ORIF - Plating
1. General considerations
After anatomical restoration and stable fixation of the ulnar fracture, relocation of the radial head will usually result. If surgery to the radial head is subsequently found to be necessary, it can be approached via a separate incision.
Occasionally, a proximal extension into a Speed and Boyd's approach can be made for additional access to the radial head via a single incision. Care must be taken not to harm the posterior interosseous nerve.
The use of a single approach to both bones of the forearm carries the significant risk of heterotopic bone formation and impairment of forearm function.
Monteggia fracture-dislocation
In Monteggia fracture-dislocations, the ulnar fracture is associated with a dislocation of the radial head.
In most cases, the radial head dislocates anteriorly or laterally; rarely posteriorly.
In Monteggia fracture-dislocations, anatomical reduction and stable fixation of the ulna are mandatory, to ensure stable relocation of the radial head.
Once operative fixation of the ulna has been completed, the surgeon must ensure the stability of the reduced radial head, preferably under image intensification.
2. Order of reduction and fixation
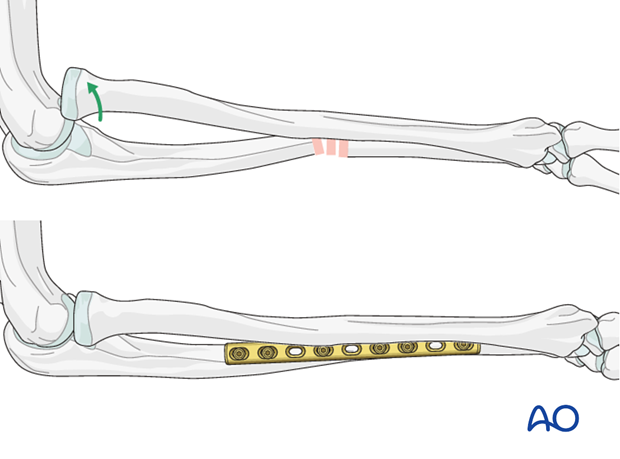
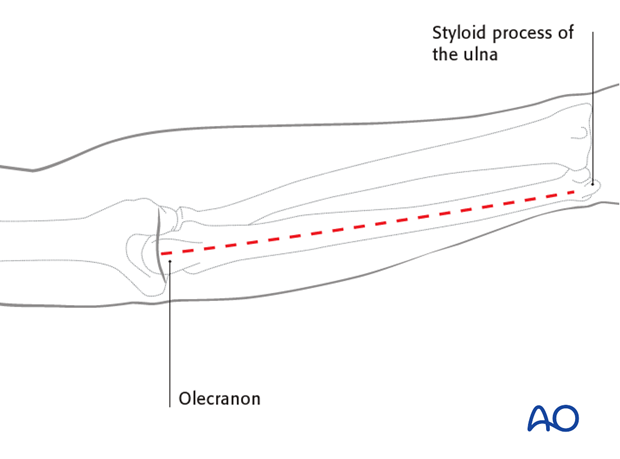
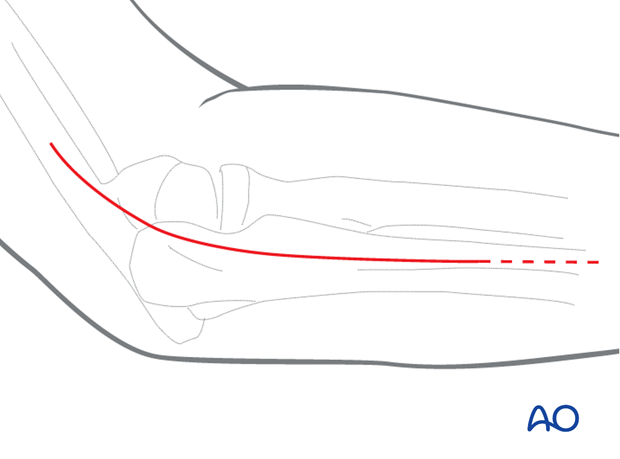
Anatomic reduction and fixation of the ulna is achieved first, through a standard posterior approach.
Check the position of the radial head, which reduces spontaneously in most of these cases (> 90%). The surgeon must determine the position of forearm rotation in which the radial head is most stable. This is very often in full supination after the radial head has dislocated anterolaterally. The stable rotational position of the forearm is that which will be used when postoperative splintage is applied.
If the radial head does not reduce correctly or if it dislocates on forearm movement (pronation/supination and flexion/extension), this may be due to either malreduction of the ulnar shaft, or there may be interposed soft tissue. If ulnar reduction is confirmed and radial head dislocation persists, access the radial head via a short lateral approach ...
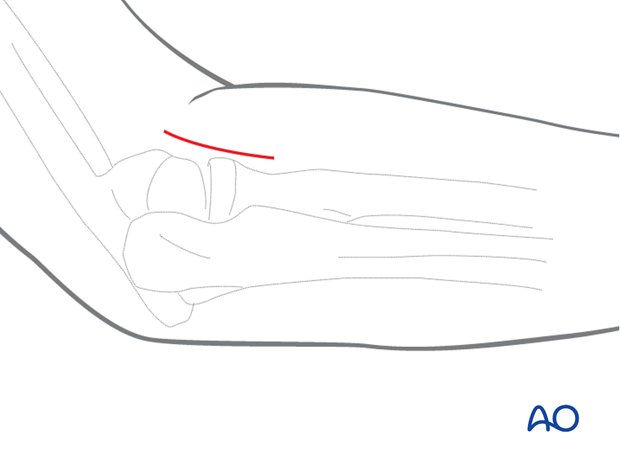
... or an extension into a Speed and Boyd approach (< 10%).
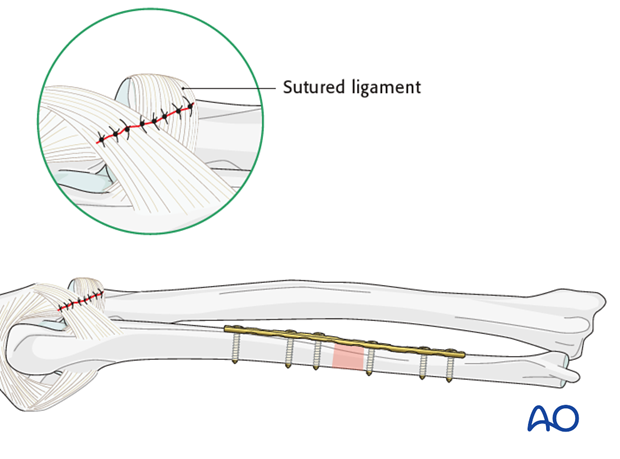
In cases of persisting radial head instability after anatomical fixation of the ulna, interposed annular ligament or the torn joint capsule is usually the cause and should be extracted from the joint and sutured.
3. Patient preparation
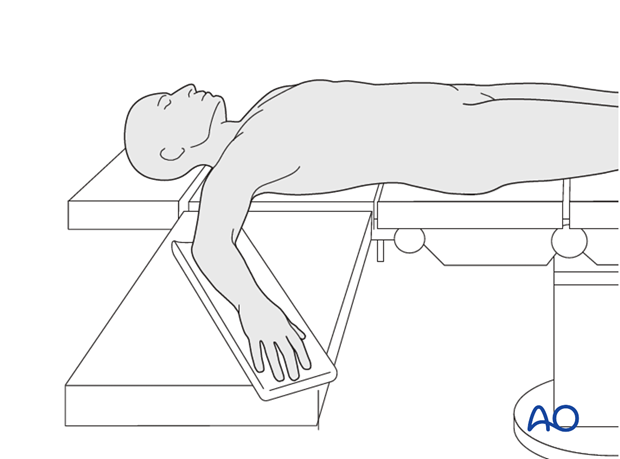
This procedure is normally performed with the patient in a supine position.
4. Reduction and fixation of the ulnar fracture
Monteggia simple ulnar fracture
For details on the reduction and fixation of the ulnar fracture see:

5. Monteggia fracture-dislocation
After fixation of the ulna, check the position of the radial head, which reduces in most cases spontaneously. If it did not reduce correctly or if it dislocates on forearm movement (pronation/supination and flexion/extension) …
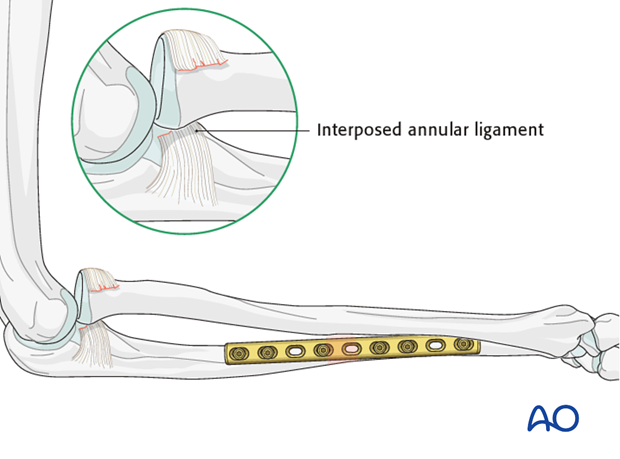
… access the anteriorly dislocated radial head with a lateral approach. In such cases, the usually interposed annular ligament and capsule are extracted and repaired.
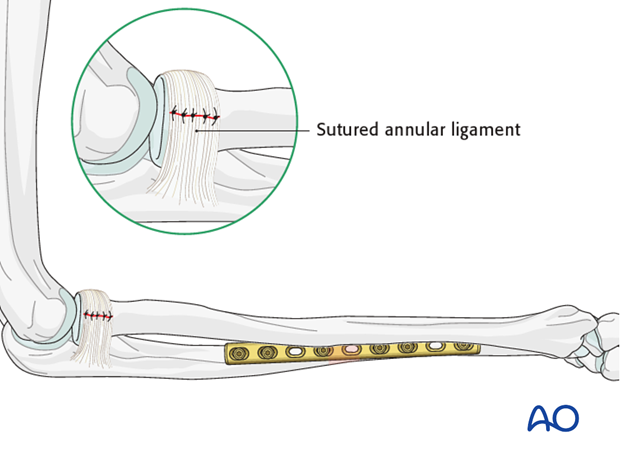
If the head was posteriorly dislocated, a Speed and Boyd’s approach is used to suture the dorsal capsular ligamentous defect.
Pitfall: persisting instability of radial head
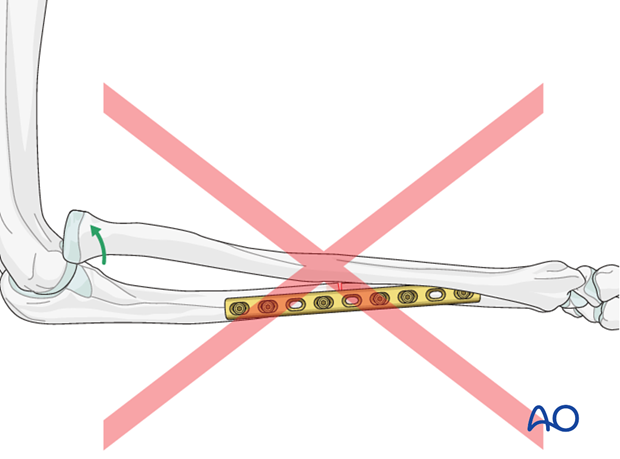
Be aware that malreduction of the ulna will lead to insufficient spontaneous anatomical reduction and/or instability of the radial head.
Such a situation demands revision of the ulnar fixation if optimal forearm function is to be restored.
6. Check of osteosynthesis
Check the completed osteosynthesis by image intensification. Make sure that the plate is at a proper location, the screws are of appropriate length and a desired reduction was achieved.
Confirm the rotational position which affords maximal stability of the radial head. This will be the forearm position in which postoperative forearm splinting will be applied.
7. Assessment of Distal Radioulnar Joint (DRUJ)
Before starting the operation the uninjured side should be tested as a reference for the injured side.
After fixation, the distal radioulnar joint should be assessed for forearm rotation, as well as for stability. The forearm should be rotated completely to make certain there is no anatomical block.
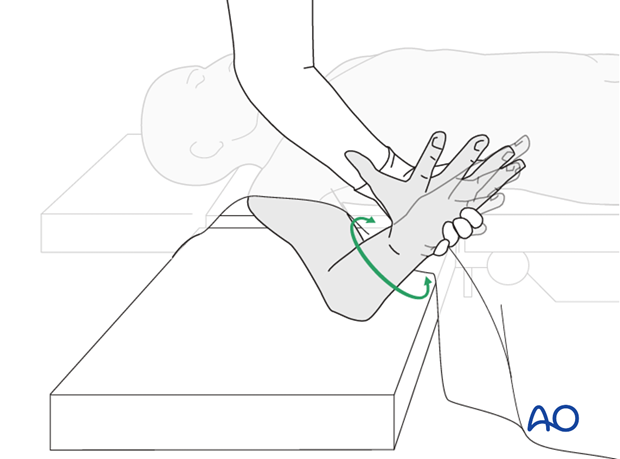
Method 1
The elbow is flexed 90° on the arm table and displacement in dorsal palmar direction is tested in a neutral rotation of the forearm with the wrist in neutral position.
This is repeated with the wrist in radial deviation, which stabilizes the DRUJ, if the ulnar collateral complex (TFCC) is not disrupted.
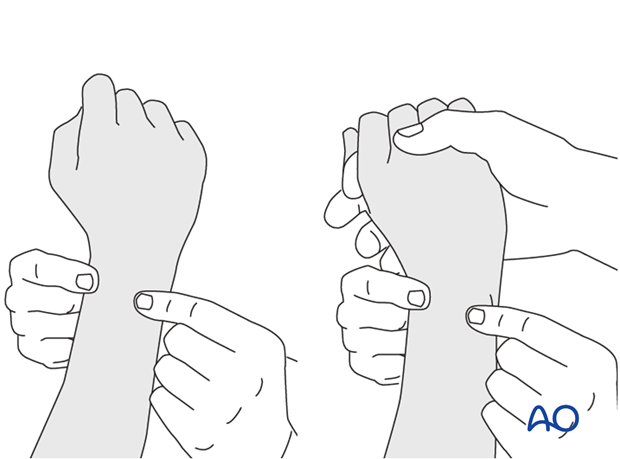
This is repeated with the wrist in full supination and full pronation.
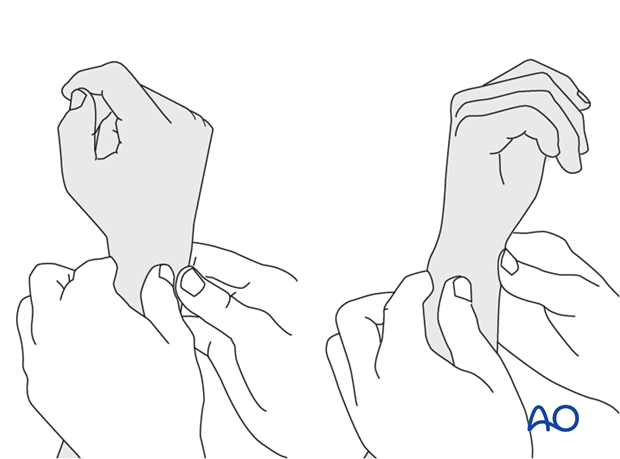
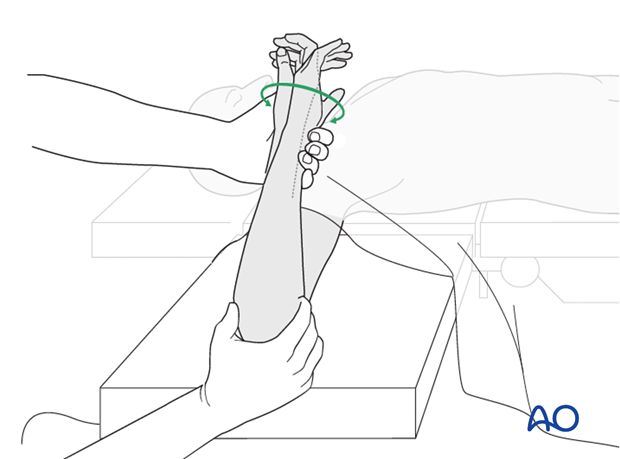
Method 2
In order to test the stability of the distal radioulnar joint, the ulna is compressed against the radius...
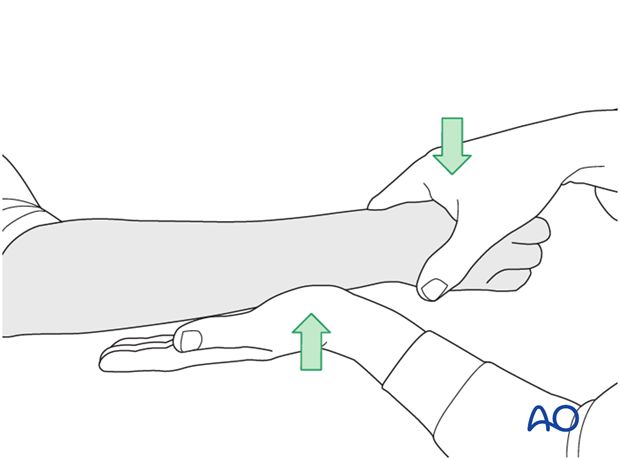
...while the forearm is passively put through full supination...
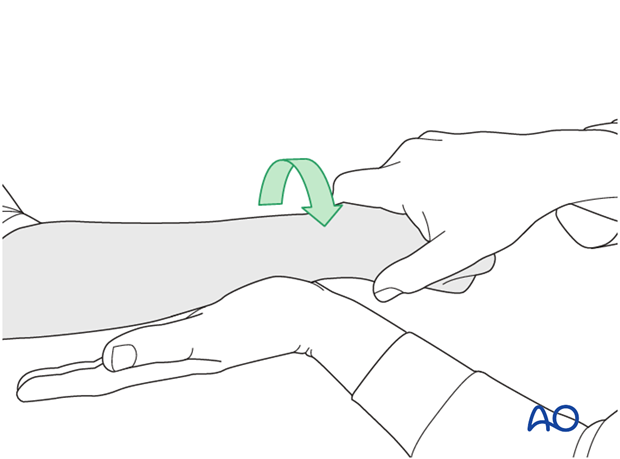
...and pronation.
If there is a palpable “clunk”, then instability of the distal radioulnar joint should be considered. This would be an indication for internal fixation of an ulnar styloid fracture at its base. If the fracture is at the tip of the ulnar styloid consider TFCC stabilization.
8. Case
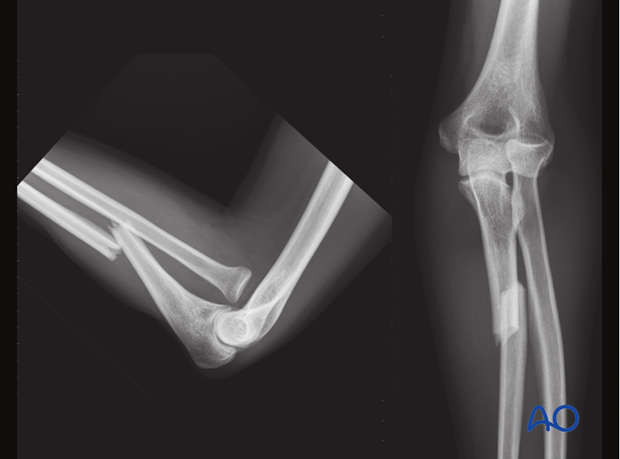
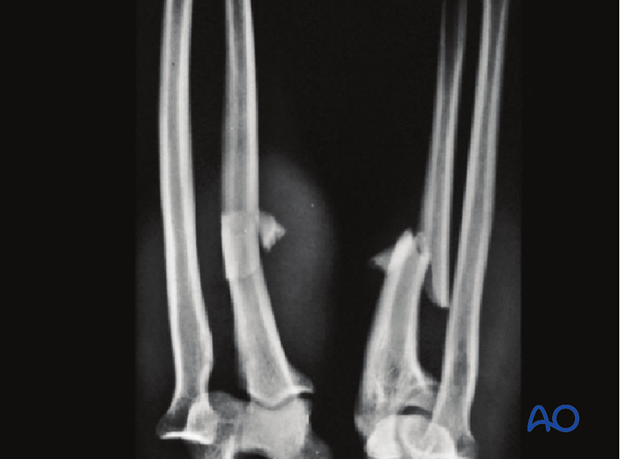
Monteggia fracture dislocation of the forearm, with a multifragmentary fracture of the ulnar shaft. Note the anterior radial head dislocation.

CT of elbow demonstrating anterior radial head dislocation.
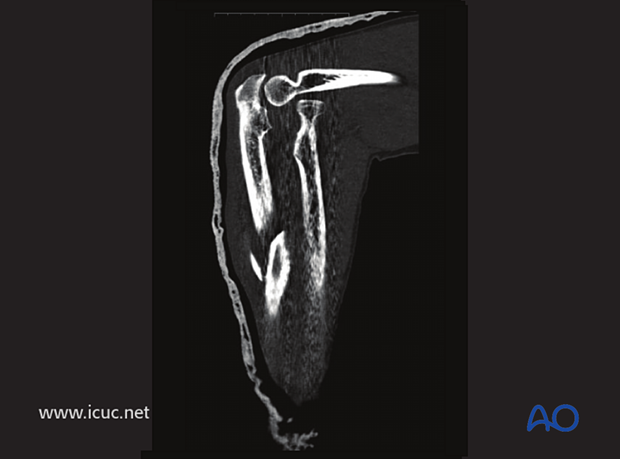
3D-CT.

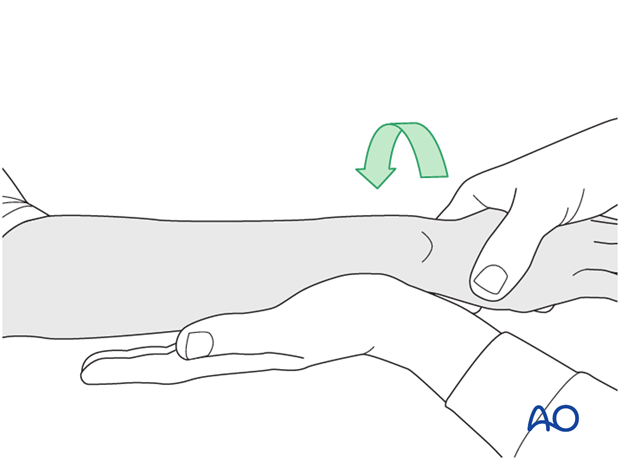
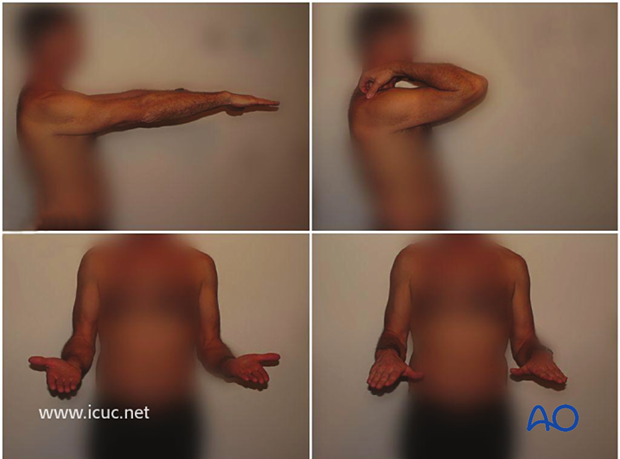
Preoperative check of posterior interosseous nerve that thumb extension is functioning.

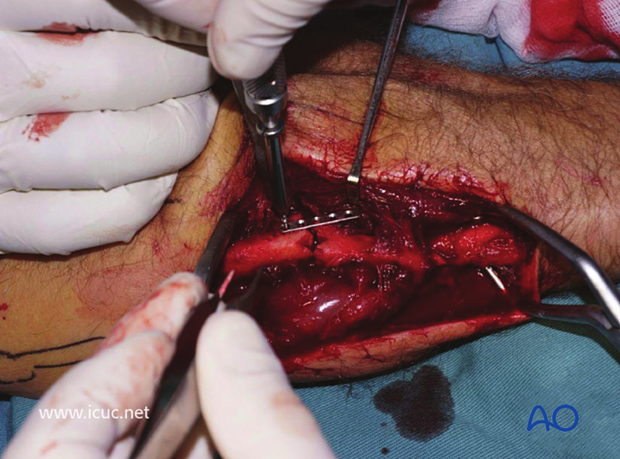
Mid ulnar incision in the internervous plane between flexors and extensors. Note the proximal ulna and distal ulna are marked.

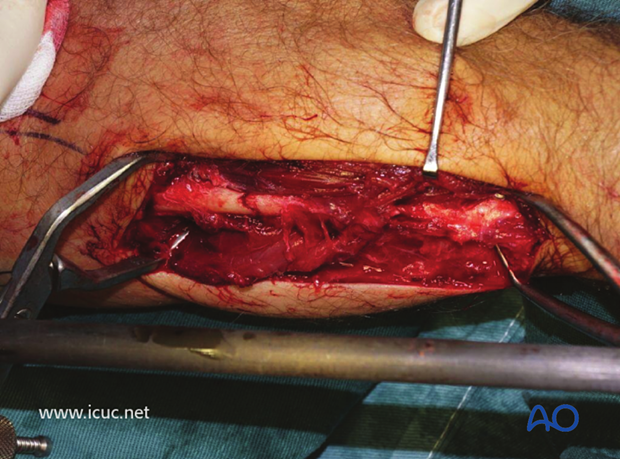
The ulnar border is subcutaneous at this site, so the fracture is easily exposed, with the extensors noted dorsally and the flexors volarly in this picture.
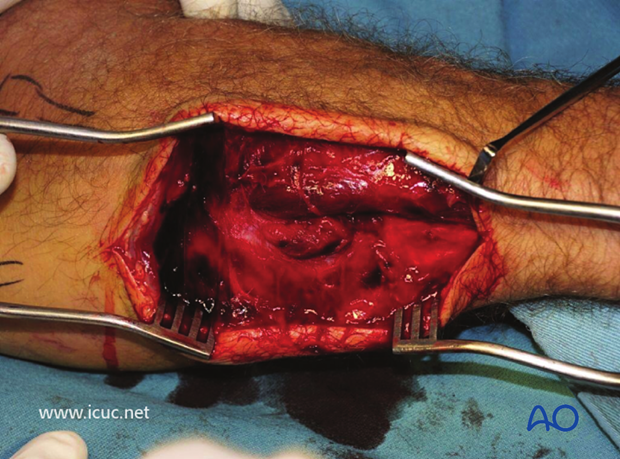
The fracture has been reduced with bone clamps.
As this fracture was multifragmentary and quite unstable, the surgeon decided to start by applying a micro plate to provide initial stability.
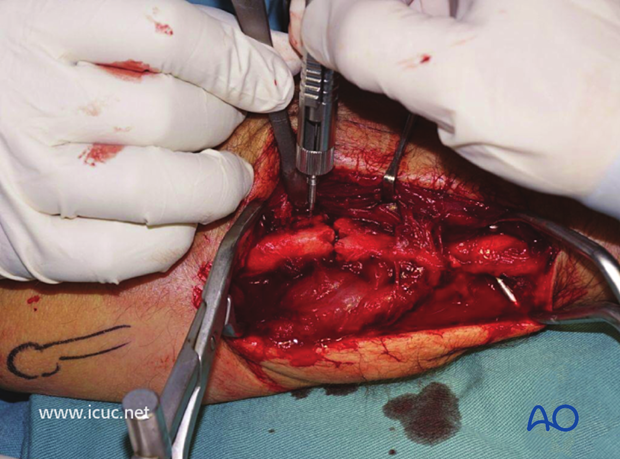
The microplate has been applied. This provides enough stability for a neutralization plate to be applied.
The small plate has reduced the proximal of the fractures with the fracture clamps still in place.

This image shows the reduction clamps and fixator has reduced the two fractures. Note that volar and dorsal soft tissues have been carefully left attached to the fracture fragments to ensure blood supply is maintained.
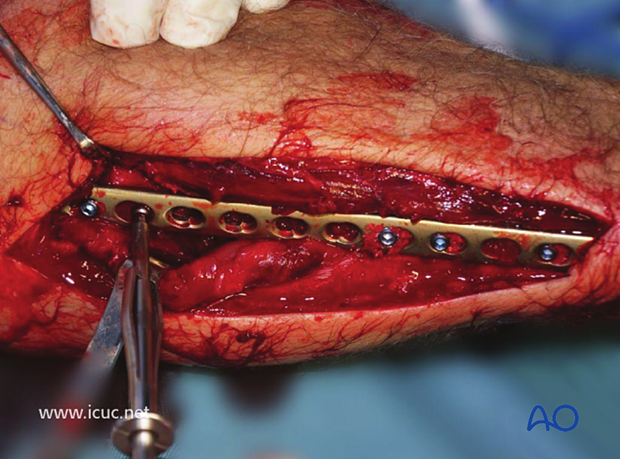
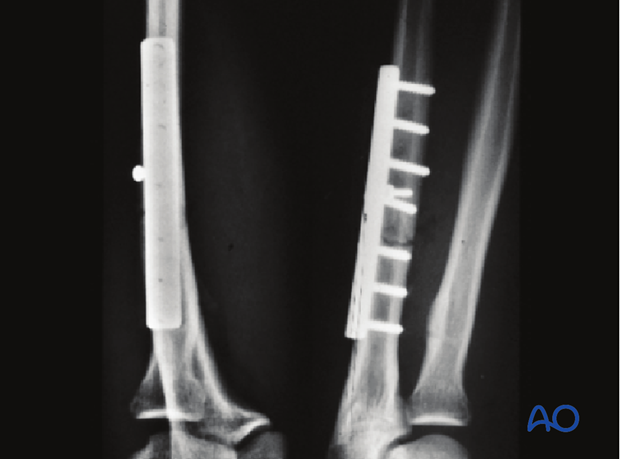
A very long LCP is used to provide enough fixation to this complex mid-ulnar fracture.

Proximal fixation has been obtained and a clamp is maintaining reduction before distal fixation.

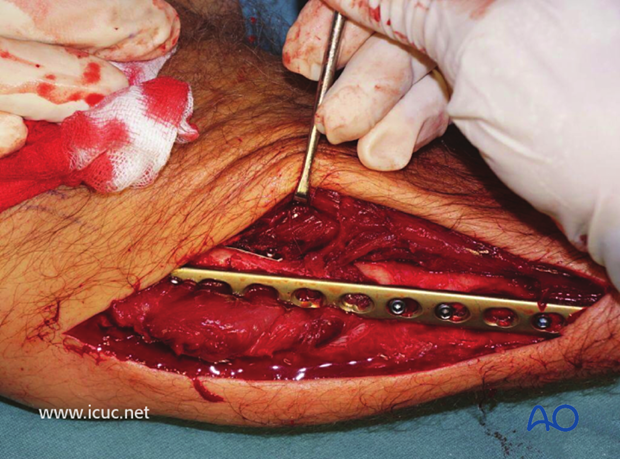
Fixation is achieved proximally and distally. Note the muscles are left attached to the volar and dorsal surfaces. Screws are only inserted into 50% of the holes.
Final fixation prior to closure.
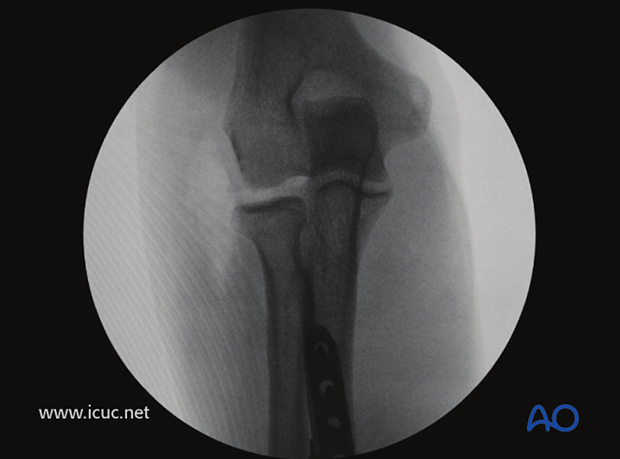
AP demonstrating nice reduction of the radiocapitellar joint.
Final closure

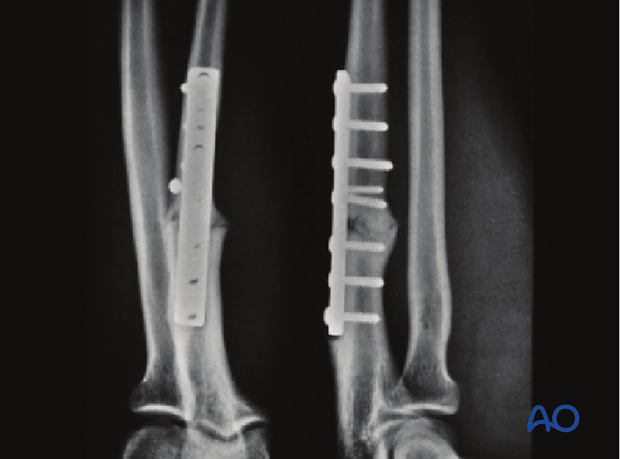
Bridging fixation with reduction plate in this complex Monteggia fracture.
Unfortunately, there is a slight gap at the fracture site and the healing might have been faster (see below) if the small plate would have been removed after the completion of the fixation.
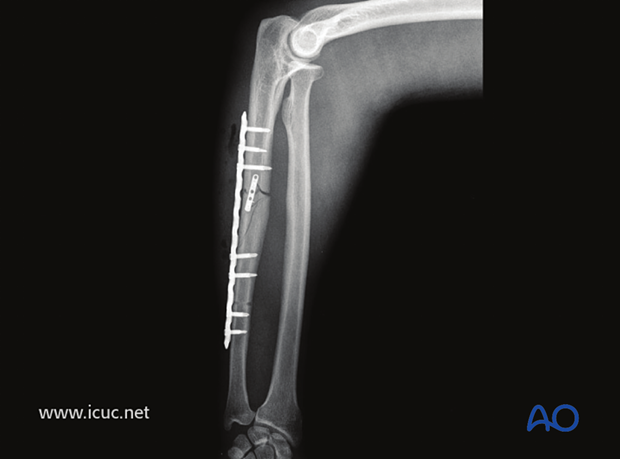
The fracture is still visible at four weeks, but the elbow is nicely reduced.
4-week clinical images of functioning elbow.

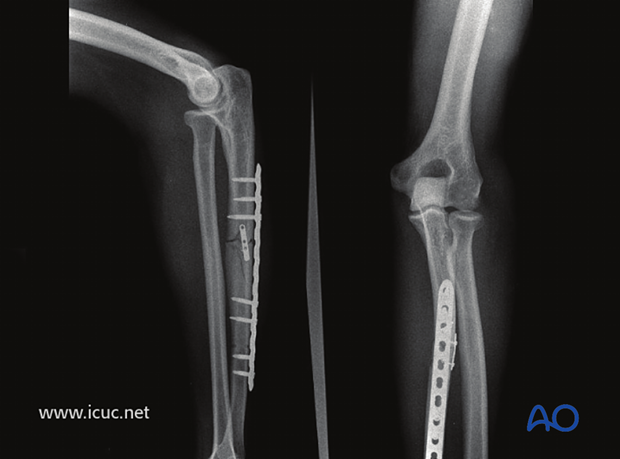
AP and lateral images at 49 weeks.
The fracture line is still visible but there is now abundant callus. It should unite but could also proceed to a non-union.
Final clinical result at 49 weeks
9. Postoperative treatment
Functional aftercare
Because of the dislocation of the radial head aftertreatment in Monteggia fractures differs from the usual functional aftercare in other forearm shaft fractures:
Following stable ulnar fixation and satisfactory location of the radial head, postoperative treatment consists of immobilization in a long-arm cast for 3 weeks, in the position of forearm rotation that at operation was determined to give maximal stability of the radial head: this is usually supination. The operated arm is elevated, and active mobilization of fingers is started early.
Only after removal of the cast can active wrist, elbow and gentle forearm rotation exercises be started.
X-ray control
Follow-up x-rays should be obtained according to local protocol. X-ray controls are advisable at 2 weeks to ensure that the radial head remains located and then after 6 weeks, 12 weeks, and 1 year to assess ulnar union.
Load bearing can be started at approximately 8 weeks after surgery, provided x-rays have shown satisfactory progress to ulnar healing.
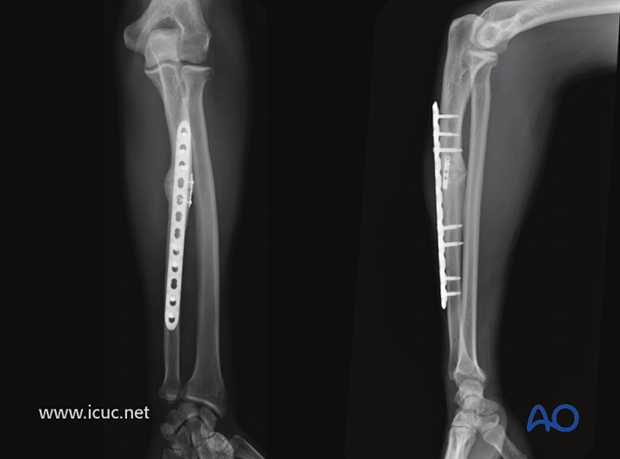
The case shows x-rays of a Monteggia fracture pre- and postoperatively.
Preoperative
Postoperative
After 1 year
Implant removal
In forearm shaft fractures, the issue of implant removal is controversial. As the ulna is not a weight-bearing bone, and as removal of plates can be a demanding procedure, implant removal is not indicated as a routine. There is a high risk of nerve damage associated with procedures to remove forearm plates.
Furthermore, as there is significant risk of refracture, most surgeons prefer not to remove plates from the forearm.
The general guidelines today are:
- removal only in symptomatic patients
- removal no earlier than 2 years after osteosynthesis.
References
- Bednar DA, Grandwilewski W (1992) Complications of forearm-plate removal. Can J Surg; 35(4):428-431.
- Langkamer VG, Ackroyd CE (1990) Removal of forearm plates. A review of the complications. J Bone Joint Surg Br; 72(4):601-604.
- Rosson JW, Shearer JR (1991) Refracture after the removal of plates from the forearm. An avoidable complication. J Bone Joint Surg; 73(3): 415-417.
- Heim D, Capo JT (2007) Forearm, shaft. Rüedi TP, Buckley RE, Moran CG (eds), AO Principles of Fracture Management, Vol. 2. Stuttgart New York: Thieme-Verlag, 643-656.













