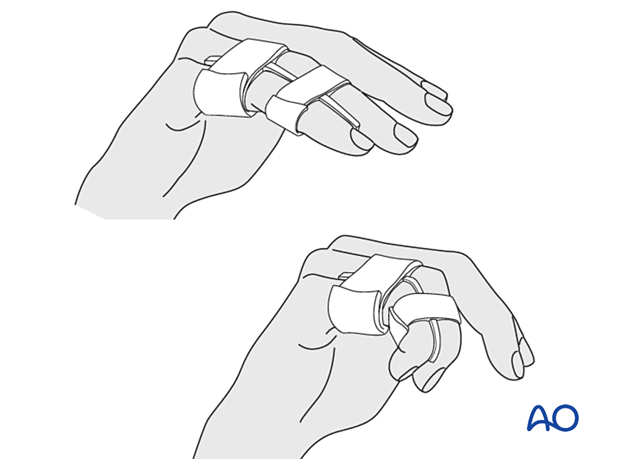
After swelling has subsided, the finger is protected with buddy strapping to neutralize lateral forces on the finger until full fracture consolidation.
Mobilization
To prevent joint stiffness, the patient should be instructed to begin active motion (flexion and extension) of all nonimmobilized joints immediately after surgery.
Follow-up
The patient is reviewed frequently to ensure progression of hand mobilization.
In the middle phalanx, the fracture line can be visible in the x-ray for up to 6 months. Clinical evaluation (level of pain) is the most important indicator of fracture healing and consolidation.
Implant removal
The implants may need to be removed in cases of soft-tissue irritation.
In case of joint stiffness or tendon adhesion restricting finger movement, arthrolysis or tenolysis may become necessary. In these circumstances, the implants can be removed at the same time.













