MIO - Bridge plate
1. General considerations
Principles
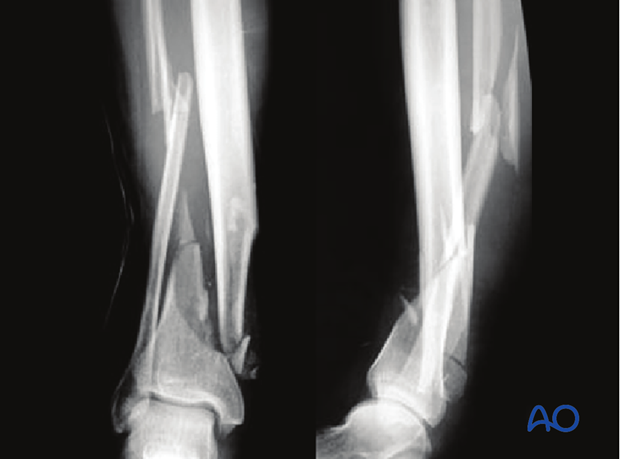
The soft-tissue conditions usually dictate the choice of procedure: early single-stage or multiple-stage surgery. When the soft tissue damage is minimal, acute single stage MIO stabilization is appropriate.
The associated shaft involvement requires a longer, stronger plate.
Displaced fractures with minimal, closed soft-tissue injury
(Tscherne classification, closed fracture grade 0, rarely grade 1)
These injuries may be reduced and fixed primarily, as a single stage procedure, if the soft tissues are in truly excellent condition.
A distractor or external fixator may help reduction. Fibular reduction and fixation is the usual next step, but this reduction must be accurate, so that it does not prevent tibial reduction. Finally, the tibial plate is introduced with MIO technique and final reduction of length, alignment and rotation is achieved.
Grossly displaced fractures and/or fractures with severe, closed soft-tissue injury
(Tscherne classification, closed fracture grade 2 or 3)
It is generally advisable to proceed in two or more stages:
- Closed reduction and joint bridging external fixation
- Definitive MIO reconstruction after 5-10 days (wait for the appearance of skin wrinkles)

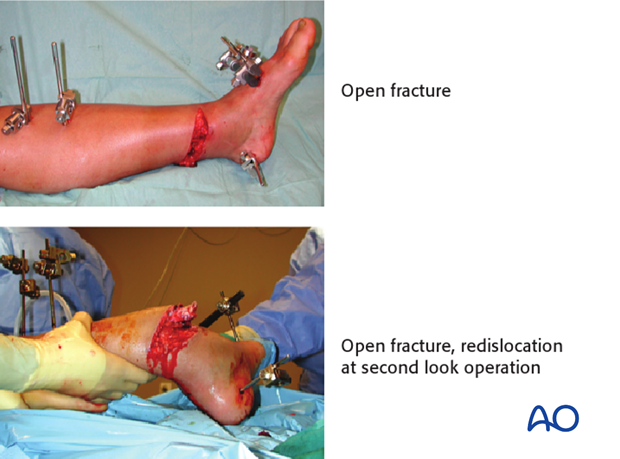
Open distal tibial fractures
These are very severe injuries which may require plastic surgery for soft-tissue reconstruction. The management includes several stages:
- Emergency management: Wound debridement and lavage. Joint-bridging external fixation and stabilization of the fibula (if needed and soft tissues allow). Where possible, closure or coverage of any opening into the joint should be achieved.
- After 48 hours: Soft-tissue coverage (local or free flap). Plan for definitive stabilization at this time.
- Definitive stabilization: Bridging of the metaphyseal comminution, with or without bone graft.
Bone grafting at the time of soft-tissue coverage is possible if the envelope is obviously viable but in marginal soft-tissue situations or in the multi-traumatized catabolic patient bone grafting as a secondary procedure may be advisable.
Teaching video
AO teaching video: Locking Compression Plate (LCP) Percutaneous Plate Fixation of the Tibia and Fibula in a Distal Multifragmentary Fracture of the Lower Leg (MIO Technique)
2. Fibula or tibia first? Sequence of bone stabilization
Introduction
If the fibula is fractured, it usually needs to be stabilized.
Simple fibular fractures
This fracture is usually addressed first with open anatomic reduction and plate fixation. Alternatively, for transverse fractures, consider a small diameter, flexible intramedullary nail. Fibular reduction helps realign the tibia fracture.
Multifragmentary fractures of the fibula
Some fibular fractures are complex, and reduction may be difficult. Any malreduction of the fibula will impede anatomic reconstruction of the tibia. In this situation, fibular ORIF is better performed after the tibia has been fixed. The syndesmotic ligaments are usually intact, so gross realignment of the fibula occurs with reduction and fixation of the tibia. For comminuted fibular fractures a MIO technique with a long bridging plate, or intramedullary fixation of the fibula with a small diameter, flexible nail is easily achieved after tibial reduction and fixation. Fibular nailing is particularly applicable if the soft-tissue injury or complexity of the fracture makes extensive exposure for internal fixation hazardous.
3. Preoperative planning
Preoperative planning is an essential part of treatment of all distal tibial fractures. It consists of:
- Careful study of the x-rays and CT scan
- Drawing of both the fracture fragments and the desired end result (often indicated by a reversed tracing of the intact opposite tibia)
- Consideration of intraoperative reduction techniques
- Choice of implants
Reduction can be achieved by ligamentotaxis alone with indirect manipulation. Direct exposure is therefore not often necessary. The shape of the implant serves as a reduction tool. A properly contoured plate applied according to a good preoperative plan improves your chances of a good reduction.
4. Patient preparation and approach
Patient preparation
This procedure is normally performed with the patient in a supine position for MIO.

Approach
For this procedure a minimally invasive approach is used.
5. Implant choice and plate preparation
Implant choice
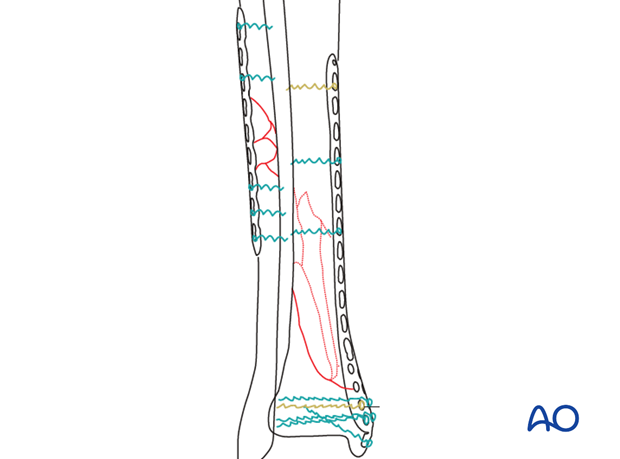
Because these fractures involve the tibial diaphysis, a longer and stronger plate is usually necessary. A variety of precontoured distal tibial plates are available.
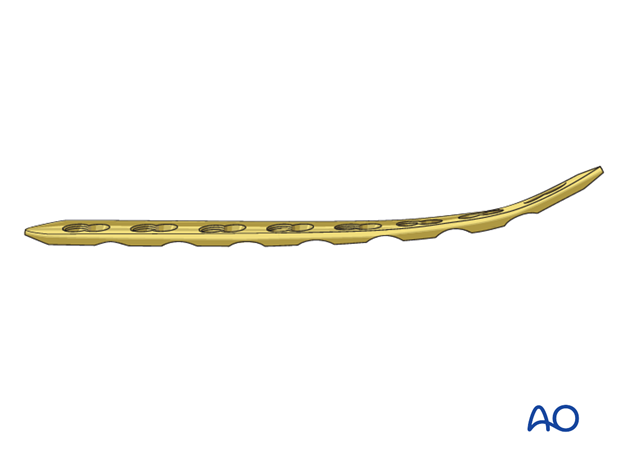
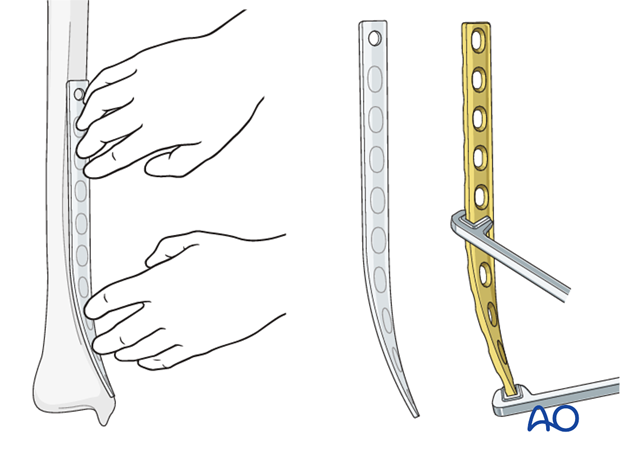
Plate contouring
If a precontoured implant is not available, or is insufficient for the fracture proximally, it will be necessary to precontour a standard (4.5 or 3.5 mm) plate prior to insertion. With MIO plate constructs it is preferable to choose an implant as long as possible for the widest distribution of load at the fracture site. Choose a plate that allows enough screws to be placed in the distal fragment. A non-contoured plate can be shaped prior to sterilization, using a sawbones model as a template. First, determine the length of the plate from preoperative x-rays.
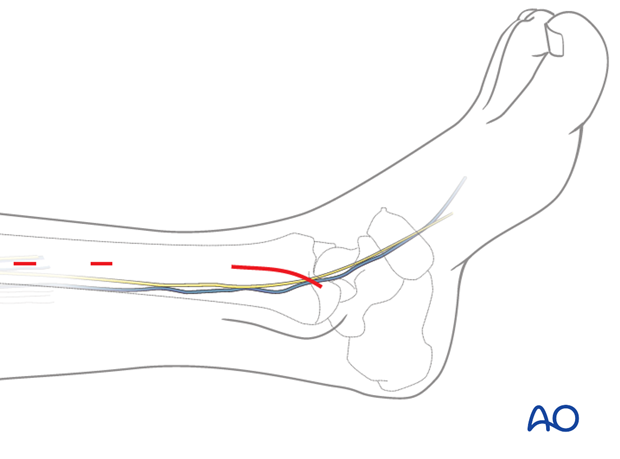
The most distal 8-12 cm of the plate must be bent to form a concave arc with a radius of curvature of about 20 cm and twisted to fit the distal tibia. As illustrated, the medial tibia is internally rotated distally (20 degrees) and lies closer to the sagittal plane.
6. Preliminary reduction
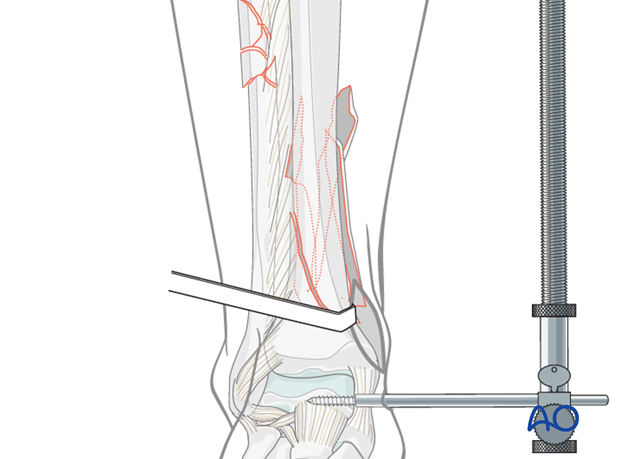
Indirect reduction with a distractor
An appropriately positioned large distractor or external fixator is a very helpful tool for reduction.
Medial positioning allows subcutaneous access to the tibia. A laterally based distractor requires a pin through the anterior muscular compartment but provides more efficient distraction of any associated fibular fracture, and correction of valgus deformities. Distraction can be used for the open reduction and plate fixation of the fibula as first step (in case of simple fracture pattern of the fibula) and for the reduction of the tibia.
Schanz screws are positioned in safe zones of the tibial shaft and talar neck (or the calcaneal tuberosity). In case of previously applied joint-bridging fixator, the already existing Schanz screws can be used.
Final reduction depends upon bringing the proximal and distal tibial segments into proper position against a correctly contoured plate. Non-locked screws or push-pull reduction devices can be used to approximate the bone to the plate.
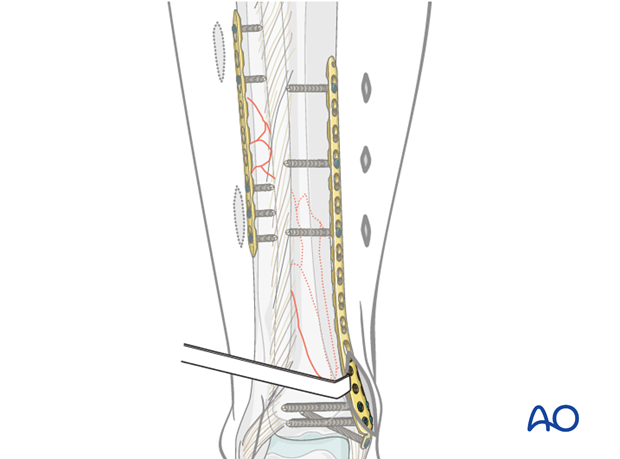
7. Plate insertion
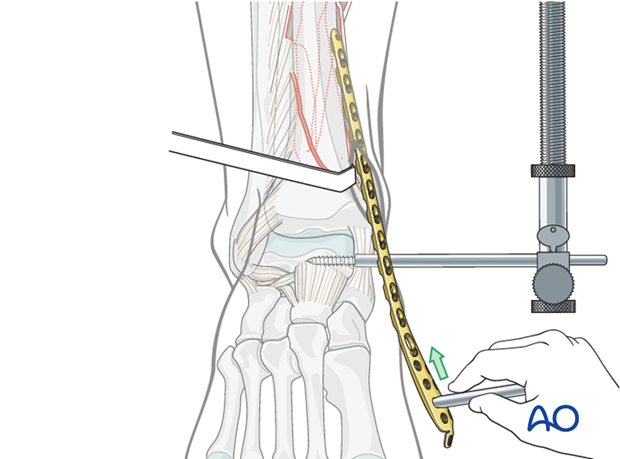
The plate is inserted after proximal tunneling with a blunt instrument.
Depending on the fracture situation, the plate is usually positioned on the anteromedial aspect of the tibia.
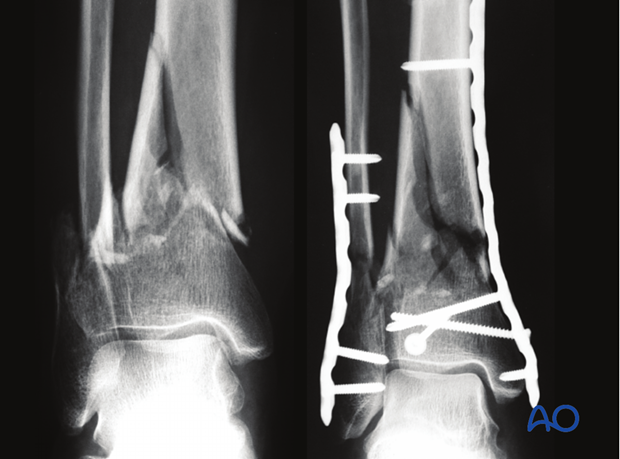
8. Plate fixation
Preliminary plate stabilization
Temporary fixation can be performed with K-wires through the screw holes (or inserted drill sleeves) to check the final plate position before the first screw is inserted.
Once accurate restoration of length, alignment and rotation have been achieved, provisional stabilization of the plate can be performed with a single conventional “positioning” screw inserted through the plate. If this is achieved with the most proximal screw, it is advisable to formally expose the proximal end of the plate.
Reduction is finalized by pulling the distal segment against the plate with a non-locking screw or other instrument (e.g., push-pull device).
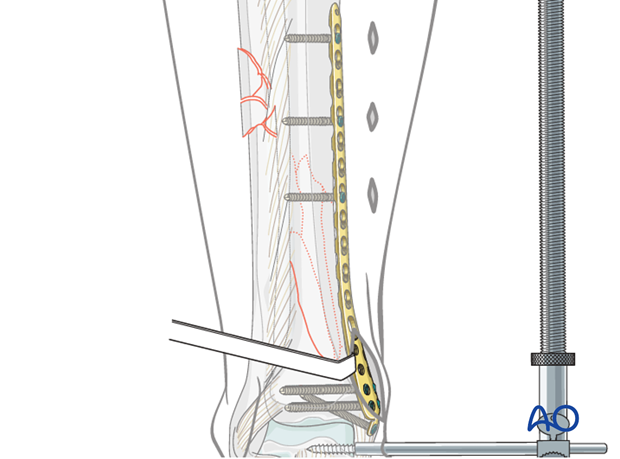
Screw insertion
Further proximal and distal screw insertion is completed.
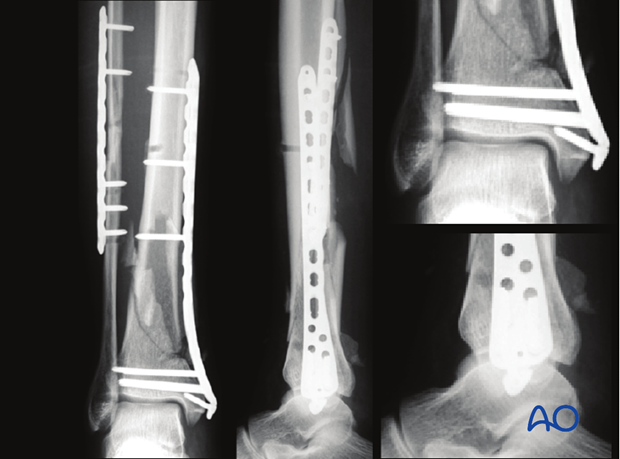
The number and position of the screws inserted is dependent on the individual fracture pattern and bone quality. Ideally the concept of “balanced” fixation should try to be achieved. Usually, the metaphysis requires more screws (3-5) than the diaphysis (2-3). In osteoporotic bone, the number of screws must be increased on both sides of the fracture.
Locking head screws (LHS) may improve fixation in osteoporotic bone and short periarticular segments. Non-locking screws may be used first to reduce the fracture against the plate. They may be sufficient for definitive fixation in the diaphysis.
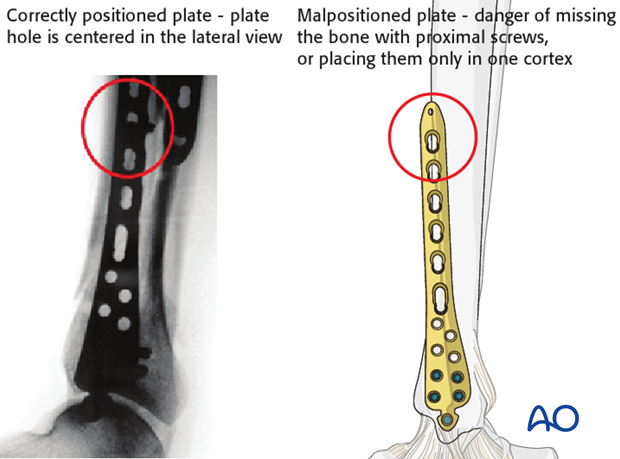
Pitfall - Malpositioning of the plate
If the plate is not positioned correctly, there is a danger of missing the bone with proximal screws or placing them only in one cortex.
Bone grafting
Bone grafting is almost never required, except in open type A fractures with bone loss. In such cases, it should be delayed until the soft-tissue envelope is stable.
9. Plating of the fibula
In most extraarticular multifragmentary fractures, the fibula is fractured as well and needs to be stabilized. Simple fractures are plated in an open technique as first step of the procedure. Complex fractures of the fibula are better addressed after stabilization of the tibia. An appropriately sized plate, often a 3.5 standard or locking compression plate (LCP) should be used. Lower profile, weaker plates (e.g., one-third tubular plates) may be enough for some fractures.
In compromised soft tissues, a minimally invasive plate osteosynthesis (MIO) can be used also for the fibula. Two short incisions at the level of both plate ends are sufficient to insert the plate from distal to proximal and also to insert 2-3 screws in each main fragment.
10. Final assessment
The x-ray imaging at the end of the operation confirms the anatomical restoration of length, alignment and rotation.
For further information see the content on assessment of reduction.
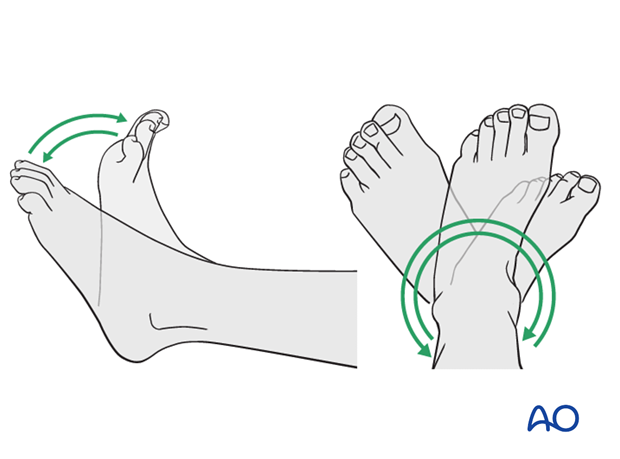
11. Aftercare following plating
Leg elevation is recommended for the first 2-5 postoperative days. Physiotherapy with active assisted exercises is started immediately after operation. Immobilization is not necessary.
Mobilization
Starts depending on the wound healing with flat footed, weight of the leg weight bearing (10-20kg).
Follow up
Clinical and radiological follow-up is recommended after 2, 6 and 12 weeks. Depending on the consolidation, weight bearing can be increased after 6-8 weeks with full weight bearing usually after 3 months. Supervised rehabilitation with intermittent clinical and radiographic follow-up is advisable every 6-12 weeks until recovery reaches a plateau, typically 6-12 months after injury. Weight-bearing radiographs are preferable to assess articular cartilage thickness. Angular stable fixation may obscure signs of non-union for many months.
Implant removal
Implant removal may be necessary in cases of soft-tissue irritation by the implant (plate and/or isolated screws). The best time for implant removal is after complete remodeling, usually at least 12 months after surgery.