ORIF - Plate and screws through anterolateral approach
1. Single-stage or multiple-stage surgery?
Principles
The choice of an early single-stage versus a multiple-stage surgical approach is based on the individual situation. In general, a staged protocol is used for the majority of high-energy pilon fractures.
Displaced fractures with minimal, closed soft-tissue injury
(Tscherne classification, closed fracture grade 0, rarely grade 1)
When soft-tissue condition is optimal, reconstruction may be achieved by a single-stage open procedure, embracing the classical four steps of Rüedi and Allgöwer:
- Reconstruction of a fractured fibula
- Reconstruction of the tibial joint surface
- Use of autogenous cancellous or corticocancellous bone graft (if necessary)
- Support by a buttress plate
Significantly displaced fractures and/or fractures with severe, closed soft-tissue injury
(Tscherne classification, closed fracture grade 2 or 3)
It is generally advisable to proceed in two or more stages:
First stage:
- Closed reduction
- Fibular reduction and stabilization: Accurate reduction and stabilization of the fibula re-establishes its proper length, alignment and rotation. This assists with proper positioning of the posterolateral tibial articular fragment (from the attachment of the posterior tibiofibular ligaments) and, in turn, with reduction of the talus relative to the tibial shaft. With complex fibular fractures, it may be better not to fix the fibula in the first stage.
- Joint bridging external fixation: It should be remote from the fracture. External fixation pins should avoid the planned future surgical approaches including the neck of the talus.
Second stage:
- Definitive open reconstruction after 5-21 days: It should be delayed until the soft tissues have recovered sufficiently to allow definitive reconstruction. Return of skin wrinkles is a good sign of soft-tissue recovery.

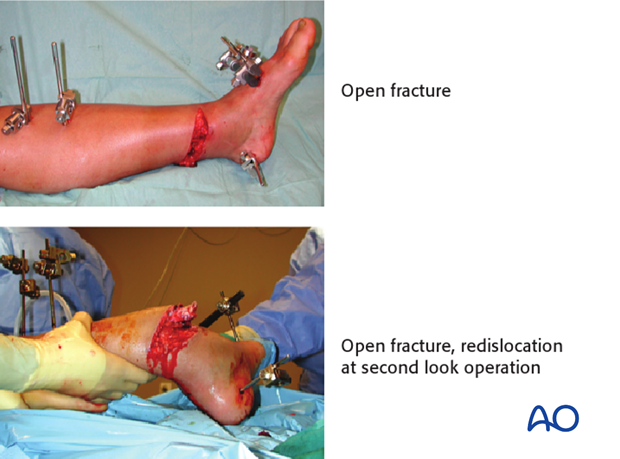
Open pilon fractures
Open pilon fractures are often very severe injuries that may require plastic surgery for soft-tissue reconstruction. The management includes several stages:
Emergency management:
- Wound debridement and lavage
- Fibular stabilization and fixation (if needed and the soft tissues allow)
- Joint-bridging external fixation.
Second stage (within 48 - 72 hours):
- Soft-tissue coverage (local or free flap)
- Reconstruction of the tibial articular surface may be possible at the same time and should be considered if the exposure for flap coverage allows.
Third stage:
Definitive stabilization between the articular segment (joint block) and tibial shaft by internal fixation (or external fixator) is typically delayed until soft-tissue recovery has occurred. However, this may be performed at the time of flap coverage in certain circumstances.
2. Planning for reduction and fixation
General considerations
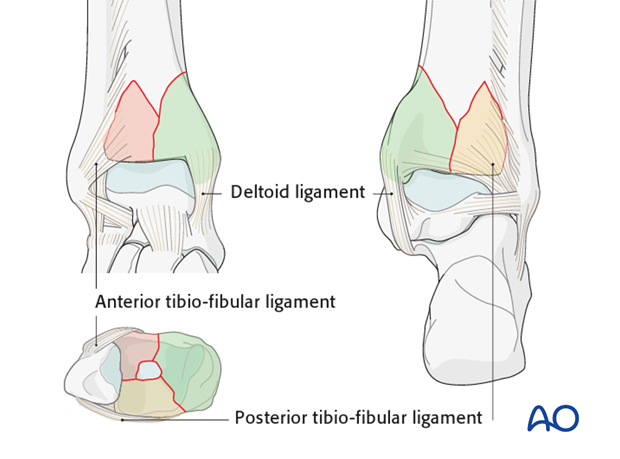
Multifragmentary articular fractures typically involve three major fragments: posterolateral, anterolateral, and medial. Additionally, there can be a central articular fragment. Ligamentous attachments are usually intact. They are the posterior tibiofibular ligament (posterolateral fragment), the anterior tibiofibular ligament (anterolateral fragment), and the deltoid ligament (medial fragment).
The fibula anatomical reduction is essential if posterolateral and anterolateral tibial articular fragments are to be reducible. Fibular malreduction is a pitfall, particularly during emergency fixation of multifragmentary fractures.
Choice of surgical approach
The choice of surgical approach is influenced by:
- Integrity and condition of the soft tissue envelope
- Fracture characteristics
- Available implants
Most tibial pilon fractures are best approached anteriorly. The optimal approach side can be determined according to:
- Size of the anterolateral fragment: when it is large, and its medial fracture plane is at or near the medial malleolus, an anteromedial approach is recommended. When the anterolateral fragment is smaller, and the fracture crosses the articular margin more laterally, its reduction can be achieved with an anterolateral approach
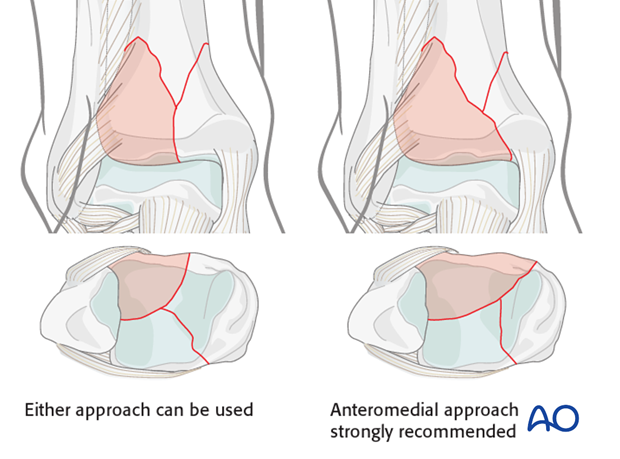
- Associated transverse traumatic wound at the distal tibia (see fig.): the surgical approach should be performed on the opposite side to minimize additional dissection beneath the traumatized skin
The anticipated incision(s) for ORIF should be considered during initial debridement and external fixation, even though definitive fixation is delayed until soft tissues recover.

Injury radiographic evaluation and its influence on approach and implants
The choice of implants is dependent on:
- The surgical approach
- The soft tissue envelope
- The associated metaphyseal comminution assessed on the injury radiographs
- Presence of impaction: direct access to the impacted area must be provided
With bending fractures, comminution occurs on the side that fails in compression. Tension failure typically produces a simple transverse fracture plain.
For pilon fractures with a varus deformity, medial metaphyseal comminution is commonly observed and medial buttress plating with a stronger medial implant is necessary. An anteromedial approach is preferable for its application.
For pilon fractures with a valgus deformity, lateral metaphyseal comminution is commonly observed, and the medial distal tibia typically fails in tension. In these patterns, lateral or anterolateral buttressing is optimal and medial fixation can be less strong.
Thus, for a pilon with significant initial valgus and lateral and/or anterolateral metaphyseal comminution, an anterolateral approach permits optimal placement of a buttress plate.
The use of locking plates
The choice of whether to use a locking implant is determined by:
- Expected healing time
- Surgical approach
- Need for additional compression at the articular surface at the time of reduction
- Plate positioning: locking implants are unnecessary if plates are placed anterolaterally and medially.
- Fracture comminution may indicate the need for supplementary plate fixation
- Associated soft-tissue envelope that may contraindicates the use of supplementary plate fixation. In this case the use of an angular stable (locking) implant may help prevent late deformity and should be considered
- Bone quality: use of locking plates may improve stabilization of osteoporotic fractures
3. Articular comminution and impaction
There are multiple commonly observed articular injuries that increase the complexity of multifragmentary metaphyseal fractures. These include the presence of articular comminution and impaction. Impaction is frequently seen centrally and medially.
Articular surface impaction is important to be identified and corrected.
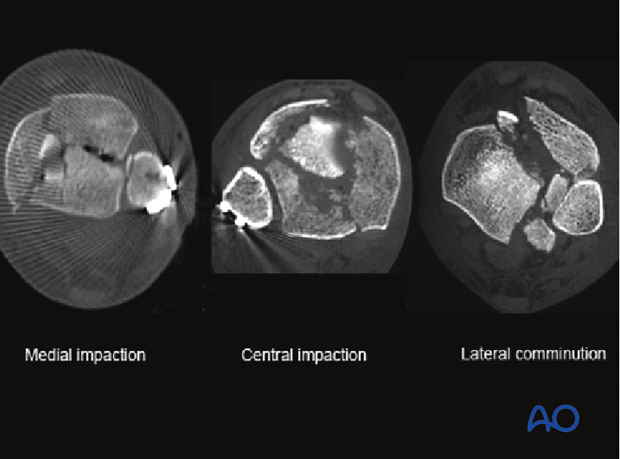
Medial comminution and impaction
Medial comminution and impaction is frequently seen in pilon fractures with a predominant varus deformity. The two typical locations are at the lateral aspect of the medial malleolus and at the medial aspect of the anterolateral fragment.
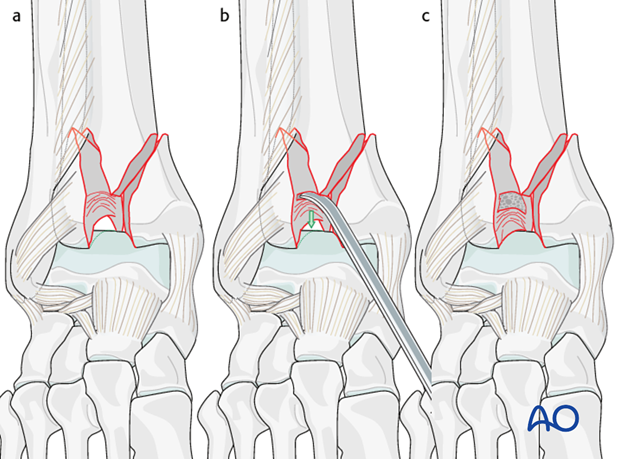
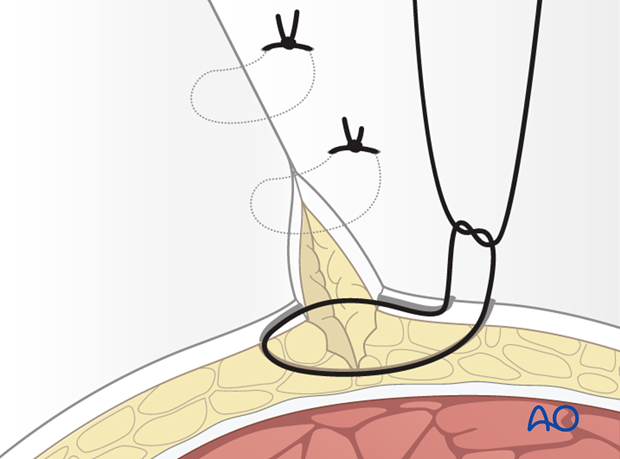
Medial articular comminution is optimally visualized through an anteromedial approach. In addition to reduction of the associated comminution of the medial malleolus, this approach allows for reduction of the impaction seen at the medial aspect of the anterolateral fragment. An osteotome or elevator can be used to disimpact the articular surface and bone graft can be placed above the articular surface.
The illustration shows an impacted area of articular surface on the anterolateral fragment (a), its reduction against the talus with an elevator (b), and after bone graft placement (c).
Lateral comminution and impaction
Lateral comminution and impaction is frequently seen in pilon fractures with a predominant valgus deformity. Lateral articular comminution can be approached through either an anteromedial or anterolateral approach. Visualization may be optimal with an anterolateral approach that allows for external rotation of the anterolateral fragment and direct reduction of the associated comminution.
4. Patient preparation and approach
Patient preparation
This procedure is normally performed with the patient in a supine position.

Approach
For this procedure an anterolateral approach is used.
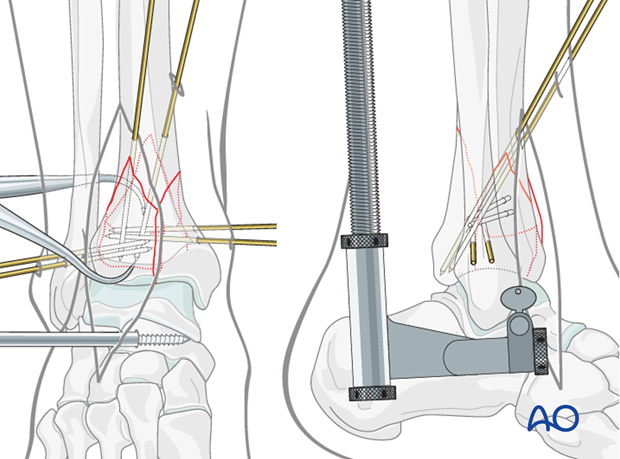
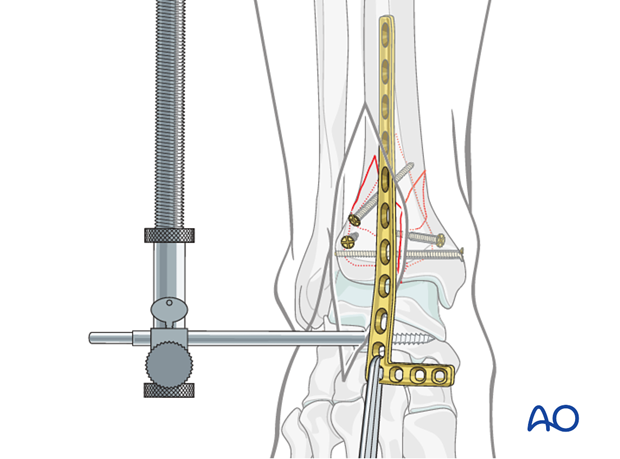
5. Application of a distractor
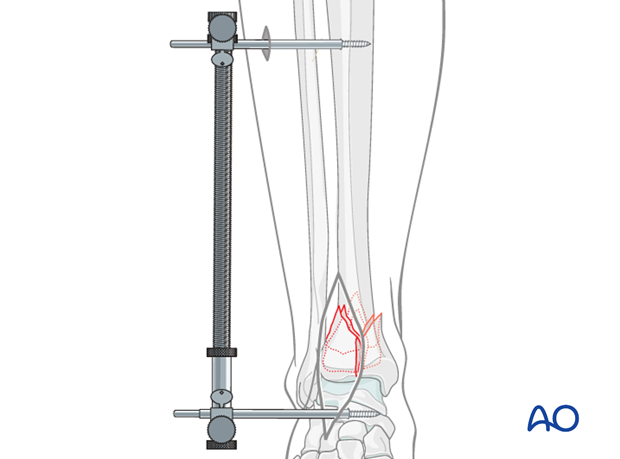
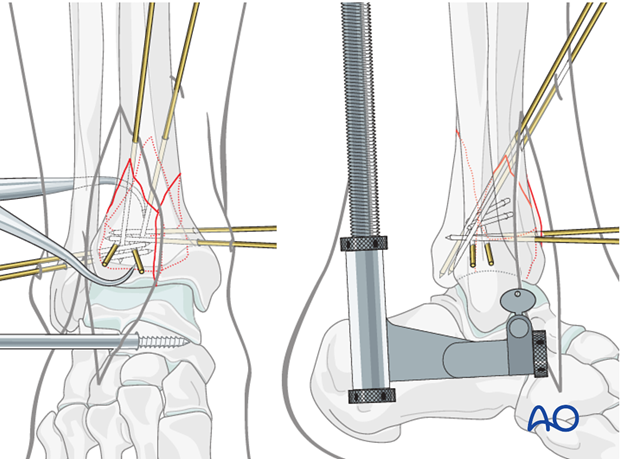
Application of a distractor intraoperatively greatly assists with articular visualization and alignment of several of the major articular fragments. A temporary joint bridging external fixator is typically replaced with a distractor during definitive articular surface reduction and fixation.
To apply the distractor laterally, a 4 mm Schanz pin is placed transversely from lateral to medial into the talar neck, through the surgical incision. A second 4 mm Schanz pin is placed from lateral to medial into the tibial shaft, proximal to the intended plate. The distal pin, anterior to the axis of rotation of the talus, produces ankle joint distraction and plantarflexion, maximizing articular visualization. The threaded rod of the distractor is placed posterolaterally, away from the incision.
Note: The course of the anterior compartment neurovascular bundle, and also the superficial peroneal nerve, should be considered during pin placement. The proximal pin should be placed in the anterior half of the tibia. It is important to use blunt dissection and the appropriate soft-tissue protection sleeves during pin placement.
6. Reduction of major articular fragments
Cleaning of the fracture site
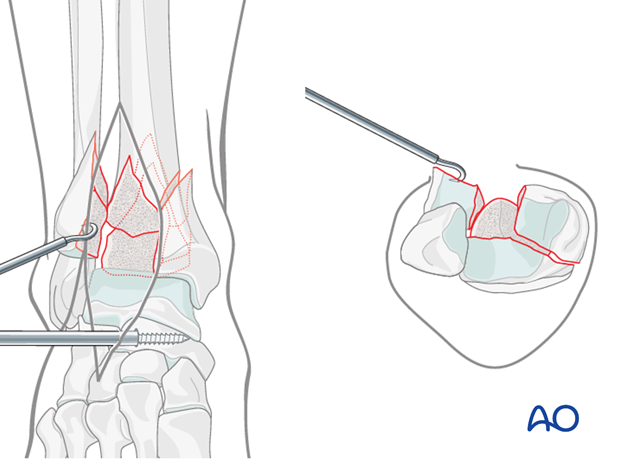
The anterolateral fragment is rotated externally on the anterior tibiofibular ligamentous hinge to allow visualization of the remaining articular segments.
The fracture is cleaned of early callus and hematoma.
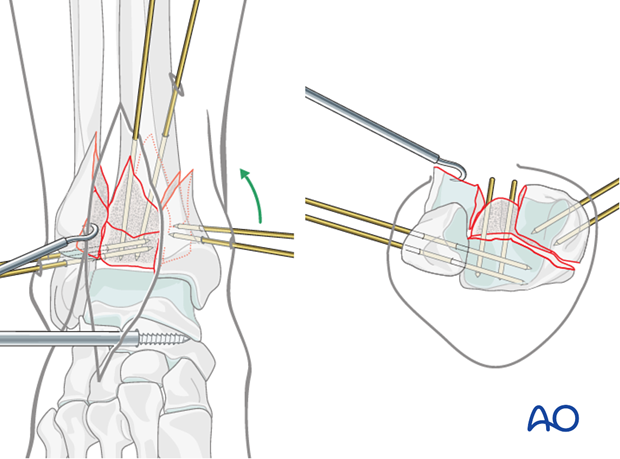
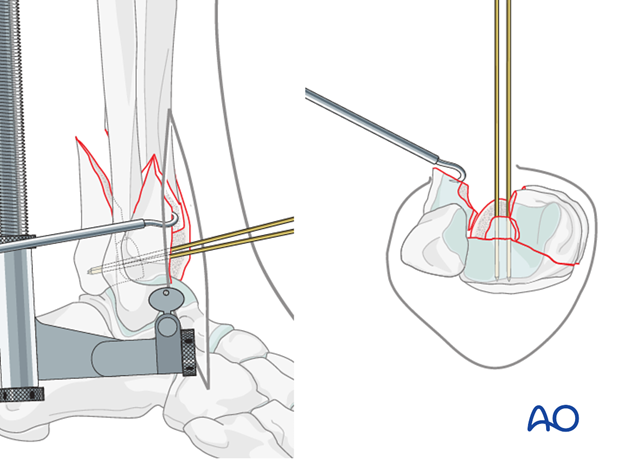
Derotation and preliminary fixation of the posterolateral fragment
The commonly observed dorsiflexion deformity of the posterolateral fragment must first be corrected.
Two small (2.5 mm) threaded pins or two K-wires are placed directly into the exposed anterior cancellous surface of the posterolateral fragment and used as joysticks to correct the dorsiflexion and posterior translation of the posterolateral fragment.
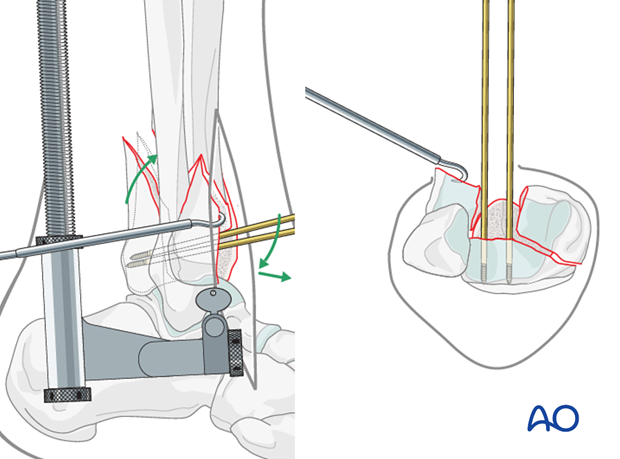
1.25 mm K-wires are placed to secure the posterolateral fragment. They can be placed from either the anterior tibia into the posterolateral segment, …
…or from the fibula into the posterolateral segment,…
…or both.
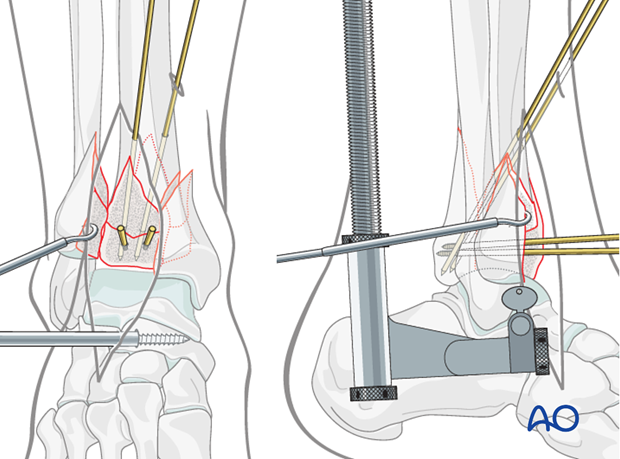
Reduction and preliminary fixation of the medial fragment
Two 1.25 mm K-wires are placed and used as joysticks into the medial fragment, to reduce it against the posterolateral fragment. In this step, the medial K-wires do not yet extend into the posterolateral fragment.
Alternatively, two small stab incisions can be used to place a large pointed Weber clamp from the posterolateral fragment to the medial fragment. The posterolateral fragment is engaged just above the ankle joint, between peroneal tendons and the Achilles tendon.
Note: To engage the posterolateral fragment, a small incision is placed at the posterolateral border of the fibula. Dissection continues between the fibula and the peroneal tendons to allow access to the posterior tibia.
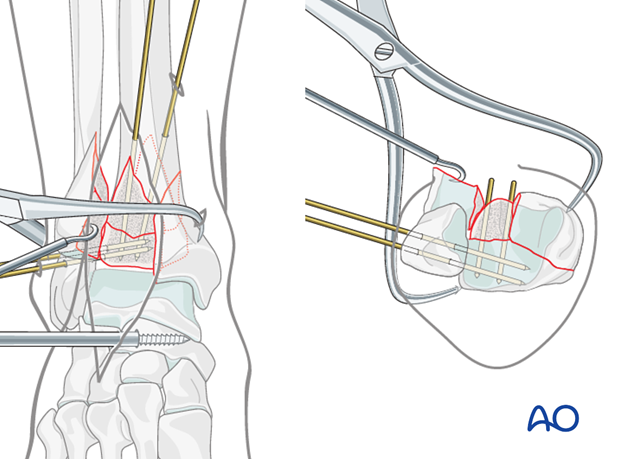
The medial and posterolateral fragments are stabilized with 1.25 mm K-wires inserted percutaneously, through the medial fragment and into the posterolateral fragment. These may be the K-wires used for fracture reduction that have been advanced. Wires placement should not interfere with the more anterior reductions.
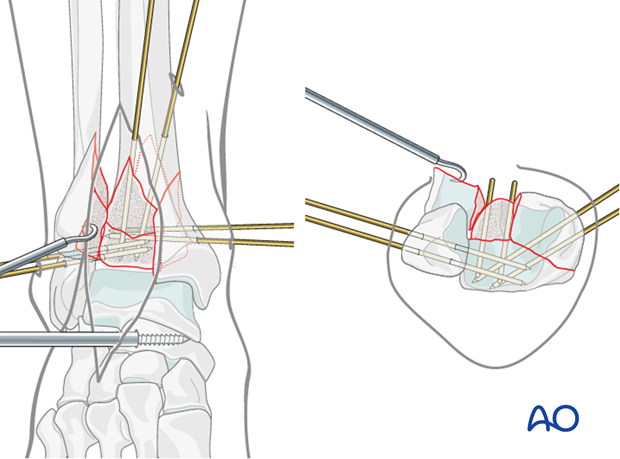
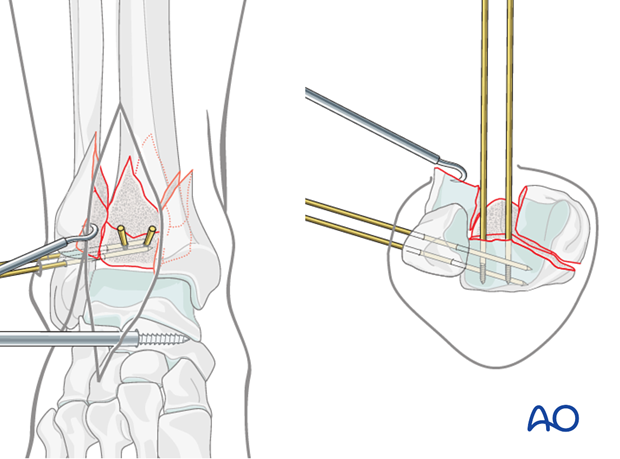
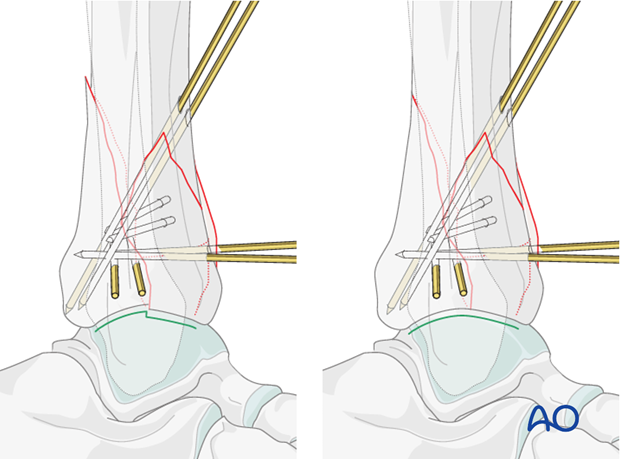
Reduction and preliminary fixation of the anterolateral fragment
The anterolateral fragment is rotated internally to complete the reduction of the pilon. This can be accomplished with dental picks and a large Weber clamp, placed from the posterolateral fragment to the anterolateral fragment.
The anterolateral fragment reduction can be confirmed cortically at the junctions with the medial fragment and the intact tibia. The reduction is confirmed at the articular surface using direct visualization.
The reduction is stabilized with additional 1.25 mm K-wires placed from the anterolateral fragment into the posterolateral segment.
These wires will add additional stability to the centrally impacted segment when present.
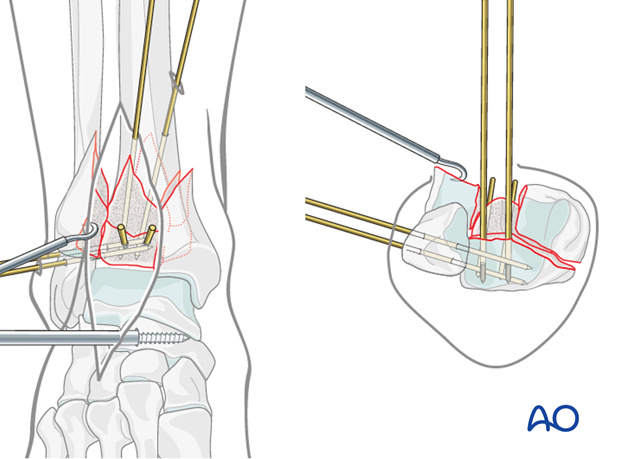
7. Reduction of central articular fragment
When present, the centrally impacted segment can either be reduced to the posterolateral fragment prior to its reduction, or to the combined and reduced posterolateral and medial fragments.
For the former reduction sequence, the centrally impacted segment is temporarily stabilized to the posterolateral fragment with two small K-wires. If a large defect exists in the metaphysis above the centrally impacted segment, a bone graft can be placed following confirmation of an accurate reduction.
To allow the reduction to be completed, fixation of the central impacted segment must be out of the way of additional articular fragments. K-wires can be inserted from the periphery of the distal tibia or cut short at the fracture surface.
Articular surface reduction
Initial attempts at reduction of the articular surface are often unsuccessful. Careful assessment is necessary. Malreduction must be corrected prior to definitive fixation.
Revision requires re-displacement of the anterolateral fragment. Displacement of the posterolateral and medial segments, typically in the sagittal plane, may also require correction. This process is repeated over and over until the fracture is reduced. See also the content on assessment of reduction.
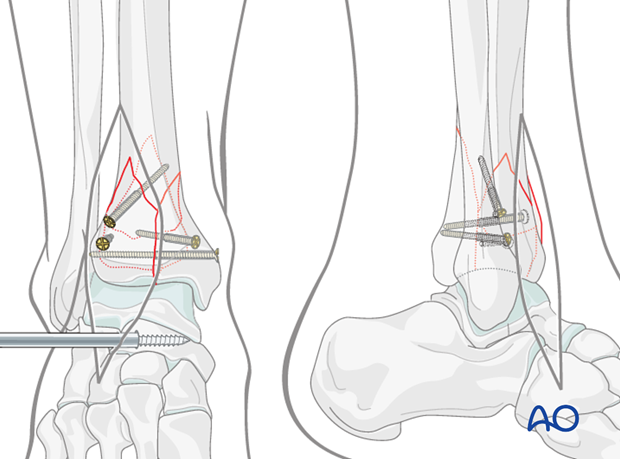
8. Lag screw fixation
Small lag screws can be placed between the major articular fragments. Small cruciate head 2.4 mm cortical screws may be advantageous as they do not interfere with the anticipated plate placement. Special extra-long screws will be necessary. The K-wires can be removed if stable compression of the articular fragments is obtained.
Alternatively, the K-wires can be left in place and the plate is applied.
9. Plate fixation
Introduction
In multifragmentary metaphyseal fractures, definitive internal fixation often includes lateral and medial plate fixation which span from the articular block to the tibial diaphysis. The distractor may need to be removed to allow plate placement. Additionally, plantarflexion of the foot is frequently necessary.
Options to consider include the number of plates as well as their stiffness, strength, and location. Comminuted areas and osteoporotic fractures may benefit from supplementary plates. If the fibula remains unstable, more stable tibial fixation may be advisable.
Choice of implant
The specific implant is less important than the reduction and the plate function. Non-locking buttressing implants can be used for the majority of pilon fractures. Angular stable fixation, using locking head screws, may avoid the need for a second plate and may reduce the need for bone grafting.
A precontoured L-shaped anterolateral plate (locking or not) may be the ideal implant for the anterolateral approach. If an anterolateral locking plate is used, an additional medial plate may not be necessary. However, if the anterolateral plate is no locking plate, an additional medial buttressing implant is often necessary.
Precontoured plates may often be used without adjustments. However, conventional straight plates must be contoured to fit the bone.
Application of the lateral plate
If lag screws are in place and reduction is stable, the distractor can be removed to facilitate plate insertion and placement. However, if the distractor is necessary to maintain length and alignment of the articular block, it may be advisable to leave the distractor in place.
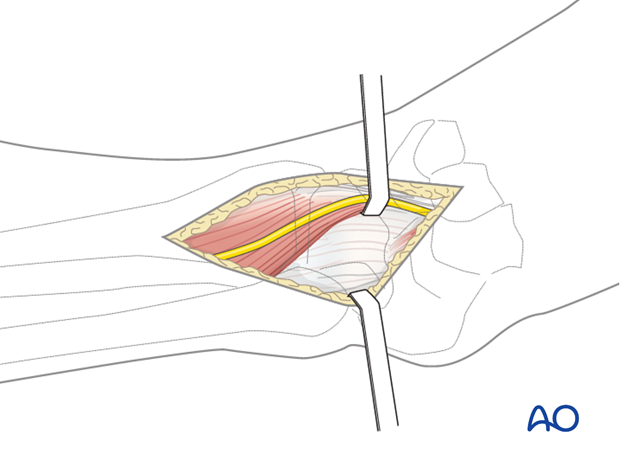
The plate is slid submuscularly along the lateral cortex of the tibia, deep to the anterior compartment musculature and neurovascular bundle, and anterior to the interosseous membrane.
Note: Care must be taken during plate placement to ensure that the plate is slid directly against the tibia to avoid damage to the neurovascular bundle.
Distal screw placement in lateral plate
Distal screws are placed from anterior to posterior engaging the major articular fragments. The lateral fluoroscopic image is used to ensure safe, extraarticular screw placements. The number and location of the distal screws is determined by the fracture pattern. Placed appropriately, they can help support central comminuted areas.
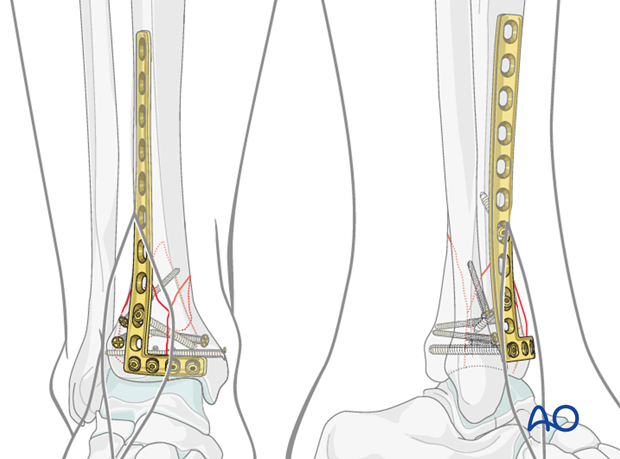
Proximal screw placement in lateral plate
Proximally a separate incision (4-6 cm in length) is placed 1 cm lateral to the tibial crest to allow plate adjustment and proximal screw placements.
Fixation of the medial side
Depending on the fracture configuration and location, medial fixation will consist of either
- Screws,
- Subcutaneous medial buttress plating,
- Or combinations thereof.
Note: The medial plate can be slid subcutaneously through a small (2 cm) incision. The screws through the plate can be inserted through small stab incisions. An additional long surgical exposure of the medial tibia should be avoided.
Wound closure
Prior to closure, reduction and stability must be reconfirmed (see also the content on assessment of reduction). The joint arthrotomy is repaired. It is imperative that the extensor retinaculum is also repaired to prevent bowstringing of the extensor tendons. The skin is closed with interrupted 3-0 nylon sutures placed in a modified Allgöwer-Donati fashion ( Dietz UA, Kuhfuss I, Debus ES, Thiede A. (2006) Mario Donati and the vertical mattress suture of the skin. World J Surg; 30(2):141-148).
.
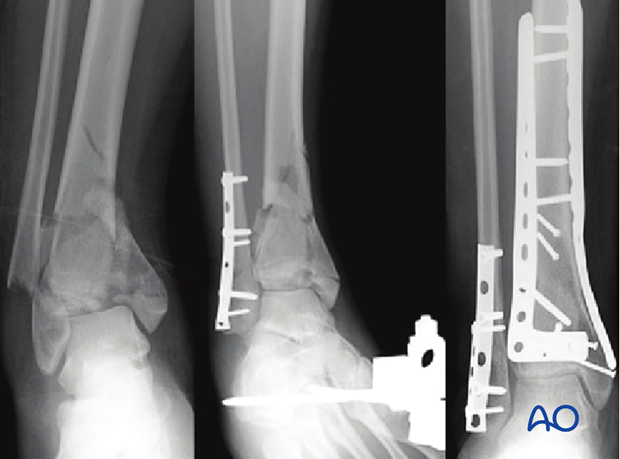
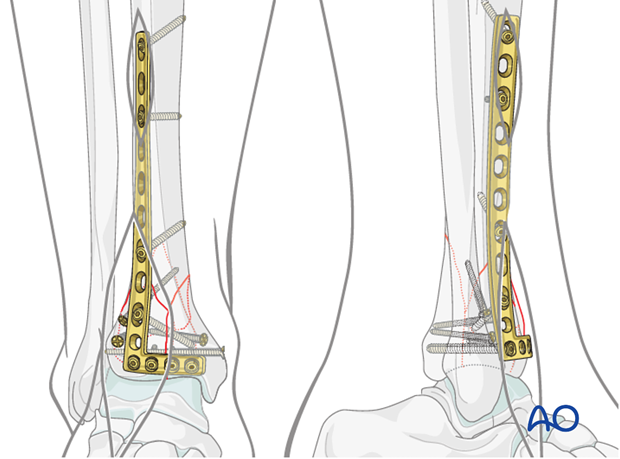
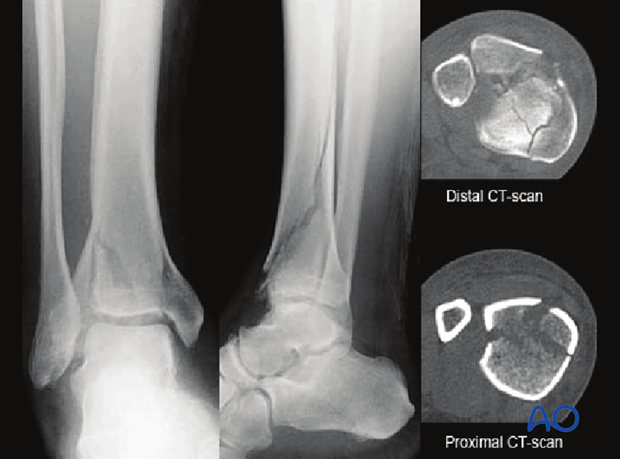
10. Case example
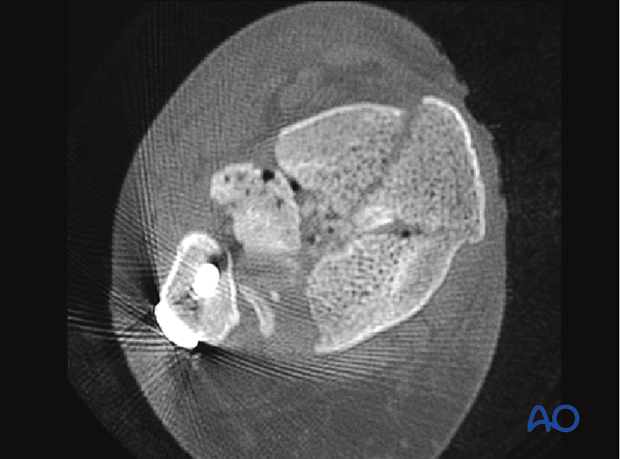
This 32-year old male sustained an injury to his left leg after a fall from height. The injury-radiographs demonstrate tibial shortening. The fibula is intact. The major three articular fragments – anterolateral, posterolateral and medial – are shown.
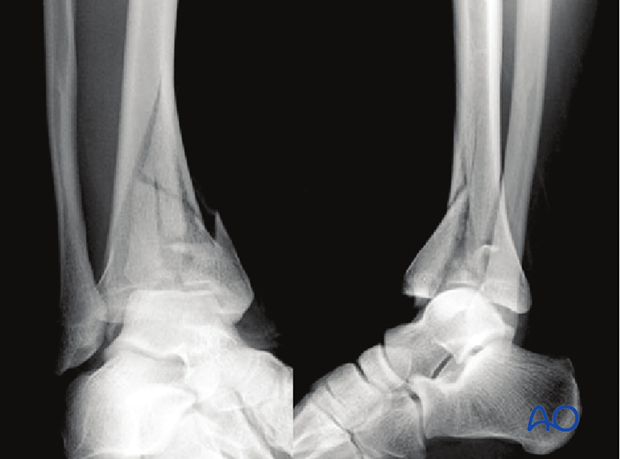
Initial management consisted of temporary spanning external fixation to allow recovery of the soft-tissue swelling. A CT scan was obtained after external fixation to allow for an accurate assessment of the articular injury.

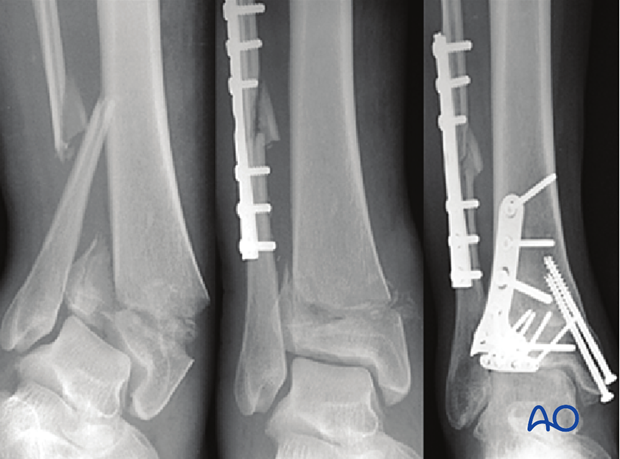
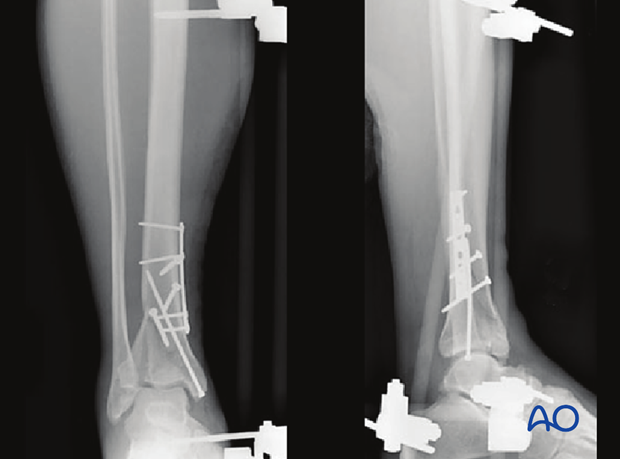
An anterolateral surgical exposure was used. Intraoperative articular visualization was optimized with a distractor spanning from the mid-tibia to the talar neck. Preliminary articular reduction was obtained, and K-wires were placed.
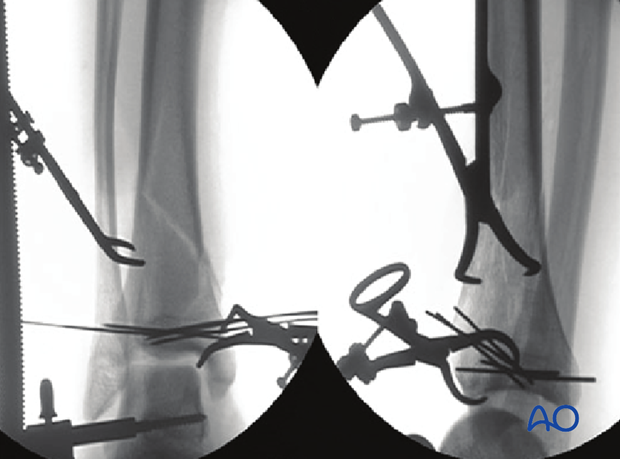
Small cortical lag screws were used to maintain the reduction and to allow for removal of the K-wires.

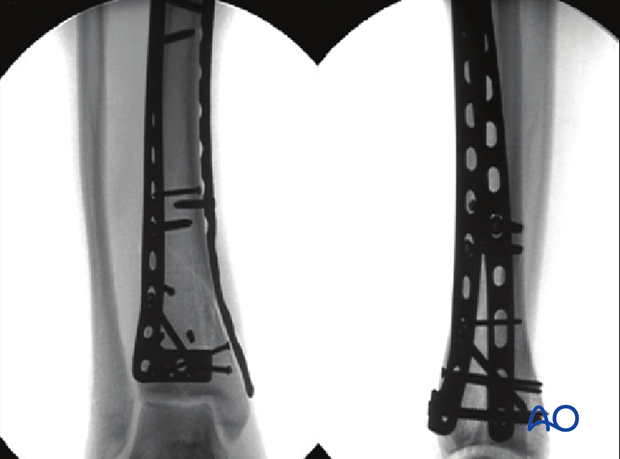
Definitive plate fixation consisted of an anterolateral non-locking plate combined with a medial non-locking plate. Both implants were placed through limited incisions using minimally invasive techniques. Proximal screw fixations were placed through small incisions.
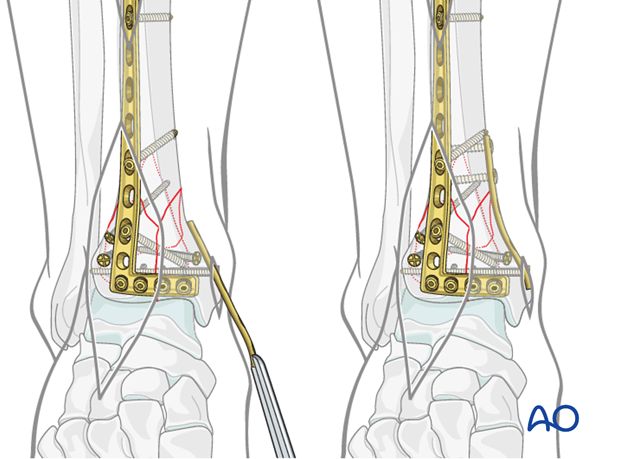
11. Fixation of fractures with proximal extension
Fractures with proximal diaphyseal extensions
In selected fracture patterns with a long oblique proximal extension of the posterior, or posterolateral articular fragment, early fixation of this fracture component may be advantageous. Early callus on the large fracture surface may hinder delayed reduction of such fragments.
Early fixation of such an articular fragment with long proximal extension, effectively converts a complete articular fracture pattern into a partial articular fracture pattern, simplifying the delayed articular reconstruction.
Plating the proximal extension
The CT-scan demonstrates where the fracture is located proximally on the posterior tibial surface. This area is exposed through a posteromedial approach. The fracture can be stabilized with lag screws, an antiglide plate, or combinations thereof.
In the illustrated case, fixation of the posterior fragment was performed acutely through a limited posteromedial approach at the time of initial bridging external fixation.
Definitive fixation
Definitive reconstruction of the articular surface is delayed until the soft tissues allow. The surgical approach and implants are determined based on the remaining fracture configuration.
In the illustrated case, definitive articular reconstruction of the anterior fractures was delayed for 16 days.

12. Aftercare following plating
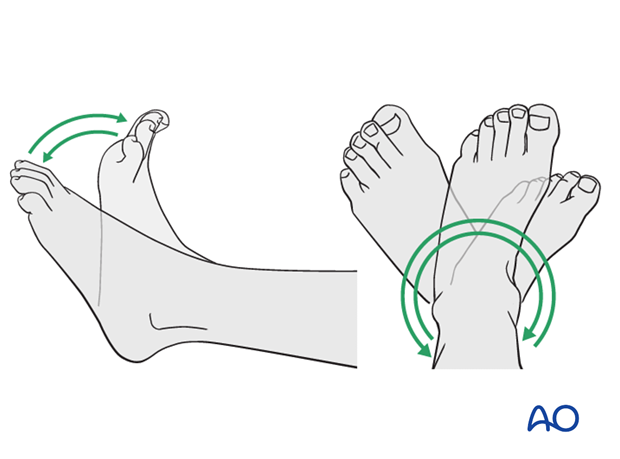
Leg elevation is recommended for the first 2-5 postoperative days. Physiotherapy with active assisted exercises is started immediately after operation. Immobilization is not necessary.
Mobilization
Starts depending on the wound healing with flat footed, weight of the leg weight bearing (10-20kg).
Follow up
Clinical and radiological follow-up is recommended after 2, 6 and 12 weeks. Depending on the consolidation, weight bearing can be increased after 6-8 weeks with full weight bearing usually after 3 months. Supervised rehabilitation with intermittent clinical and radiographic follow-up is advisable every 6-12 weeks until recovery reaches a plateau, typically 6-12 months after injury. Weight-bearing radiographs are preferable to assess articular cartilage thickness. Angular stable fixation may obscure signs of non-union for many months.
Implant removal
Implant removal may be necessary in cases of soft-tissue irritation by the implant (plate and/or isolated screws). The best time for implant removal is after complete remodeling, usually at least 12 months after surgery.