ORIF through extended iliofemoral approach
1. General considerations
Sequence of the treatment
For ORIF of T-shape fractures with extended iliofemoral approach, the following surgical sequence is common:
- Joint distraction and removal of incarcerated fragments
- Reduction of femoral head dislocation if not achieved closed on admission
- Assessment of reduction
- Fixation of the anterior column
- Fixation of the posterior column
Planning/templating
Preoperative templating is essential for understanding the complexity of an acetabular fracture.
When using implants on the innominate bone, it is important to know the best starting points for obtaining optimal screw anchorage (see General stabilization principles and screw directions).
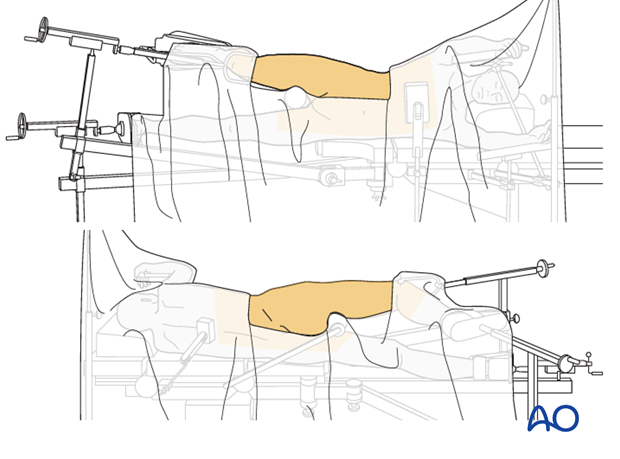
Patient positioning
The patient is positioned lateral on a flat top radiolucent table or a fracture table. Typically, a distal femoral traction pin is applied to allow the application of traction and also to stabilize the extremity. The knee is flexed 45°.
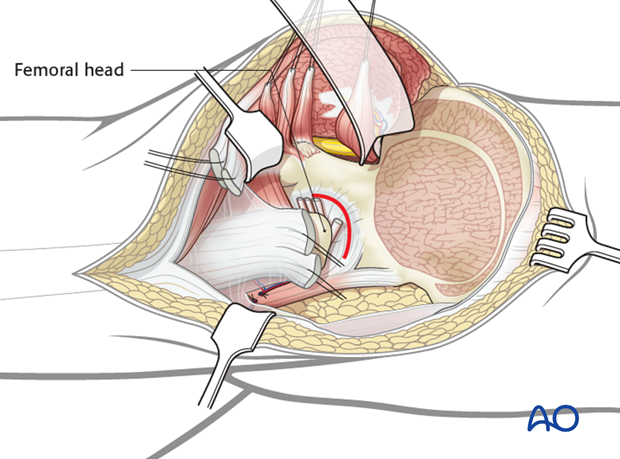
Capsulotomy
The extended iliofemoral approach allows the hip joint to be opened with a capsulotomy, just distal to the labrum. Lateral and/or distal retraction of the femoral head makes it easier to see into the joint.
It also allows the fracture to be seen well on the external surfaces of both the anterior and the posterior columns.
The internal surface of the pelvis can be palpated with a finger in the greater sciatic notch, for further assessment of the reduction.
Indirect visualization
Unusually for a significant joint, articular reduction of acetabular fractures is indirect. The articular surface of the hip joint is not seen directly. Reduction must be assessed by the appearance of the extraarticular fracture lines and intraoperative fluoroscopic assessment. Some fracture lines are palpated manually but not seen directly such as transverse fracture lines on the quadrilateral plate.
Quality of reduction
Posttraumatic arthrosis is directly related to the quality of reduction - the better the reduction, the greater the chance of a good or excellent result.
Teaching video
AO teaching video: Transtectal T-shaped fracture through extended iliofemoral approach
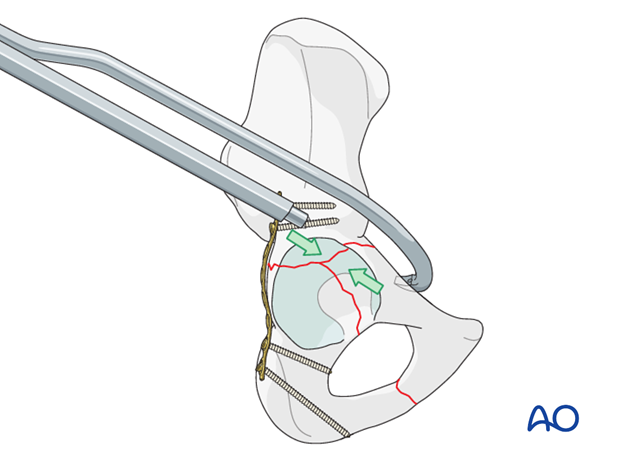
2. Joint distraction
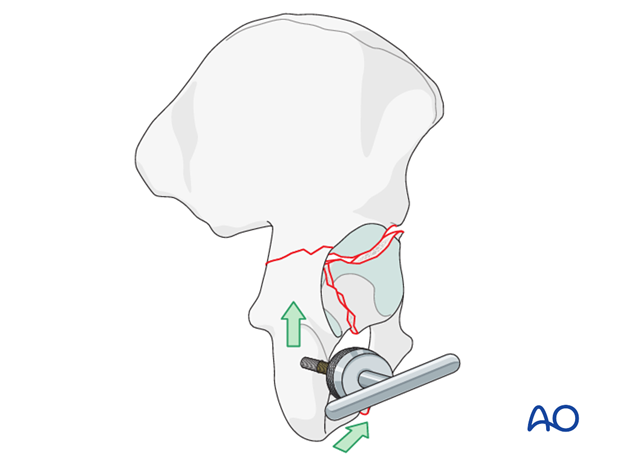
Lateral traction is applied to extract the displaced femoral head from the pelvis. This also allows some indirect reduction of the medially displaced fracture fragments by ligamentotaxis. Lateral traction is typically achieved with a Schanz screw applied through the lateral greater trochanter region of the femur. Because the patient is in the lateral position, this typically requires a manual force.
Longitudinal traction is also required to correct proximal displacement. Longitudinal traction can be obtained with a fracture table applied to a distal femoral traction pin (A), a femoral distractor (B), or with manual traction on the affected extremity.
In some surgeon’s experience, the use of a traction table post or other traction frame is helpful during this operation.
Note
Excessive longitudinal or lateral traction may result in the locking of the fracture, inhibiting further reduction maneuvers. Furthermore, the position of the femur may affect reduction and visualization. Commonly, one must reposition the involved extremity and change the vector of traction several times during the course of the operation. Thus, it must be easy to adjust the traction and the limb position intraoperatively.

Teaching video
AO teaching video: Use of the distractor on the pelvis
3. Cleaning of the fracture site
Fracture sites are prepared by preliminarily increasing the displacement and then removing early callus and granulation tissue.
Joint distraction is extremely useful to facilitate this debridement. If the femoral head is still dislocated then the joint can be cleaned before reduction.
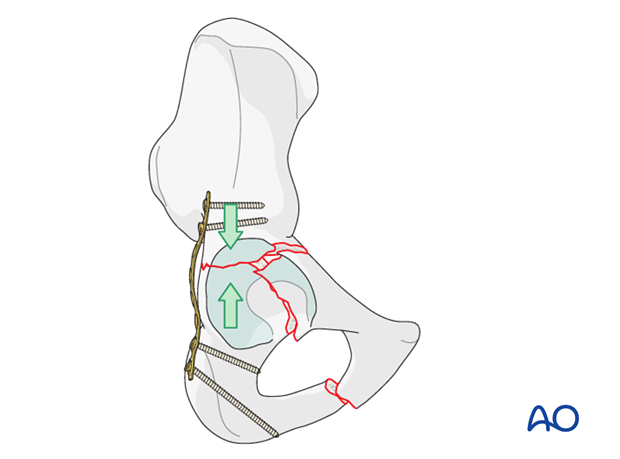
4. Posterior column: reduction
Principles
In the majority of T-type fractures, the posterior column is addressed first.
Control of the posterior column is facilitated by placement of a joystick in the ischium. This allows gross control of rotation around the stem of the T-fracture.
Assessment of reduction requires both visual assessment of the joint surface and digital palpation of the reduction, medially, on the quadrilateral surface.
Final assessment of reduction is also augmented by intraoperative fluoroscopy.
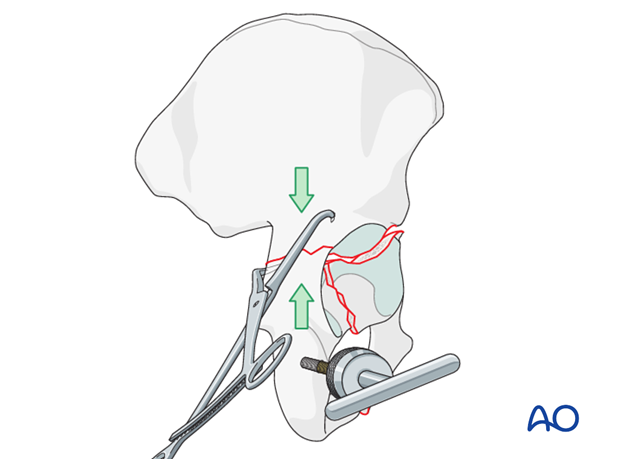
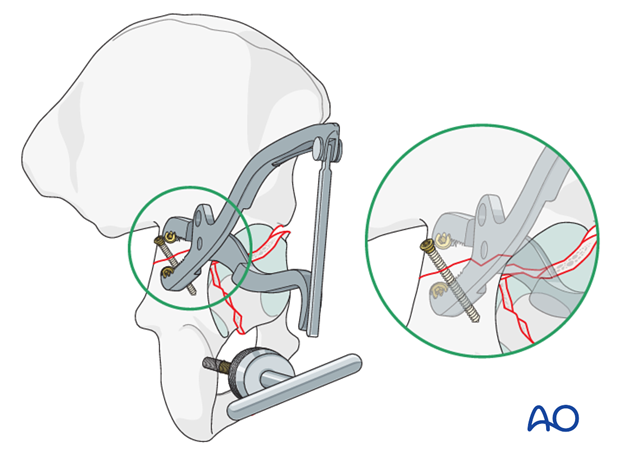
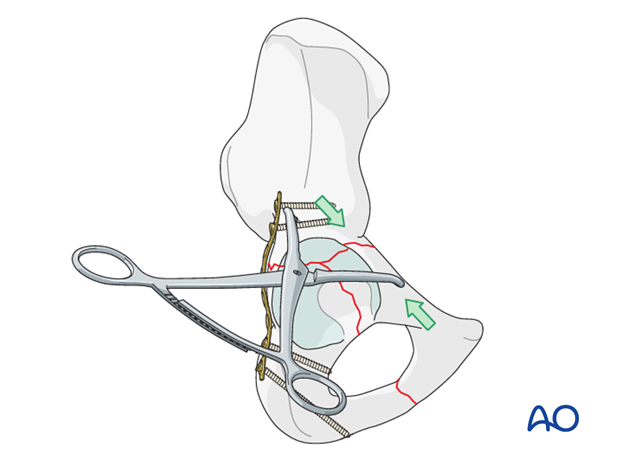
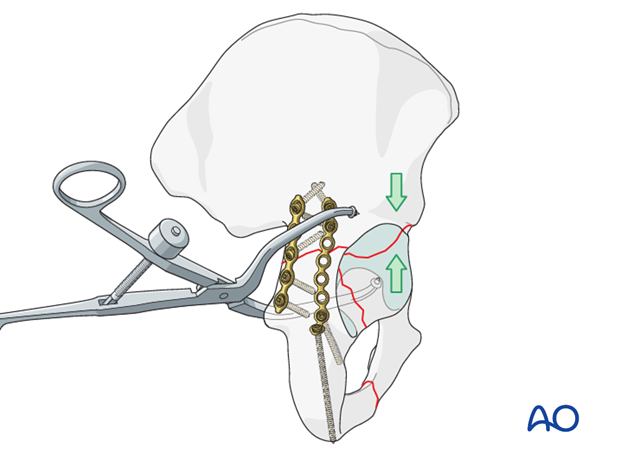
Use of reduction forceps
Appropriately chosen and placed forceps can aid reduction and provisional stabilization of the ischiopubic segment.
The pointed reduction forceps (or Weber clamp) is a very powerful reduction tool. It may be necessary to drill a small hole for application of the clamp points to prevent slipping on the convexity of the retroacetabular surface.
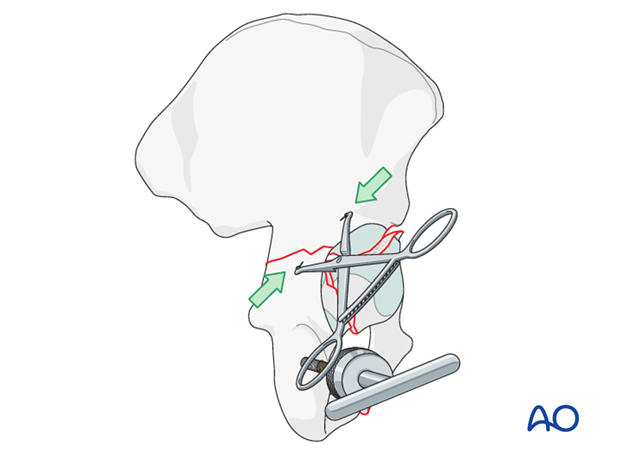
The distal end of a pointed reduction or a quadrangular clamp can be applied onto the quadrilateral surface through the greater sciatic notch. This also compresses the posterior column fracture, and may help close a medial gap.
A Farabeuf clamp, applied to screws in proximal and distal fragments, is shown reducing the posterior column fracture.
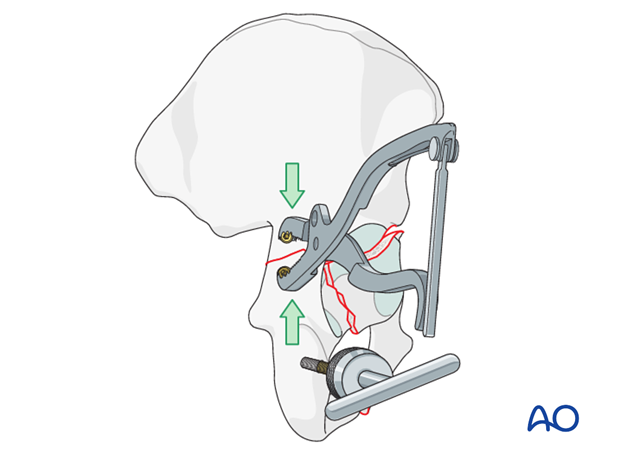
A small Jungbluth clamp, applied to screws in proximal and distal posterior column fragments, can also be used.
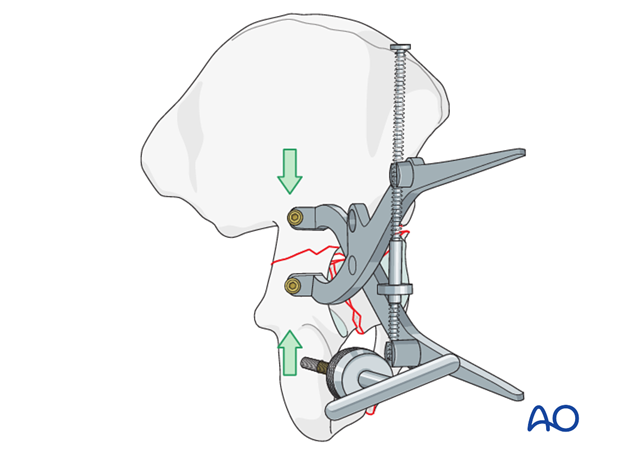
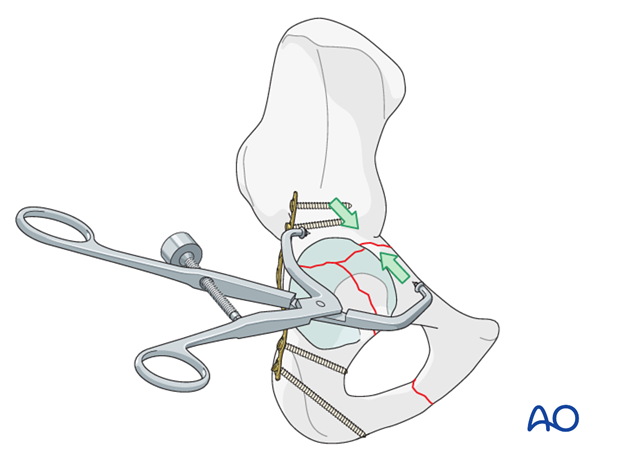
Plate reduction techniques
A 2.7 or 3.5 mm plate which spans the posterior column adjacent to the greater sciatic notch is fixed distally with a single screw.
This acts as a reduction aid analogous to a clamp placed through the greater sciatic notch.
When the screw attaching the plate to the distal fragment is tightened, pressure of the plate on the proximal fragment reduces the anteriorly displaced distal fragment.
Note: Protect the sciatic nerve
It is frequently necessary to combine reduction techniques to achieve optimum reduction.
Protection of the sciatic nerve while working in the greater sciatic notch is critical. Hip extension and knee flexion decrease sciatic nerve tension and thus improve its mobility.
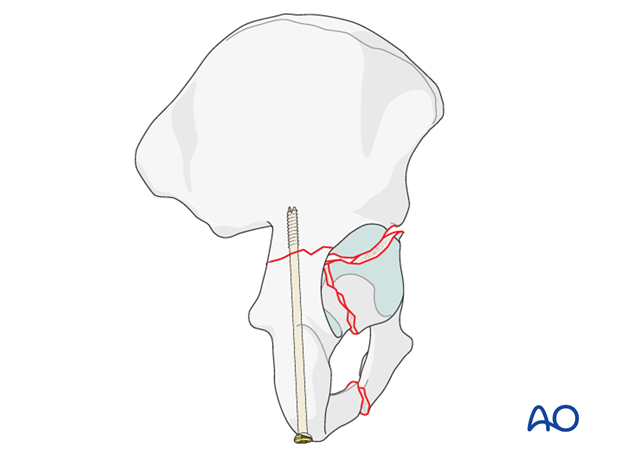
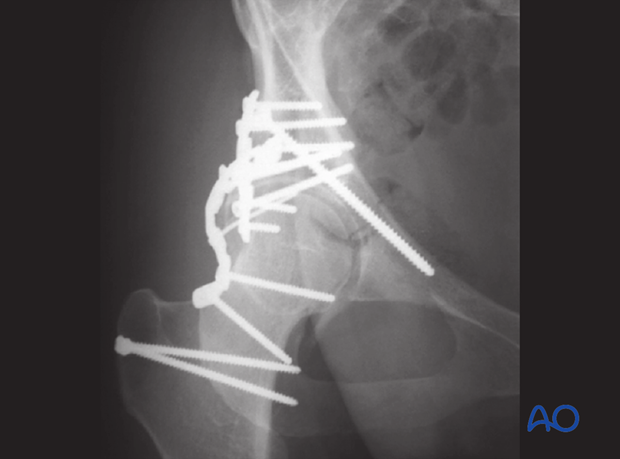
5. Posterior column: fixation
Initial screw fixation
The posterior column may be stabilized with a plate or column screw.
If using a plate for definitive fixation, then it may be possible to preliminarily stabilize the column with a lag screw, followed by a plate.
Initial plate fixation
When screw fixation is impossible, then either the final plate is placed initially or preliminary fixation is achieved with a small reconstruction plate along the greater sciatic notch to hold the reduction, before a longer plate is added to complete the fixation. The first plate may either be retained or removed.
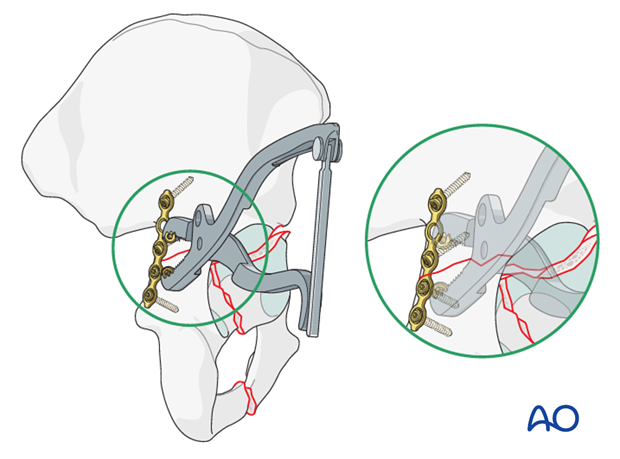
Final plate fixation
Fixation of the posterior column is completed using a pelvic reconstruction plate which spans from the ischium to the supraacetabular area. The contouring of this plate is critical since it must exert some compression on the anterior aspect of the posterior column fracture.
Patterns involving the posterior wall require definitive reduction of the wall fragments before application of this plate. Techniques for management of posterior wall fractures are discussed in the operative treatment option for posterior wall fractures, eg for transverse/posterior wall fractures.
Reduction and fixation of the posterior wall is generally the last component of the reconstruction.
Note
Posterior column fixation implants must be placed in locations that do not prevent anterior column reduction.
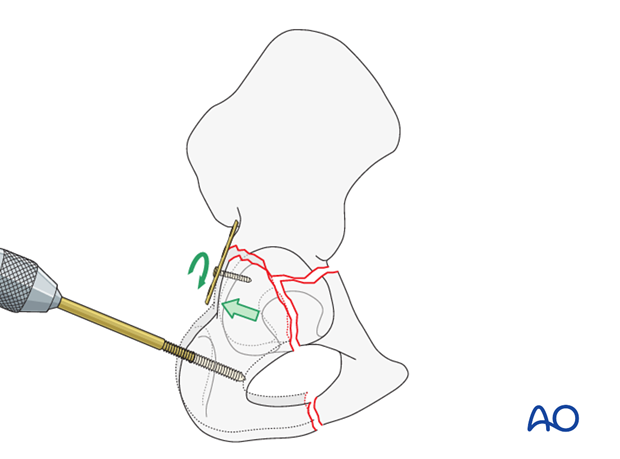
Posterior column screw
An axial posterior column screw provides interfragmentary compression across the posterior part of the fracture. This is inserted from distal to proximal.
A 7.3 mm partially threaded cannulated screw is inserted through a separate stab incision in the buttock crease over a guide wire.
The start point is at the ischial tuberosity, and a finger in the greater sciatic notch is used to guide the wire and screw up the posterior column, exiting at the pelvic brim.
Care is taken to protect the sciatic nerve at the level of the ischial tuberosity.
The use of a screw aids the placement of the posterior wall plate as it increases the freedom of placement of the wall plate.
This is commonly referred to as the “butt screw”.
6. Anterior column: reduction
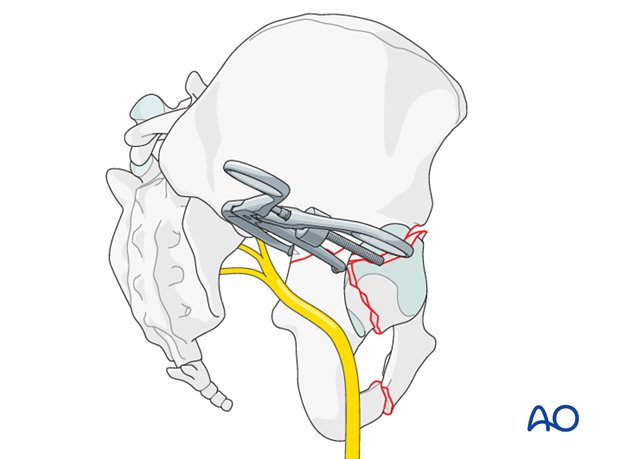
Clamp placement
Reduction clamps can be placed from the supraacetabular surface to the area of the iliopectineal surface easily through the extended iliofemoral approach.
The image shows placement of a pointed reduction forceps.
Alternatives for anterior column reduction are the oblique pelvic reduction (quadrangular) clamp, …
… or the collinear clamp.
Additional posterior clamp placement
Should the anterior fracture gape on the quadrilateral surface, an additional clamp placed from posterior may correct this displacement.
This illustration shows a quadrangular clamp.
Accuracy of reduction must be verified by direct articular visualization.
This illustration shows a pointed reduction forceps, applied from posteriorly, as another supplementary option for anterior column reduction.

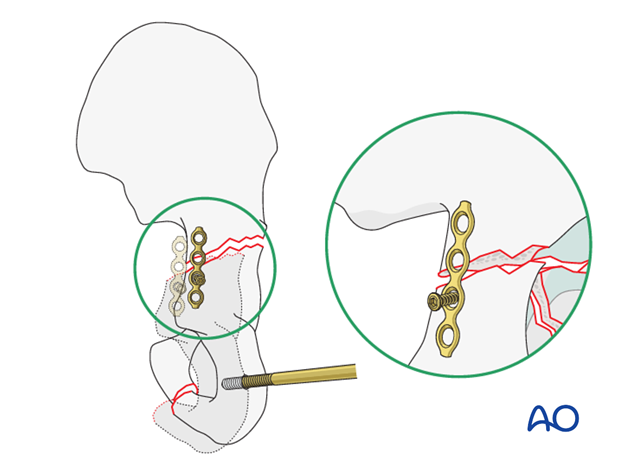
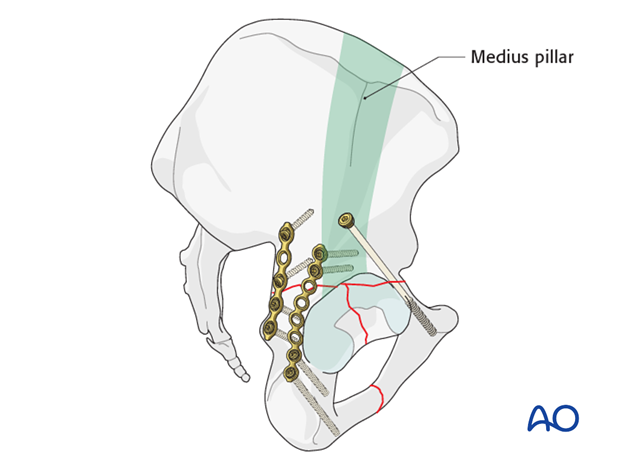
7. Anterior column: fixation
Anterior column fixation consists of position or lag screws in all cases.
The starting point for these screws is in an area of the innominate bone 2-3 cm cranial to the joint margin along the posterior margin of the gluteus medius pillar. Care must be taken to ensure that lag screws are inserted perpendicular to the anterior column primary fracture plane. Secondary displacement will occur with screw tightening when this is not achieved.
In some cases, placement of a position screw, after reduction and clamp compression, is a more prudent choice.
A 7.3 mm partially threaded screw is usually used to offer compression of the anterior portion of the transverse fracture.
A 2.8 mm guidewire is inserted along the anterior column before the appropriate length screw is passed over the wire.
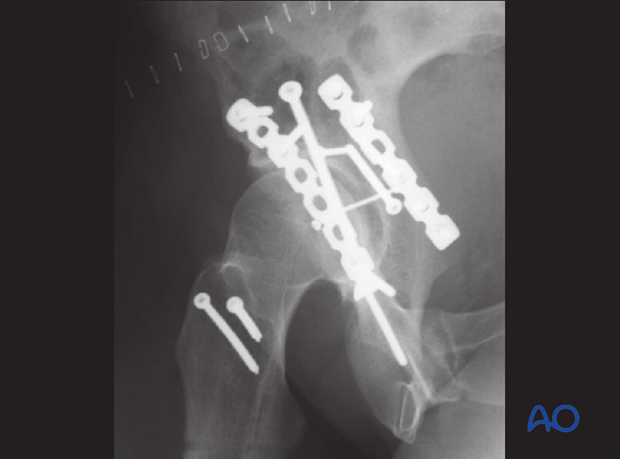
8. Radiographic assessment
Intraoperative confirmation of hardware position
During reduction and fixation, take fluoroscopic images in AP, iliac, and obturator oblique views to confirm reduction and/or screw placement.
To confirm that the screws are extraarticular an image exposed with the fluoroscope’s central ray superimposed on the long axis of the screw is taken.
Final radiographic assessment
Once all fixation is in place, confirm the appropriate appearance of AP, obturator oblique and iliac oblique views and check the location of any screw that is placed near the hip joint.
The AP view should be inspected to assure that congruence has been obtained. The femoral head should have the same relationship to the radiological roof, the anterior rim and the posterior rim as on the contralateral side.
If the low anterior column was affected, the obturator foramen profile and symphysis should be inspected to assess the quality of the distal reduction.
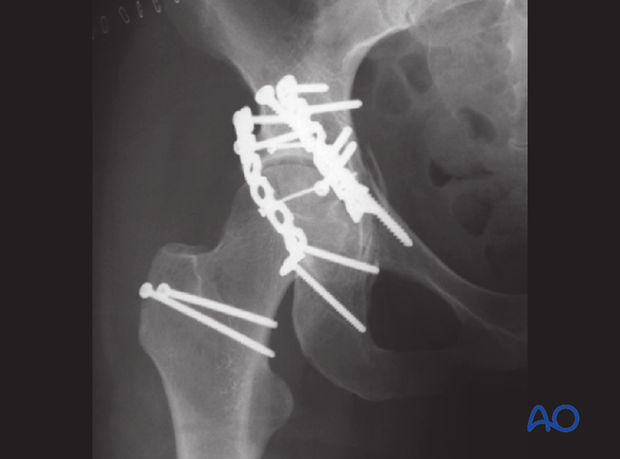
The lag screw should be seen to be crossing the level of the transverse fracture, and the lower plate screws should be directed down the ischium and not in the direction of the posterior wall.
If a posterior wall fragment was involved, it should be seen as reduced and stabilized on this image.
The accuracy of the reduction of the trochanteric osteotomy fragment can be confirmed on this view.
Iliac oblique should be inspected to ensure that the posterior column reduction is anatomic. The screws directed down the posterior column should be inspected and verified as extraarticular.
Postoperatively, obtain formal high-quality radiographs of AP and both oblique views.
9. Postoperative care
During the first 24-48 hours, antibiotics are administered intravenously, according to hospital prophylaxis protocol. In order to avoid heterotopic ossification in high-risk patients, the use of indomethacin or single low dose radiation should be considered. Every patient needs DVT treatment. There is no universal protocol, but 6 weeks of anticoagulation is a common strategy.
Wound drains are rarely used. Local protocols should be followed if used, aiming to remove the drain as soon as possible and balancing output with infection risk.
Specialized therapy input is essential.
Following the extended iliofemoral approach, the patient’s leg may be positioned in abduction in order to reduce tension on the muscles of the reconstructed area.
Follow up
X-rays are taken for immediate postoperative control, and at 8 weeks prior to full weight bearing.
Postoperative CT scans are used routinely in some units, and only obtained if there are concerns regarding the quality of reduction or intraarticular hardware in others.
With satisfactory healing, sutures are removed around 10-14 days after surgery.
Mobilization
Early mobilization should be stressed and patients encouraged to sit up within the first 24-48 hours following surgery.
Mobilization touch weight bearing for 8 weeks is advised.
Weight bearing
The patient should remain on crutches touch weight bearing (up to 20 kg) for 8 weeks. This is preferable to complete non-weight bearing because forces across the hip joint are higher when the leg is held off the floor. Weight bearing can be progressively increased to full weight after 8 weeks.
With osteoporotic bone or comminuted fractures, delay until 12 weeks may be considered.
Implant removal
Generally, implants are left in situ indefinitely. For acute infections with stable fixation, implants should usually be retained until the fracture is healed. Typically, by then a treated acute infection has become quiescent. Should it recur, hardware removal may help prevent further recurrences. Remember that a recurrent infection may involve the hip joint, which must be assessed in such patients with arthrocentesis. For patients with a history of wound infection who become candidates for total hip replacement, a two-stage reconstruction may be appropriate.
Sciatic nerve palsy
Posterior hip dislocation associated with posterior wall, posterior column, transverse, and T-shaped fractures can be associated with sciatic nerve palsy. At the time of surgical exploration, it is very rare to find a completely disrupted nerve and there are no treatment options beyond fracture reduction, hip stabilization and hemostasis. Neurologic recovery may take up to 2 years. Peroneal division involvement is more common than tibial. Sensory recovery precedes motor recovery and it is not unusual to see clinical improvement in the setting of grossly abnormal electrodiagnostic findings.













