ORIF - K-wires
1. Principles
Introduction
K-wires can be applied to many different fracture patterns. Considerations include fracture obliquity, comminution, and soft tissue status.
We will here illustrate two of many possible configurations.
As K-wires cannot compress the fracture, the fracture needs to be reduced before K-wire insertion. This is particularly true for articular fractures.
The preferred K-wire configuration would be extra-articular to prevent damage to the articular surface. Axially inserted wires that break may be difficult to retrieve.
Threaded K-wires are generally not preferred as they are more challenging to extract and potentially maintain fracture gaps.
Reduction of the proximal phalanx should be anatomic when possible.
The goal of an intramedullary wire would be to secure the fracture site in a soft-tissue-friendly manner while maintaining alignment.
K-wires should be sized appropriately to the bone. Typically wires thicker than 2.0 mm are not needed. The surgeon should be careful to cool the K-wire during insertion to reduce the risk of thermal necrosis.
Toe fractures versus long bone fractures
Toe fractures are different from long bone fractures.
- The bones are very small
- Fracture gaps are small
- Fixation devices don't need to counter large forces
Thus, following the AO principles is less critical than for long bones, and often isolated screws or K-wires alone will work satisfactorily.
Restoration of length, rotation, and angulation are important for cosmesis.
The hallux is particularly critical due to its importance for walking.
Timing of surgery
The timing of surgery is influenced by the soft tissue injury and the patient's physiologic status.
Dislocation or injuries associated with the skin at risk requires immediate intervention regardless of the amount of soft tissue swelling.
If possible, swelling should be significantly decreased before surgery, which can take up to two weeks in some instances.
Open fractures should be promptly irrigated and debrided, and treated with antibiotics. Definitive fracture fixation may not be possible during this setting.
Forefoot fractures do not contribute to physiologic instability. If there is no soft tissue at risk, urgent intervention is not required.
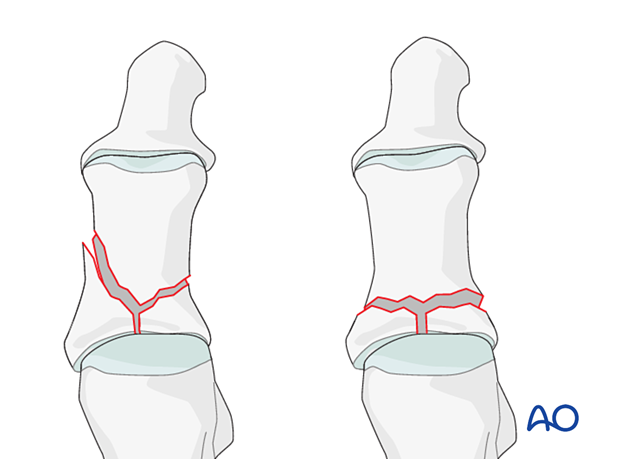
K-wire configurations
This fracture pattern is the most technically challenging to stabilize with K-wires alone due to the small bone size. First, the articular surface needs to be held together. Then the articular block needs to be attached to the diaphysis with a K-wire.
2. Patient preparation and approach
Patient preparation
This procedure is typically performed with the patient placed supine and the knee flexed 90°.

Approach
An open approach may be required to reduce the fracture and remove soft-tissue interposition.
Typically the medial approach to the hallux is used.
Consider inserting the K-wires outside the skin incision to prevent contamination.
3. Reduction and preliminary fixation of the articular block
Indirect reduction
Grasp the digit's terminus and use a combination of axial and angular traction to exaggerate the deformity.
Realign the toe and release the traction.

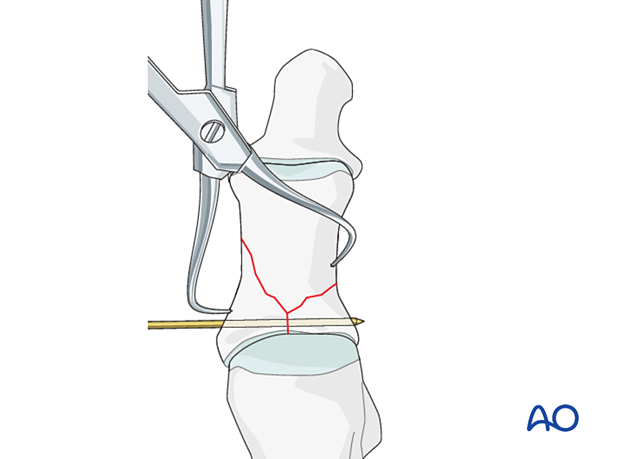
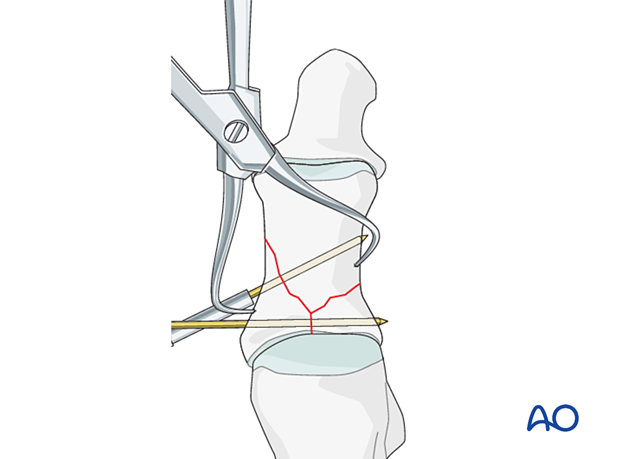
Direct reduction
DebridementWhen an anatomic reduction is desired, it is crucial to debride the hematoma and invaginated periosteum from the fracture site.
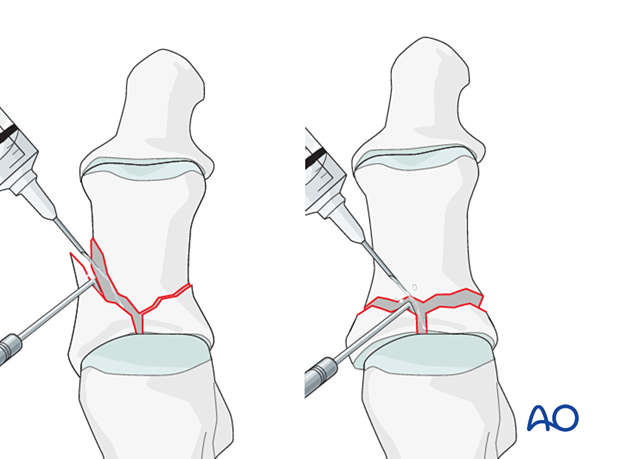
Restore the articular surface using small, pointed reduction forceps for larger fragments. Be careful not to apply excessive force as this can lead to fragmentation. If possible, apply the reduction clamp so that the forces created by the clamp are at right angles to the fracture line. This clamp placement helps in reducing the fracture and in applying compression.
Insert provisional K-wires to maintain the reduction of the articular block.
K-wires can be inserted into the fragment and used as a joystick.
Once reduction is accomplished, the wire may be advanced to secure the reduction.
Use image intensification to confirm the reduction.
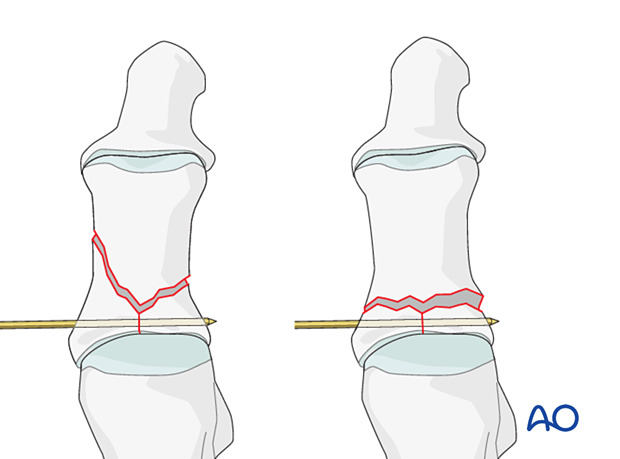
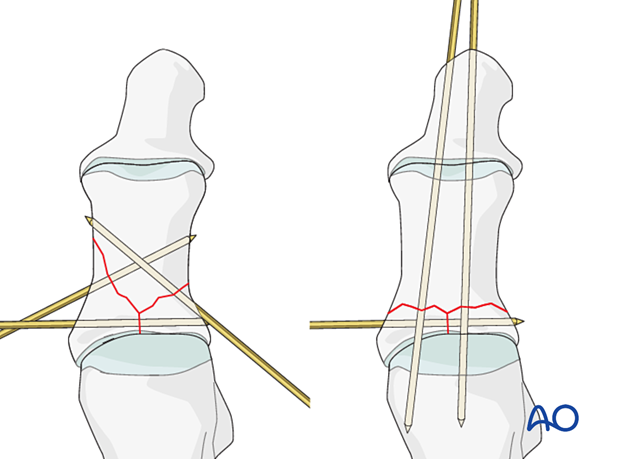
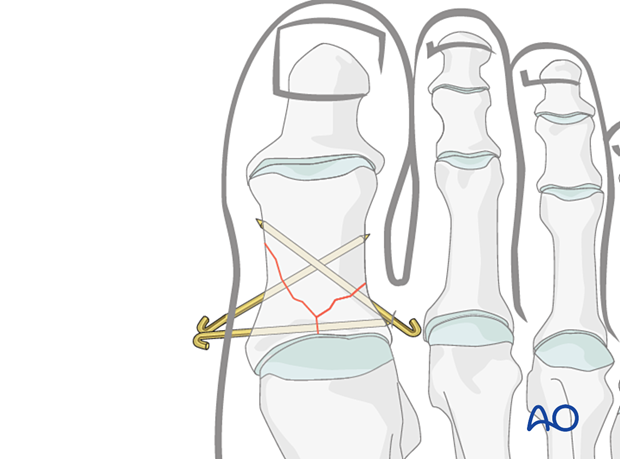
4. Reduction and fixation of the articular block to the shaft using non-axial K-wires
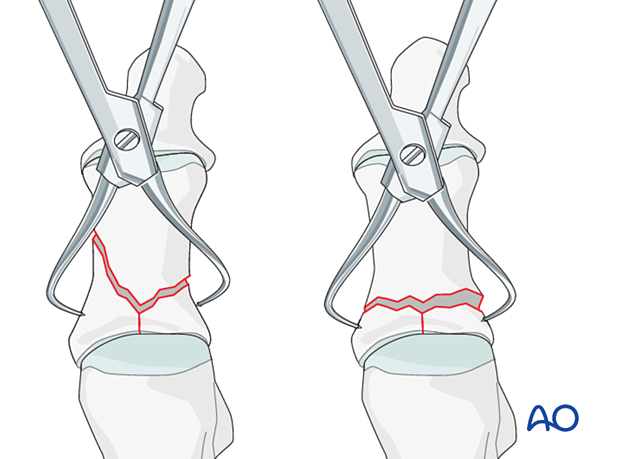
Reduction of the articular block to the shaft
Restore anatomical axial rotation, length, and angulation one or more of the below techniques:
- Closed manual reduction
- Use a K-wire as a joystick
- Use small reduction forceps
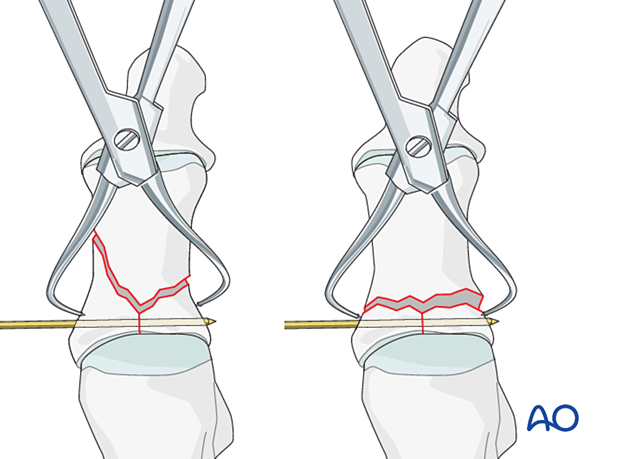
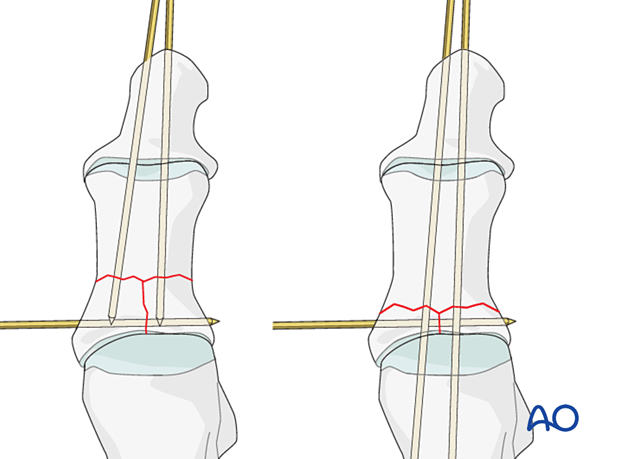
K-wire insertion
Insert K-wires to maintain the reduction of the articular block to the shaft.
Caution should be made to prevent thermal injury when inserting a K-wire in dense bone.
Intraoperative fluoroscopy is particularly useful to aid the correct position of the K-wire.
The stability of the reduction is assessed, and if needed, additional K-wires are inserted.
When satisfactory stability is achieved, cut the K-wires leaving adequate K-wire protruding through the skin to facilitate removal.
Assess the skin pin interface and release any excessive skin traction.
5. Reduction and fixation of the articular block to the shaft using axial K-wires
K-wire insertion
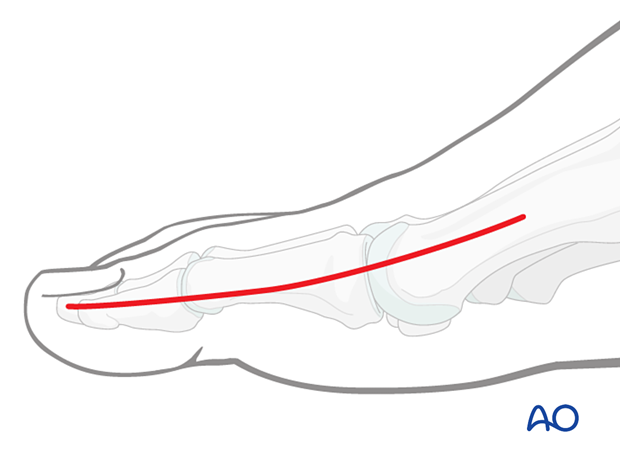
To avoid unnecessary radiation from image intensification, mark the K-wire's planned track with a skin marker on the distal phalanx in both the AP and the lateral aspects.

K-wire insertion into the distal phalanx
A 16 gauge hypodermic needle or a drill guide can be used to prevent the K-wire from slipping during insertion. Either instrument facilitates K-wire insertion along the longitudinal axis of the phalanx.
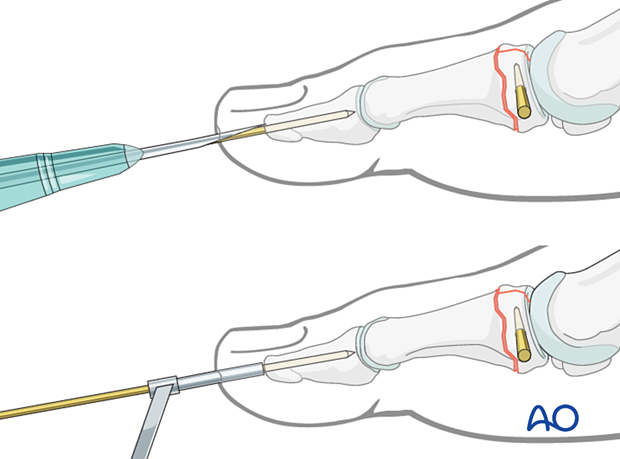
If a K-wire is mistakenly inserted at an angle to the phalanx axis, it is recommended to leave it in until a second K-wire has been inserted in the correct orientation. Leaving the first K-wire in place prevents the second wire from going unintentionally along the wrong track.
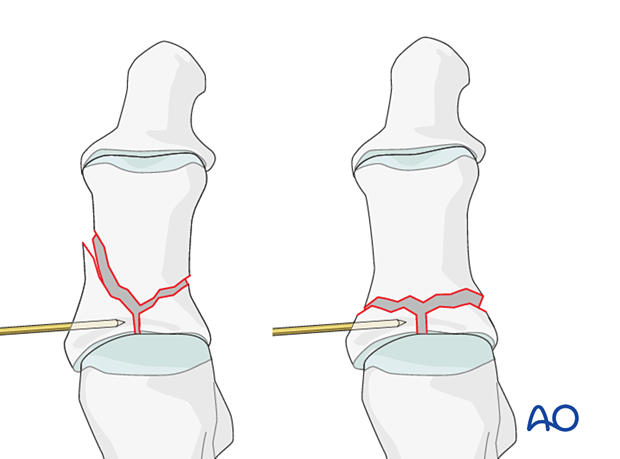
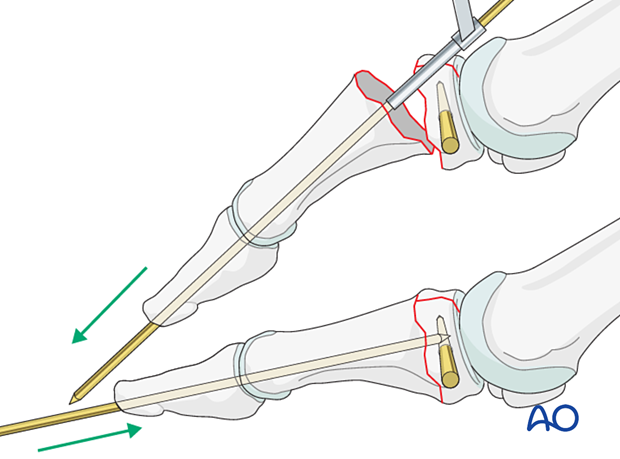
Fixation using axial K-wires as a joystick for reduction, and fixation
With a different fracture pattern, a different technique can be used to reduce and fix the articular block to the shaft.
Two axial K-wires are recommended once initial fixation is obtained.
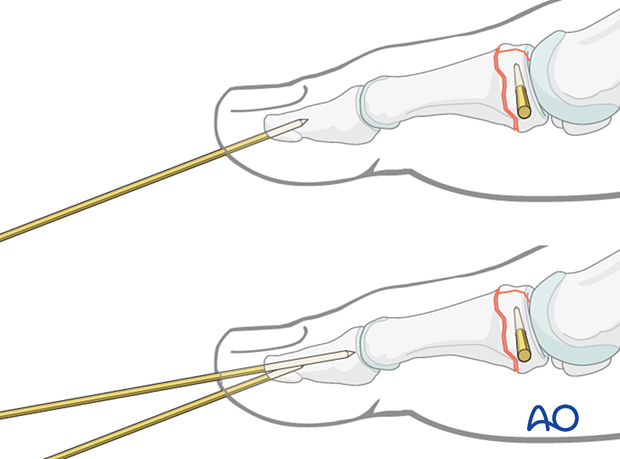
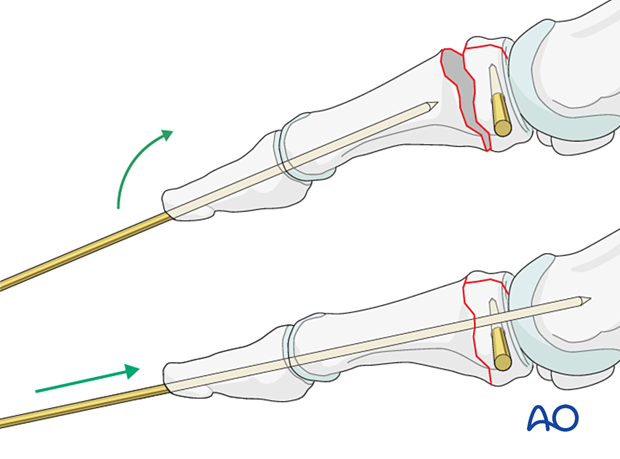
Advance the K-wire up to the fracture line but not across it. Use the K-wire as a joystick to reduce the fracture.
Once reduction is satisfactory, the wire can be advanced across the fracture plane and into the phalanx base or metatarsal head, depending on the size of the proximal segment.
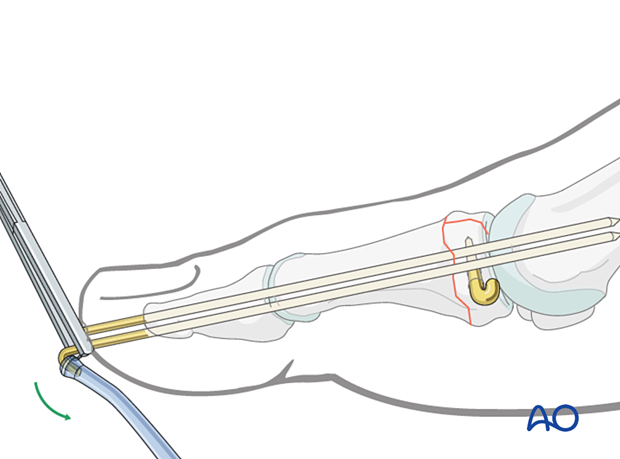
In open fractures, another option is to introduce a double-ended K-wire in a retrograde fashion with the inside-out technique.
Flex the distal fragment to gain an optimal view of the fracture surface. Insert the K-wire through a drill guide and advance it along the medullary canal and through the distal tip of the tuft, piercing the soft tissues until it exits the skin.
While leaving the drill guide in place for soft-tissue protection, pull on the K-wire's distal end until it is flush with the fracture surface.
Use the K-wire as a joystick to reduce the fracture, and advance it across the fracture up to the base of the fractured phalanx.
Insertion across the joint (if needed)
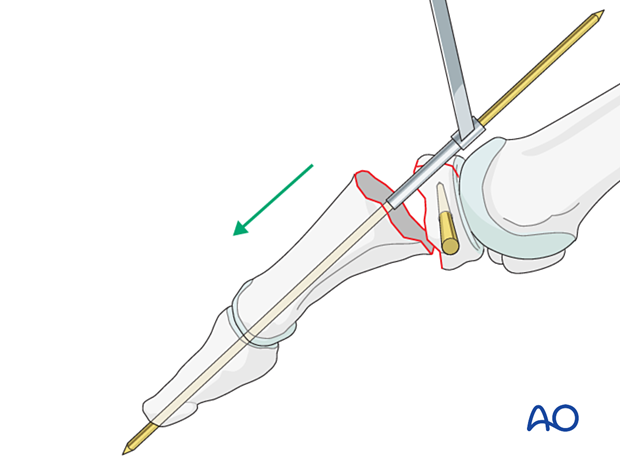
In proximal or multifragmentary fractures, advance the K-wire across the joint and into the phalanx base (or metatarsal) proximal to the injured phalanx. Be careful not to penetrate a second joint.
In more distal fractures, insertion of the K-wire across the joint may not be necessary.
A second axial K-wire should be inserted if there is space and it is possible.
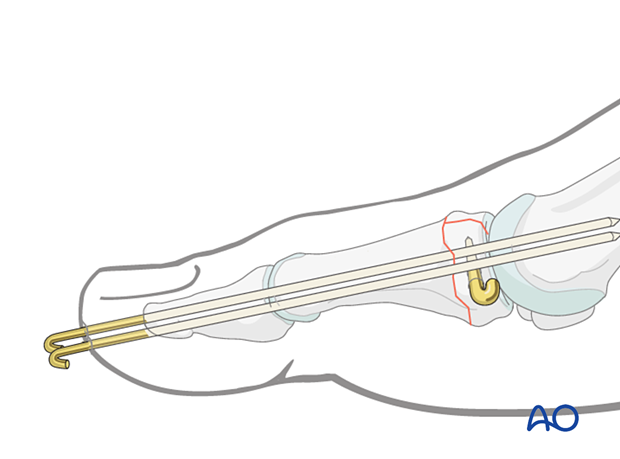
Cut the K-wires
Cut the K-wire so that it protrudes through the skin, about 1 cm from the tip of the toe.
With the wire placed in a finished position, clamp the portion of the wire nearest the skin with a Kocher.
Using a sucker tip that goes over the tip of the K-wire, the K-wire is bent 170°.
Leaving the K-wires to protrude through the skin in this way has the advantage of its being easy to remove. The disadvantages are patient discomfort and the risk of pin-track infection.
6. Aftercare
An appropriate well-padded dressing should be applied to protect the surgical incision.
The skin pin interface should be similarly well-padded but with dressings that can be readily removed to inspect for pin site infection.
Immediate postoperative treatment is rest, ice, and elevation.
The patient should be encouraged to begin early weight-bearing as permitted by the stability of the fracture. In general, patients can be weight-bearing as tolerated.
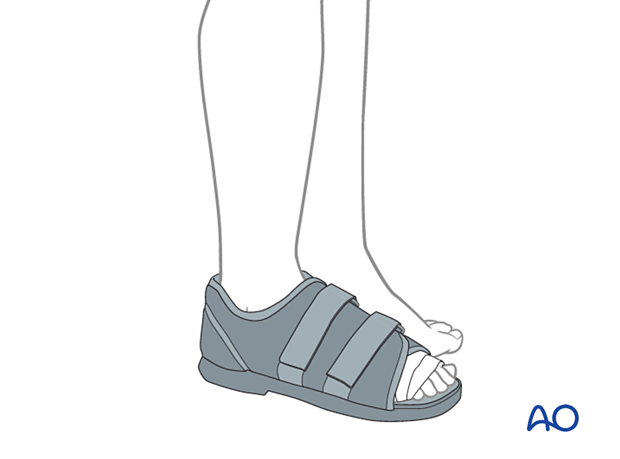
A stiff-soled shoe can be used to protect the surgical site.
Patients must exercise their ankle and subtalar joints to prevent stiffness (eg, by stretching their Achilles).
X-ray the toe at six weeks to confirm satisfactory union and remove K-wires if present. Once the fracture is united, the orthosis may be gradually discontinued.
7. Case
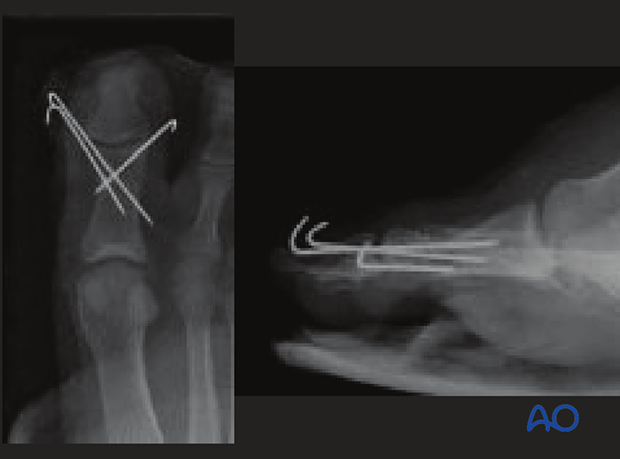
This case shows a multifragmentary complete articular fracture of the distal end of the proximal hallux, with significant displacement.
Due to the marked displacement, the clinical presentation shows a crooked toe, thus indicating surgery.
Although these are mostly open injuries, this was closed.

Lateral image showing dorsal displacement.
There was also a significant associated nail bed injury.
The AP and lateral images show a satisfactory closed reduction and multiple K-wires.