ORIF - Plate
1. Introduction
The principle of this procedure is first to reduce and fix the articular block, which is then fixed to the shaft using a plate.
Anatomical reduction of the joint surface is essential to prevent chronic instability or posttraumatic degenerative joint disease.
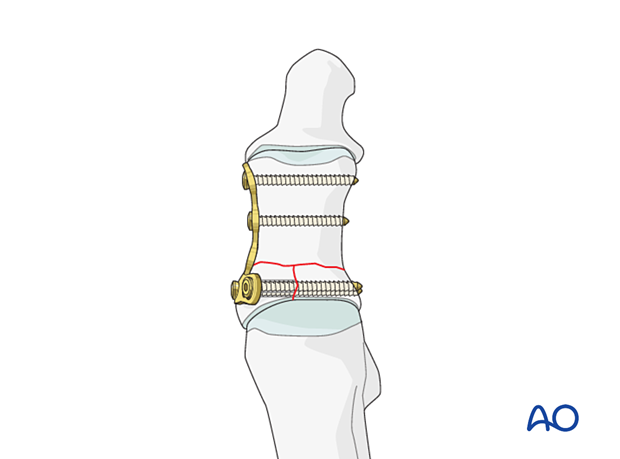
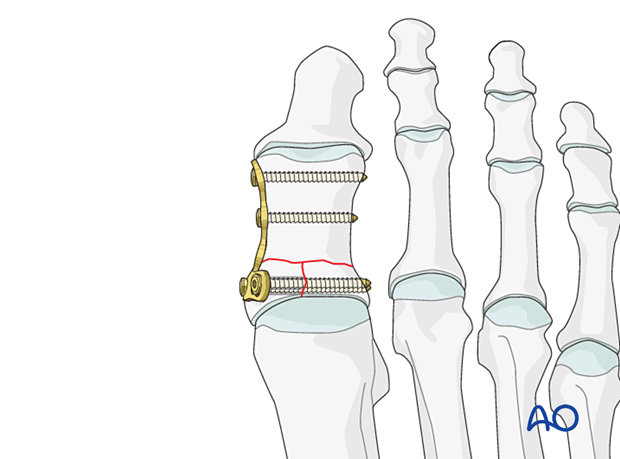
Depending on the fracture pattern, the plate can be applied medially or dorsally to allow lag screw insertion through the plate, perpendicular to the fracture plane.
To illustrate the principles, we will show medial plate fixation for a simple complete articular fracture where the articular fracture component lies in the sagittal plane.
As a dorsal plate will cause less soft tissue irritation than a medial plate, some surgeons prefer dorsal plate application independently of the fracture patterns direction. This would only be feasible for the illustrated fracture if the articular block is fixed with a medially inserted lag screw (or K-wire), followed by a dorsal plate application. Alternatively, a locking plate would need to be used.
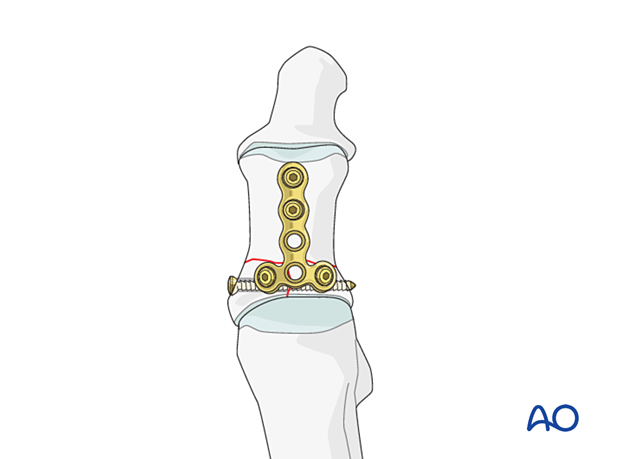
Plate selection
A 2.0 or 2.4 T-plate is typically used. The length of the plate should allow at least two points of fixation in the shaft.
Toe fractures versus long bone fractures
Toe fractures are different from long bone fractures.
- The bones are very small
- Fracture gaps are small
- Fixation devices don't need to counter large forces
Thus, following the AO principles is less critical than for long bones, and often isolated screws or K-wires alone will work satisfactorily.
Restoration of length, rotation, and angulation are important for cosmesis.
The hallux is particularly critical due to its importance for walking.
Timing of surgery
The timing of surgery is influenced by the soft tissue injury and the patient's physiologic status.
Dislocation or injuries associated with the skin at risk requires immediate intervention regardless of the amount of soft tissue swelling.
If possible, swelling should be significantly decreased before surgery, which can take up to two weeks in some instances.
Open fractures should be promptly irrigated and debrided, and treated with antibiotics. Definitive fracture fixation may not be possible during this setting.
Forefoot fractures do not contribute to physiologic instability. If there is no soft tissue at risk, urgent intervention is not required.
2. Patient preparation and approach
Patient preparation
This procedure is typically performed with the patient placed supine and the knee flexed 90°.

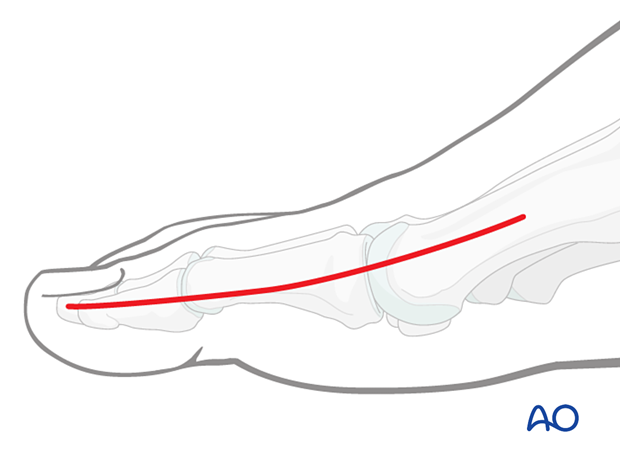
Approach
These fractures can be approached through either the:
Extension of the medial incision allows for visualization of the entire dorsal surface.
3. Reduction
Visualization
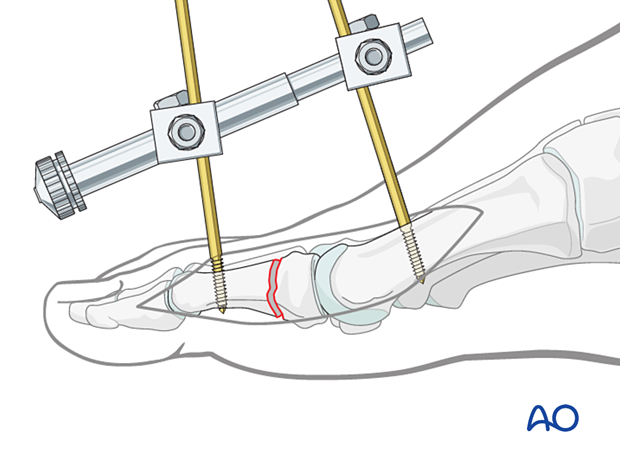
Visualization of the joint is challenging but may be improved by longitudinal distraction or a percutaneous reduction aid such as a mini distractor.
Visualization of the joint may be further improved by releasing the dorsal insertion of the extensor hallucis brevis.
Re-establishment of length
The fracture will shorten through the comminuted region. Length may be restored either by manual traction or the use of a distractor.

Irrigation
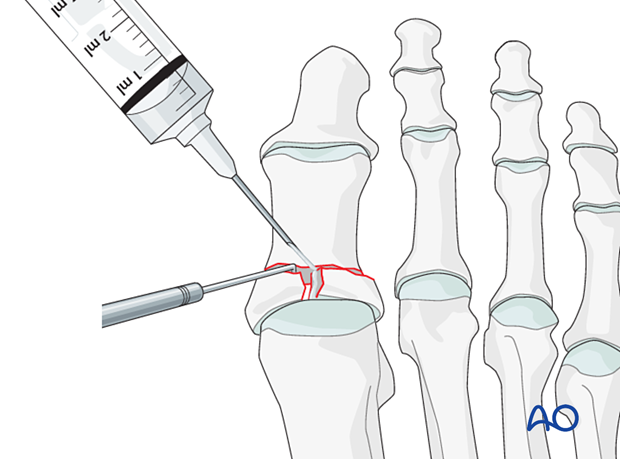
Clean the fracture using a dental pick. Direct suction or irrigation is helpful.
The fracture edges are exposed, and the fragment mobility is assessed. It is essential to maintain the vascularity of small fragments.
The extent of articular involvement is assessed, including separate osteochondral fragments.
If reconstruction of the articular surface is not feasible, a fusion of the joint should be considered.
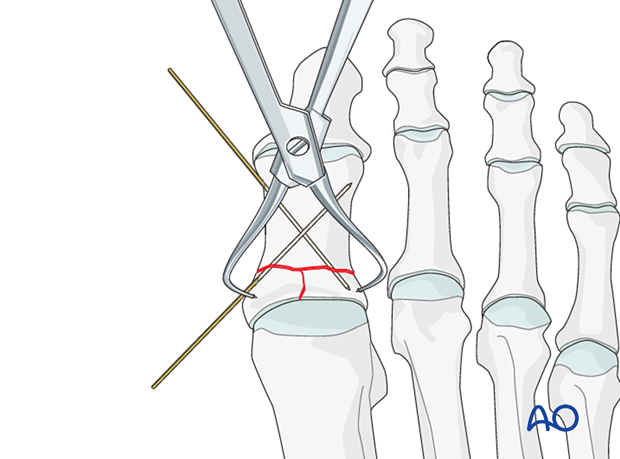
Reduction and temporary fixation of the articular block with simple fracture
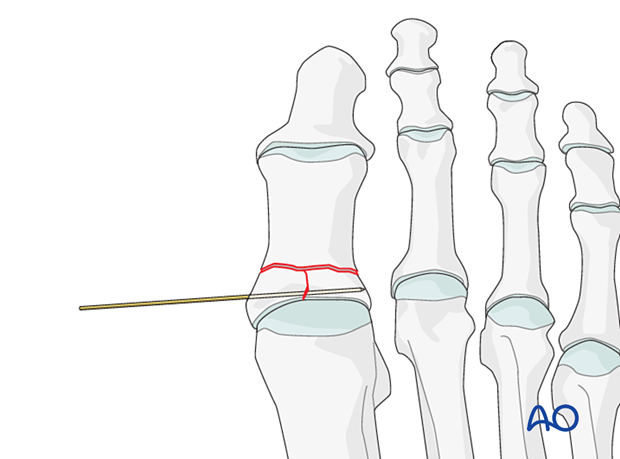
Reduction using forcepsReduce and temporarily fix the articular block with pointed reduction forceps.
Be careful not to apply excessive force as this can lead to fragmentation. If possible, apply the reduction clamp so that the forces created by the clamp are at right angles to the fracture line. This clamp placement helps in reducing the fracture and in applying compression.
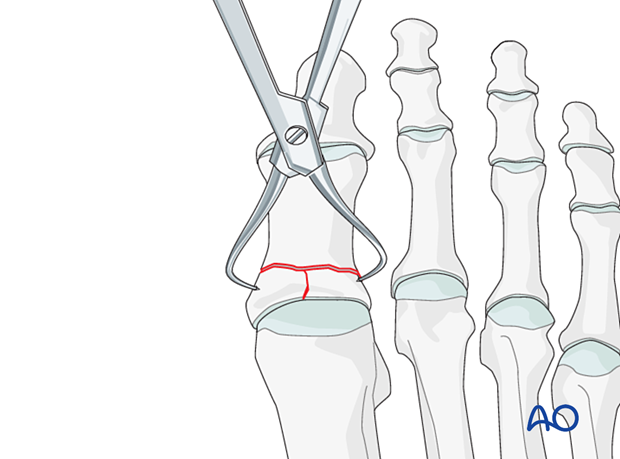
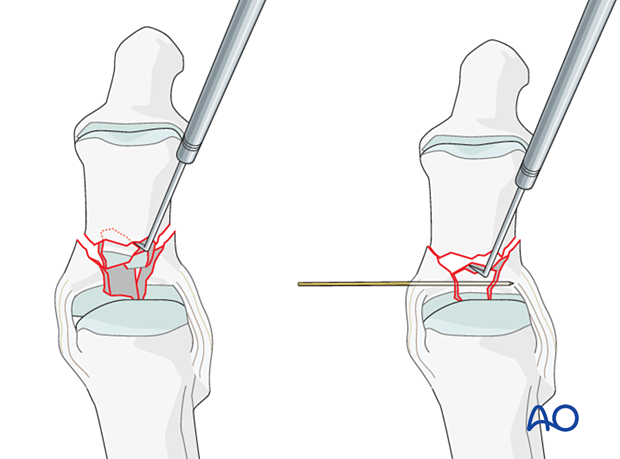
Insert a K-wire into one of the articular fragments and use it as a joystick to reduce the articular block.
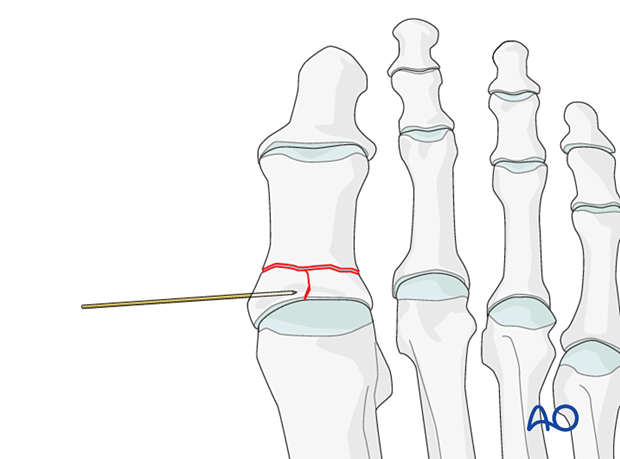
Once reduction is accomplished, advance the wire to secure the reduction.
Reduction and temporary fixation of impacted articular segment
Centrally impacted fragments are not reducible by ligamentotaxis as they are devoid of soft-tissue attachments.
Therefore, an indirect or direct reduction is necessary to restore alignment, length, and rotation.
The key to fixing compression fractures is restoring the joint surface to as close as normal as possible and supporting the reduction with internal fixation and possible bone graft.
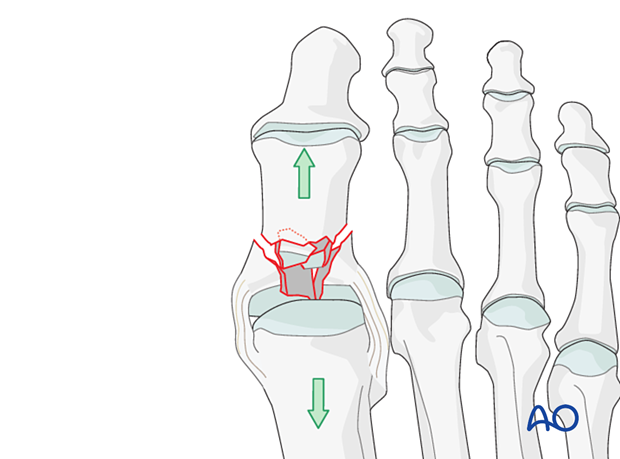
Using a K-wire, or dental pick, the fragments are disimpacted and pushed towards the head of the metatarsal, which is used as a template to ensure congruity of the articular surface of the hallux.
Degenerative joint disease may follow if a cartilage step-off greater than 1 mm remains.
Since the metaphyseal cancellous bone is impacted, a void may be created by its disimpaction.
A void jeopardizes the fracture in two ways:
- It is a very unstable situation in which the fragments may easily re-displace (collapse)
- The healing process is delayed
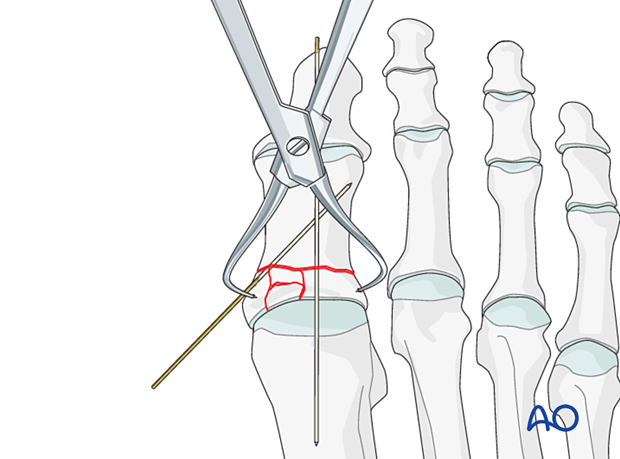
Reduction and temporary fixation of the articular block to the shaft
Reduce the articular block to the shaft and restore anatomical axial rotation, length, and angulation.
A periosteal elevator used as a lever may be helpful.
Alternatively, use a reduction forceps or a K-wire as a joystick as described above.
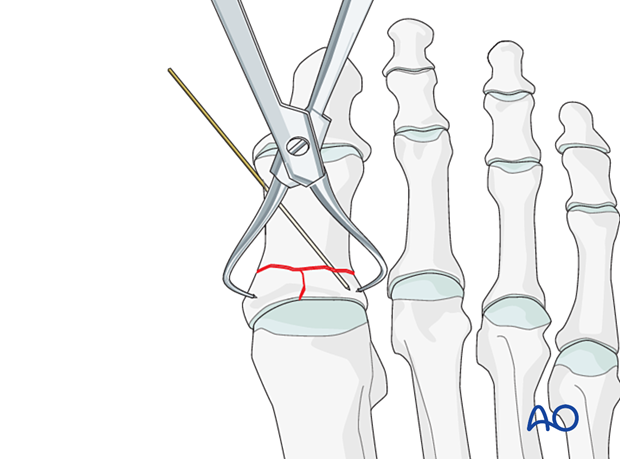
Use image intensification to confirm the reduction.
In length-stable fractures, a reduction forceps or a K-wire is used to secure the reduction.
Verify length, rotation, and angulation.
In comminuted fractures, a K-wire is inserted axially to maintain the reduction.
4. Fixation
Plate selection and contouring
Choose a T-plate of appropriate length, and contour the plate to fit the proximal hallux's medial aspect. The plate should be contoured to allow bony contact across the entire extraarticular fracture plane after screw tightening.
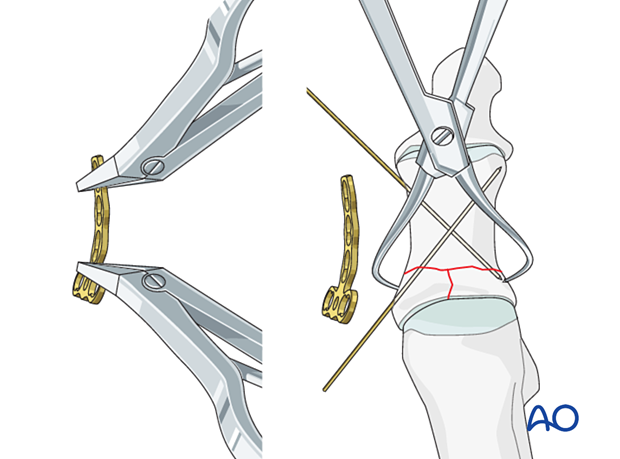
Fixation of the articular block
Fix the plate to the base of the hallux with two lag screws, which will compress and provide stability for the vertical intraarticular component.
Do not forget to overdrill the near cortex at the base to achieve the lag effect.
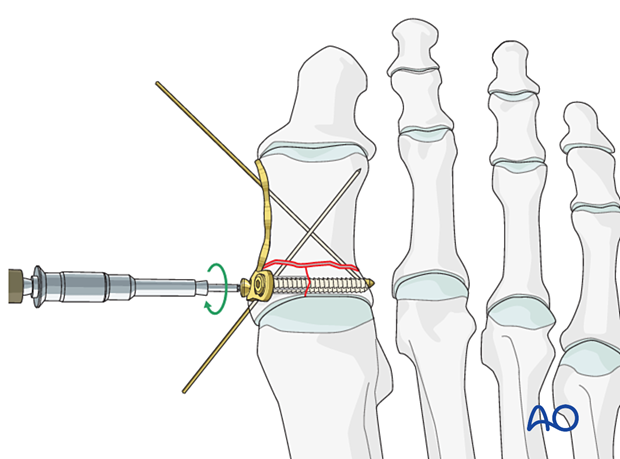
Fixation of the articular block to the shaft
Fix the articular block to the shaft by inserting two 2.0 mm or 2.4 mm screws in the shaft segment in neutral mode.
Ensure that there are no fracture gaps before screw insertion.
Remove the K-wires.
5. X-rays
Obtain x-rays to confirm length, rotation, and angulation, as well as hardware placement.
6. Aftercare
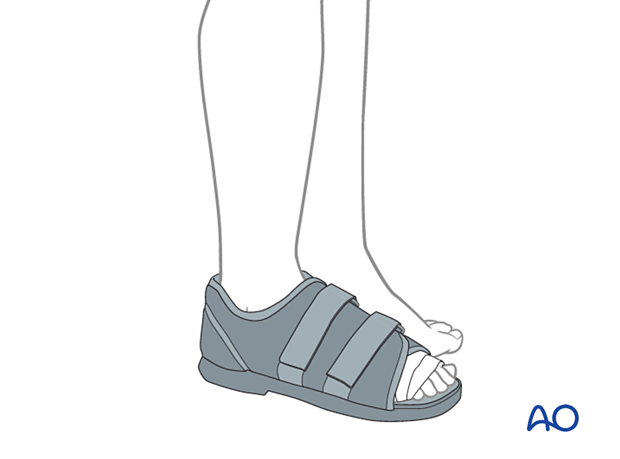
Weight-bearing may be allowed as long as the patient is provided with a flat, rigid sole shoe, which is continued for 6 weeks until X-rays or clinical examination is consistent with healing.
If the fracture construct does not involve transarticular fixation and is stable, range of motion exercises (both actively and passively) may be initiated once soft tissues permit.