Oblique ulnar fracture: lag screw and plate fixation
1. Principles
Options for fixation
Note: The first principle (A) will be described using two different techniques.
Absolute stability
Interfragmentary compression
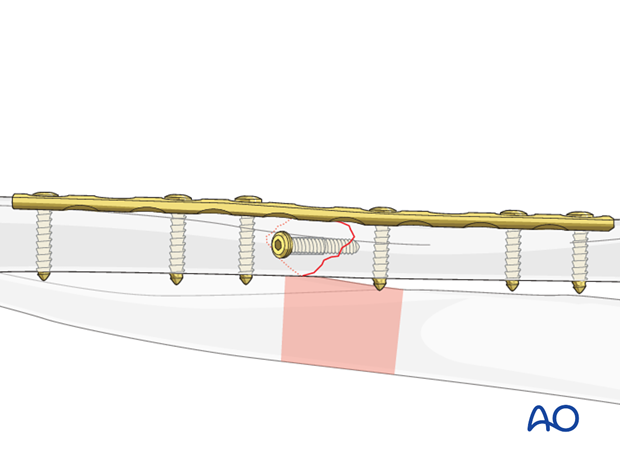
Interfragmentary compression can be achieved by a lag screw, inserted either through a plate hole (1), or separate from the plate (2).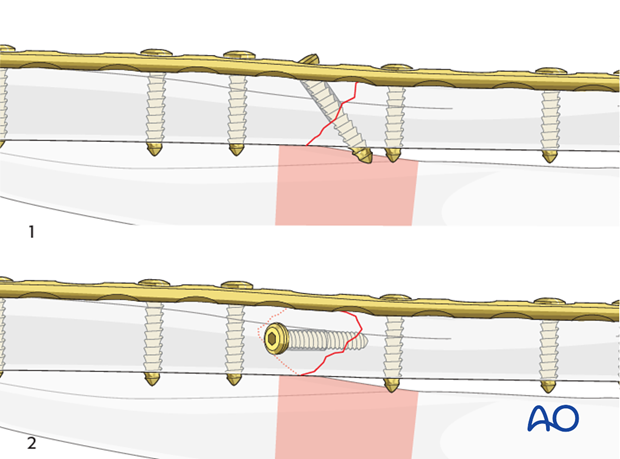
Dynamic compression principle
Axial compression
Interfragmentary compression can be achieved by loading the oblique fracture site axially, using specific techniques.Axial compression, using self-compressing plates (DCP, LC-DCP, LCP, etc.), is achieved by eccentric screw placement.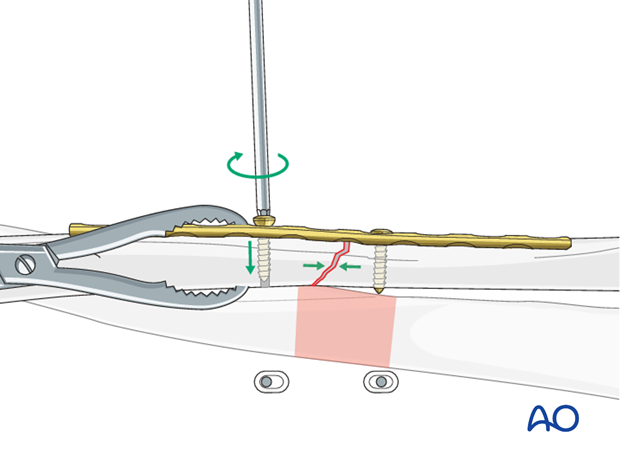
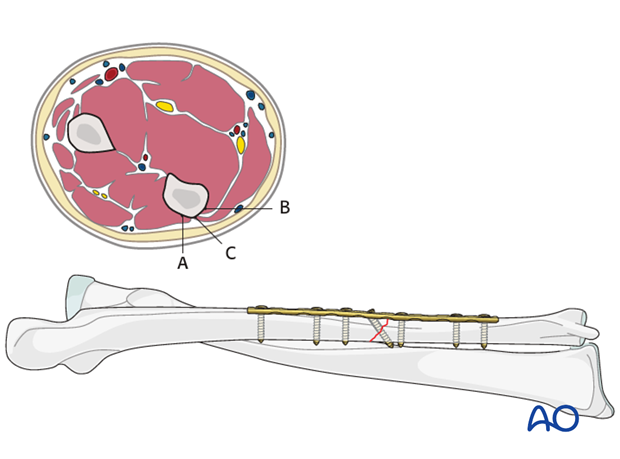
Plate position
While plate position on the tensile (subcutaneous) aspect of the ulna (C) is biomechanically preferable, plate prominence can be a problem and cause irritation. To avoid too superficial position of the plate, it can be placed towards positions (A) or (B) where it will be covered by the muscle compartment.
In oblique fractures, the plate position should consider the fracture morphology. It is preferable to insert the lag screw through the plate, if possible.
In the following procedure, we demonstrate the plate positioned deep to the extensor carpi ulnaris muscle (A).
2. Reduction
Open and anatomical reduction
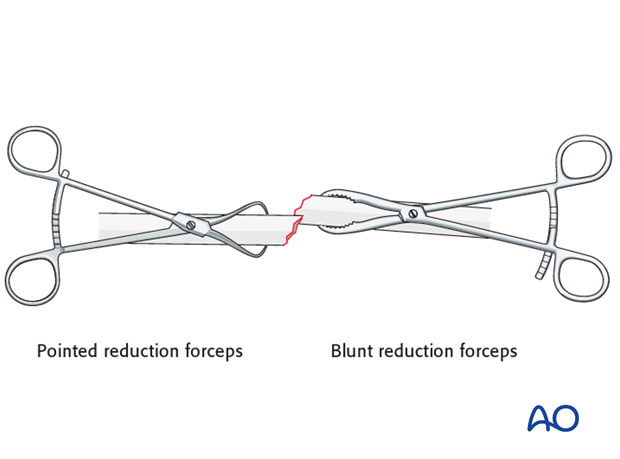
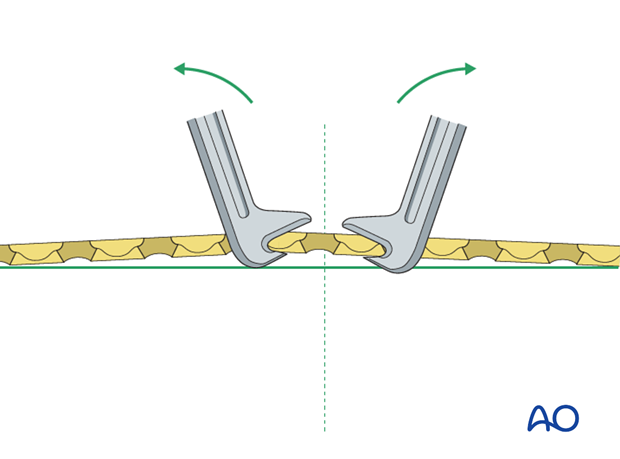
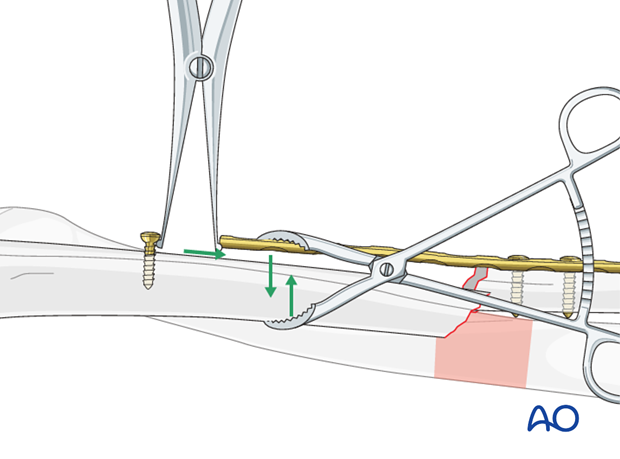
Reduce the fracture anatomically, using a reduction forceps on each main fragment. The use of blunt, as opposed to pointed, reduction forceps can be helpful, particularly if greater forces are required.
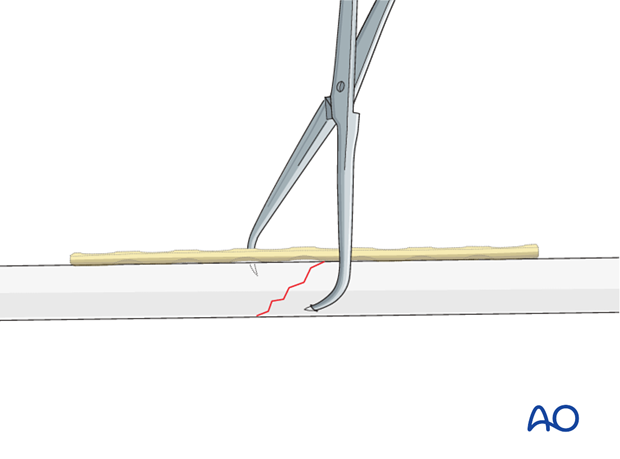
A small bone lever can be used to reduce the fragments.
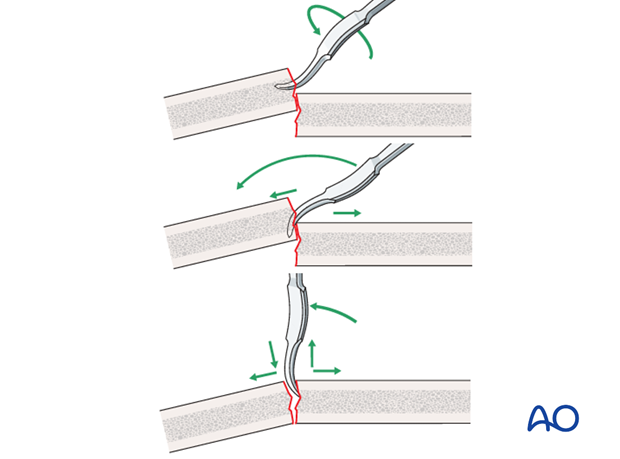
Reduction of overlapping oblique fractures can sometimes be achieved by twisting a reduction forceps, thereby lengthening the fracture.
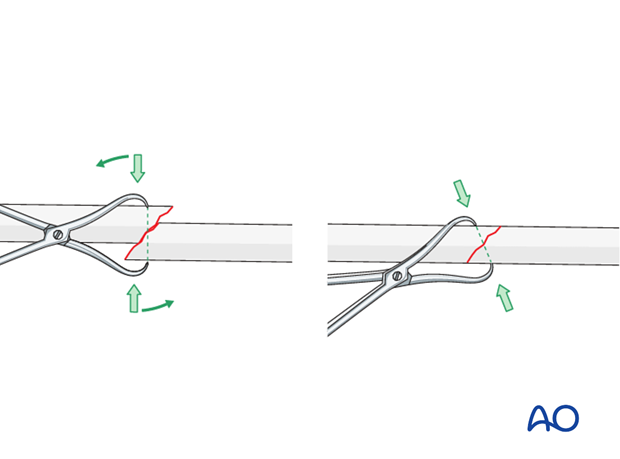
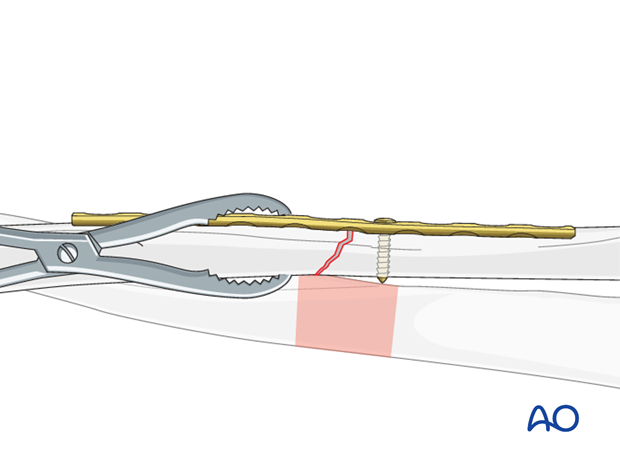
Maintain fracture reduction
Maintain the fracture reduction with pointed reduction forceps. Place the forceps such that it will not interfere with the planned plate position.
3. Plate length and number of screws
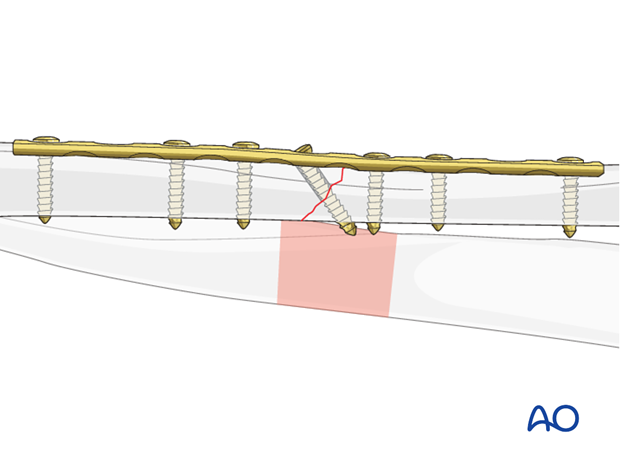
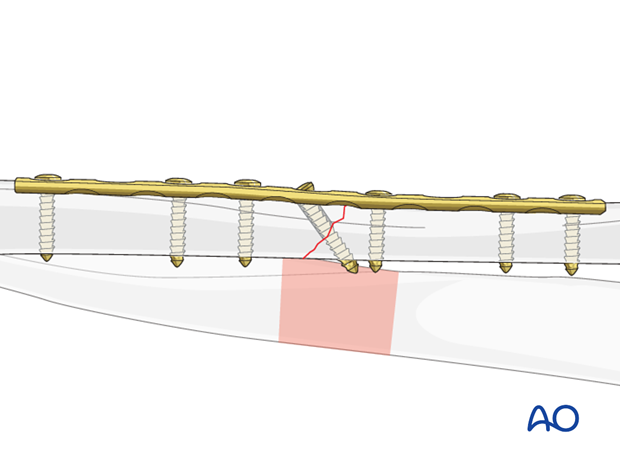
4. Fixation – lag screw as primary fixation device separate from plate
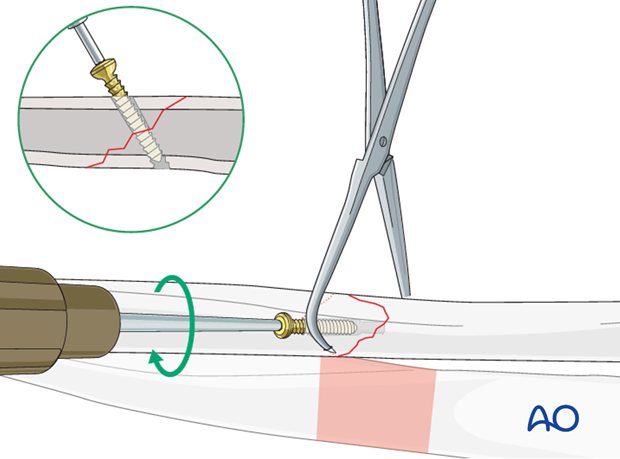
Drill gliding hole
Ensure that the direction of the drill is as perpendicular to the fracture plane as possible.
Thread hole: guide in gliding hole
Measure for screw length
Use a depth gauge to measure for screw length.
Measure the longer side of the oblique drill hole, as shown, to ensure sufficient screw length.
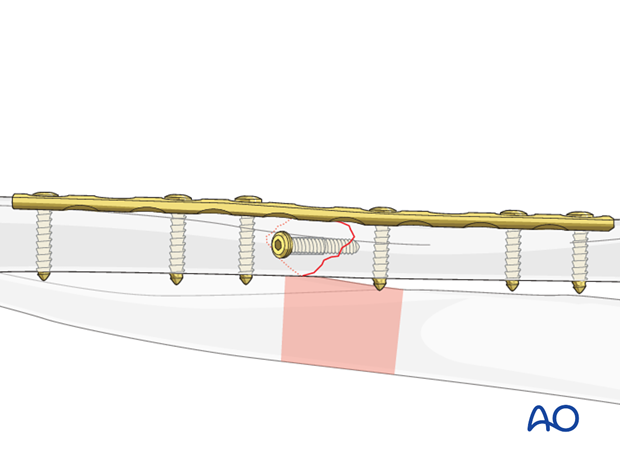
The lag screw should protrude 1-2 mm through the opposite cortex to ensure maximal thread purchase. However, too long a screw may be tender, or injure soft tissues.
Tap the thread hole
This maneuver is not necessary when using self-tapping screws.
Lag screw insertion
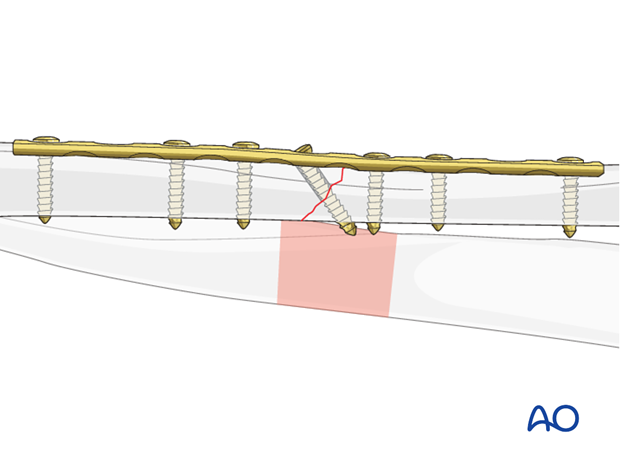
Help to maintain the reduction by leaving the pointed reduction forceps in situ.
Neutralization (protection) plate
The pointed reduction forceps can then be removed.
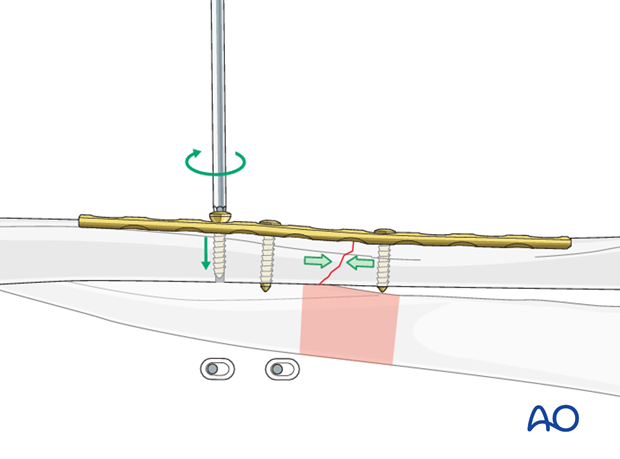
5. Fixation – lag screw as primary fixation device through the plate
If this technique is used, then axial compression must not be applied via the plate.
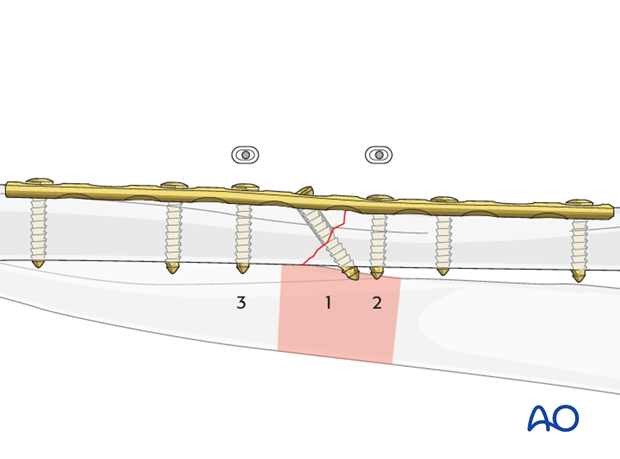
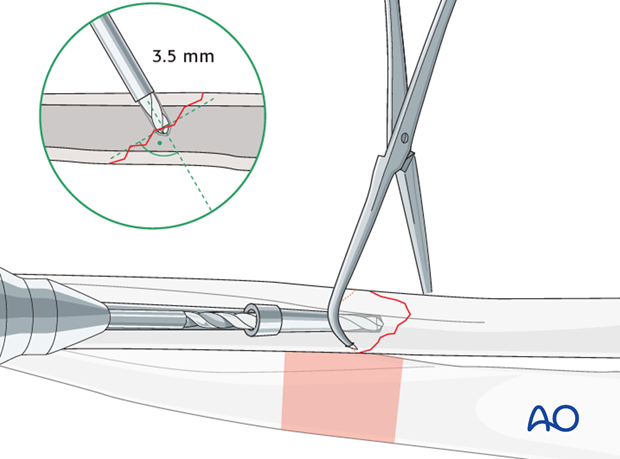
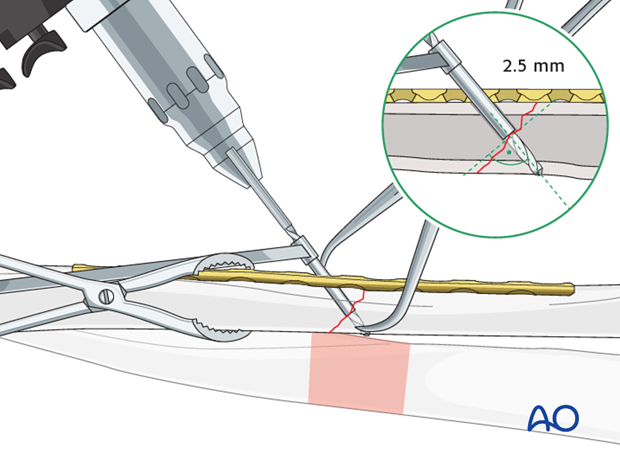
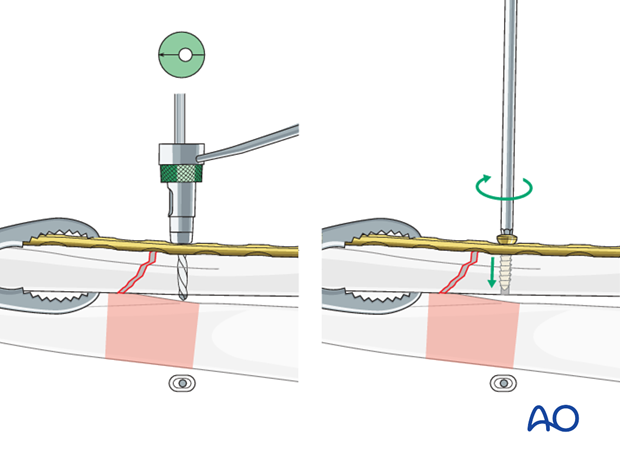
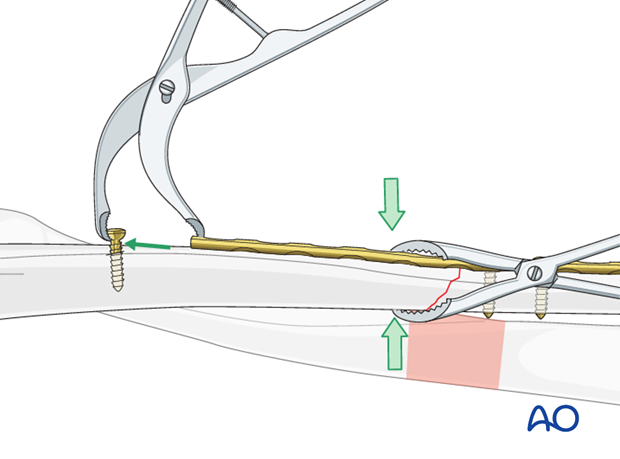
Drill gliding hole through plate
A perfectly contoured plate is now applied to the surface of the anatomically reduced fracture and fixed to one main fragment, either with a neutral screw, or with a bone forceps as illustrated. The interfragmentary lag screw can then be inserted through the appropriate plate hole.
Using a 3.5 mm drill sleeve and a 3.5 mm drill bit, drill a gliding hole in the near cortex.
Ensure that the direction of the drill is as perpendicular to the fracture plane as possible.
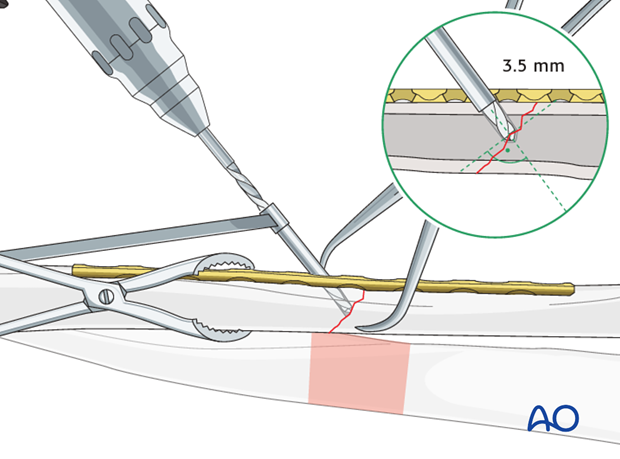
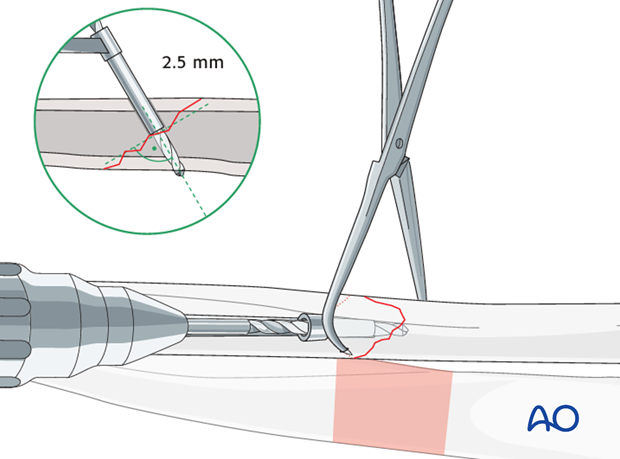
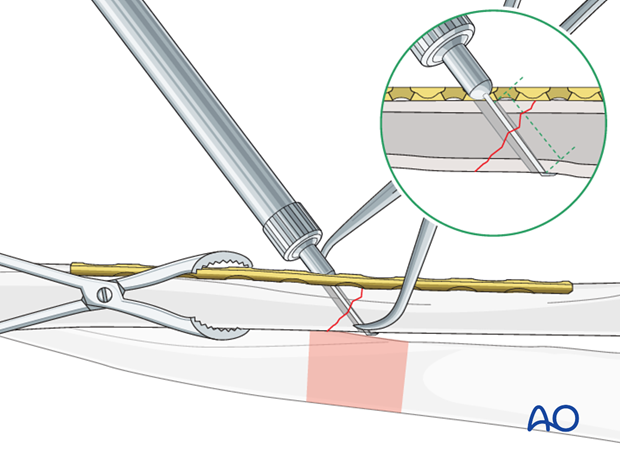
Thread hole: guide in gliding hole
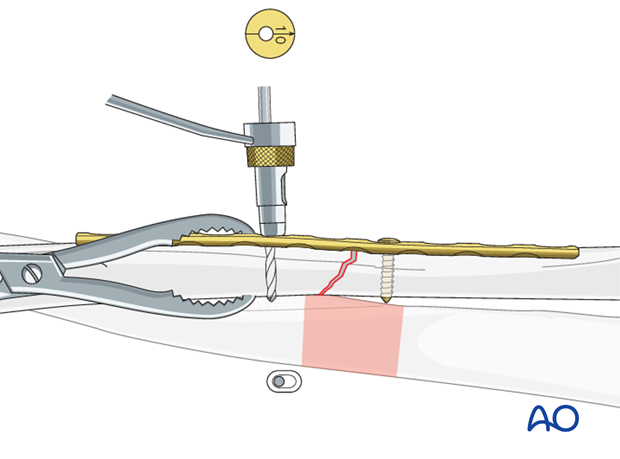
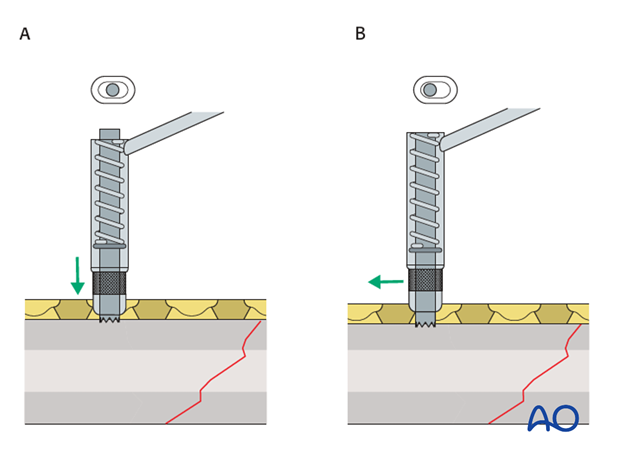
Measure for screw length
Measure the longer side of an oblique drill hole, as shown, to ensure sufficient screw length.
A screw should protrude 1-2 mm through the opposite cortex to ensure maximal thread purchase. However, too long a screw may be tender, or injure soft tissues.
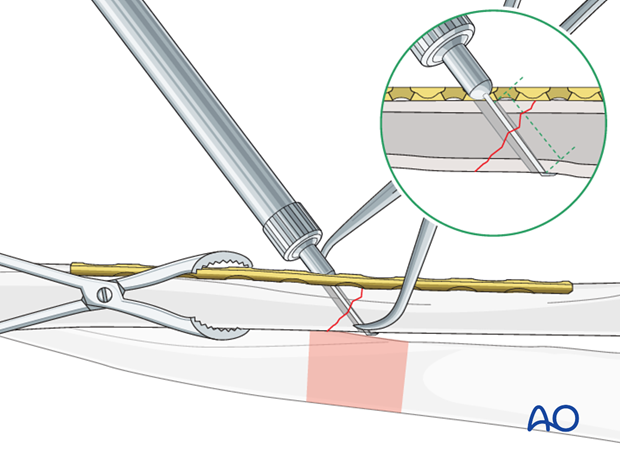
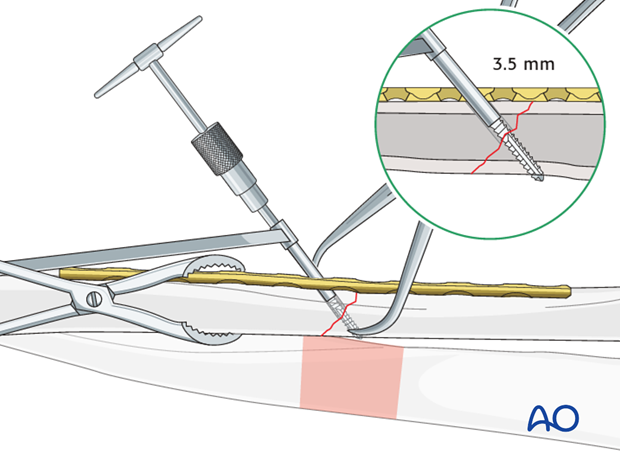
Tap the pilot hole
This maneuver is not necessary when using self-tapping screws.
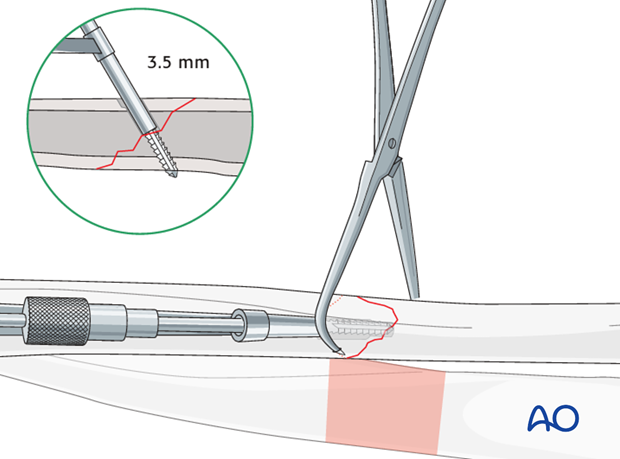
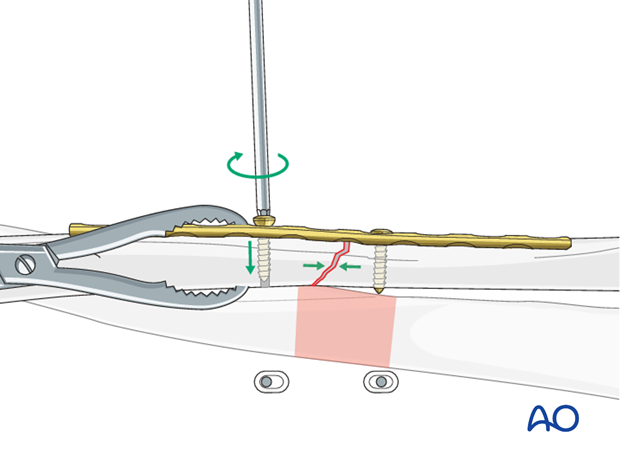
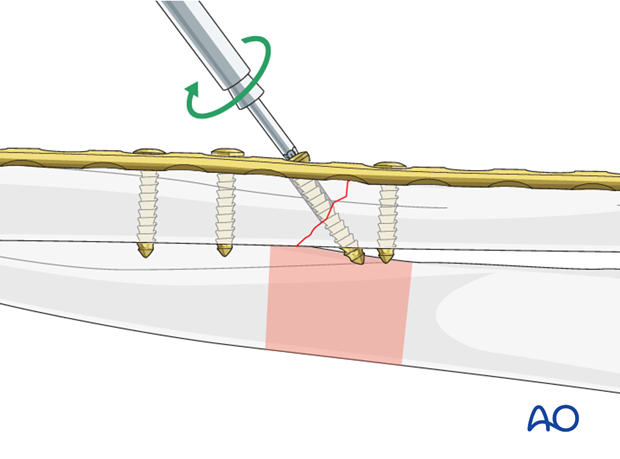
Lag screw insertion
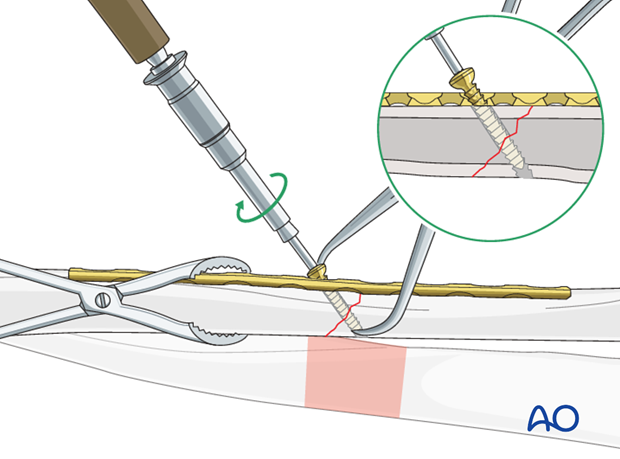
Insert the plate screws
6. Fixation – compression plating with an additional lag screw
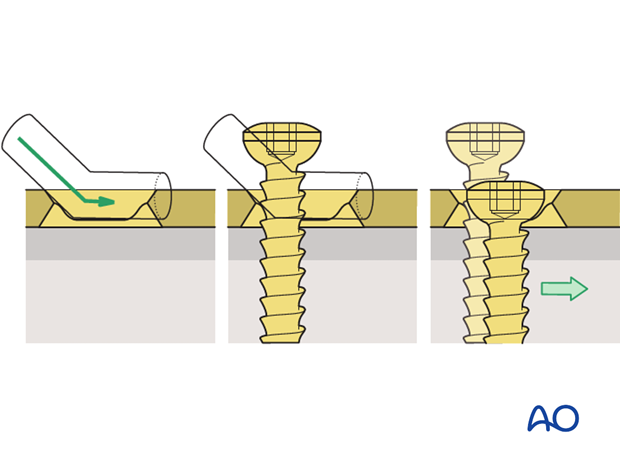
Prebending the plate
The solution to this problem is to “over-bend” the plate so that its centre stands off 1-2 mm from the anatomically reduced fracture surface.
When the neutral side of the plate is applied to the bone, slight gapping of the cortex will occur directly underneath the plate.
As the load screw is tightened, the tension generated in the plate compresses the fracture evenly across the full diameter of the bone.

Insert 1st screw
Note: Because of the design of the LC-DCP holes, the neutral drill guides for the LC-DCP have a very slightly eccentric hole and an arrow, which needs always to point towards the fracture line.
Maintain reduction
Insert 2nd screw eccentrically
Note: the arrow on the drill sleeve has to point towards the fracture line.
Tighten screw
Insert additional screws
As the second eccentric screw is tightened, the first eccentric screw in the same fragment needs to be loosened slightly to allow the plate to slide on the bone.
Pearl: alternative drill sleeve
Lag screw
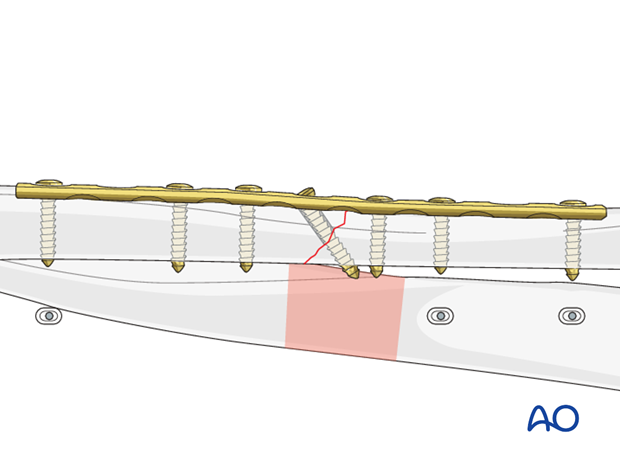
Completed osteosynthesis

7. Check of osteosynthesis
Check the completed osteosynthesis by image intensification. Make sure that the plate is at a proper location, the screws are of appropriate length and a desired reduction was achieved.
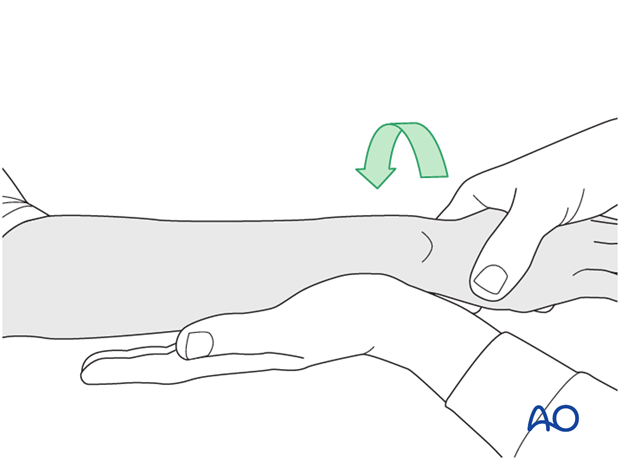
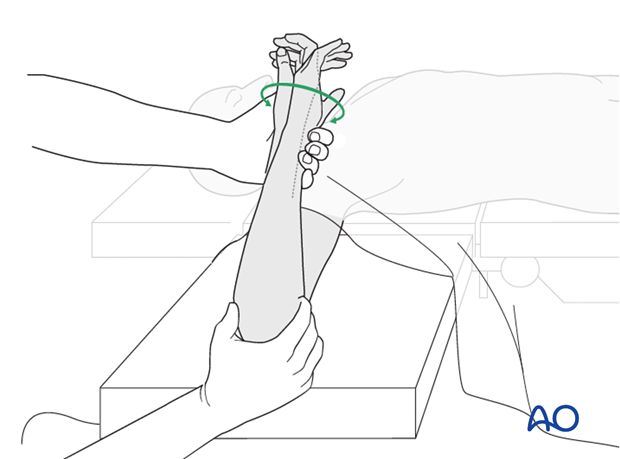
The elbow should be stabilized at the epicondyles and the forearm rotation should be checked between the radial and ulnar styloids.
8. Assessment of Distal Radioulnar Joint (DRUJ)
Before starting the operation the uninjured side should be tested as a reference for the injured side.
After fixation, the distal radioulnar joint should be assessed for forearm rotation, as well as for stability. The forearm should be rotated completely to make certain there is no anatomical block.
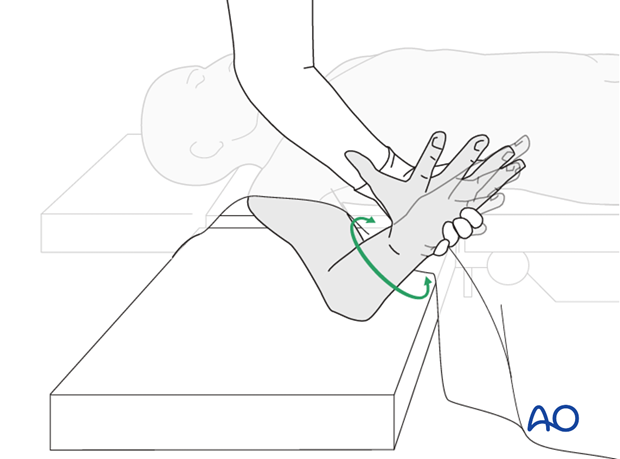
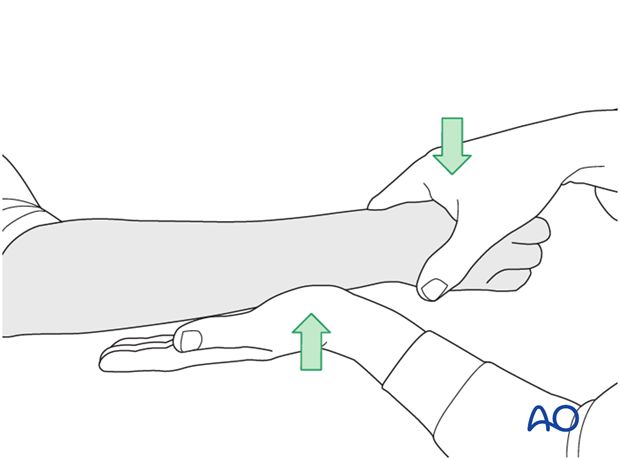
Method 1
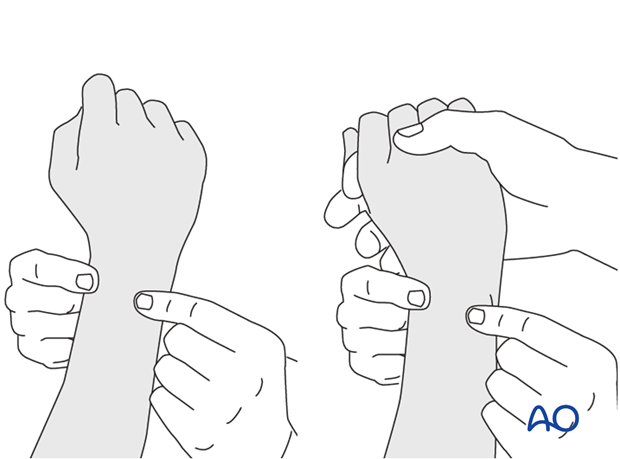
The elbow is flexed 90° on the arm table and displacement in dorsal palmar direction is tested in a neutral rotation of the forearm with the wrist in neutral position.
This is repeated with the wrist in radial deviation, which stabilizes the DRUJ, if the ulnar collateral complex (TFCC) is not disrupted.
This is repeated with the wrist in full supination and full pronation.
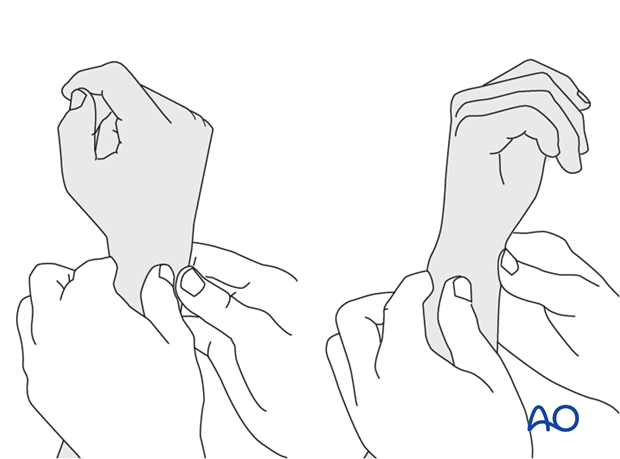
Method 2
In order to test the stability of the distal radioulnar joint, the ulna is compressed against the radius...
...while the forearm is passively put through full supination...
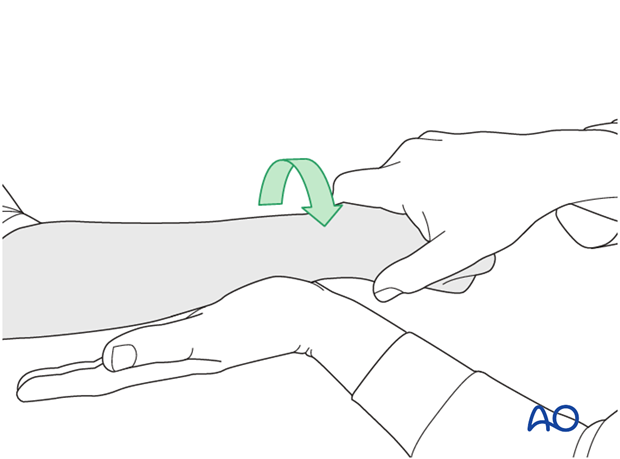
...and pronation.
If there is a palpable “clunk”, then instability of the distal radioulnar joint should be considered. This would be an indication for internal fixation of an ulnar styloid fracture at its base. If the fracture is at the tip of the ulnar styloid consider TFCC stabilization.