Closed reduction
1. General considerations
Bleeding
Nasal fractures can cause significant bleeding. Proper techniques for hemostasis should be applied before any diagnostic procedure and any definitive treatment of nasal fractures.
Read more about hemostasis here.
Choice of anesthesia
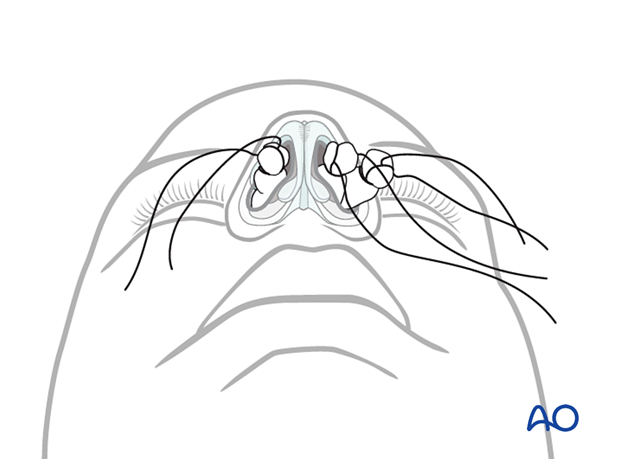
Local anesthesiaClosed reduction of nasal fractures can be performed under local anesthesia for most patients. It is highly dependent on the skill and thoroughness of the operator and the ability to establish proper local anesthesia and patient cooperation.
The nasal cavity should be prepared with cotton pledgets moistened in a solution of a topical anesthetic with a vasoconstrictor. In addition, a local anesthetic is injected to block the bilateral infratrochlear and infraorbital nerves. An additional amount of local anesthesia is infiltrated in the area of the anterior nasal spine.
Intravenous sedation may be added for the comfort of the patient.
General anesthesia is an option according to patient’s preference and is preferred by many practitioners who wish to minimize the incidence of secondary surgery.
2. Fracture reduction instruments
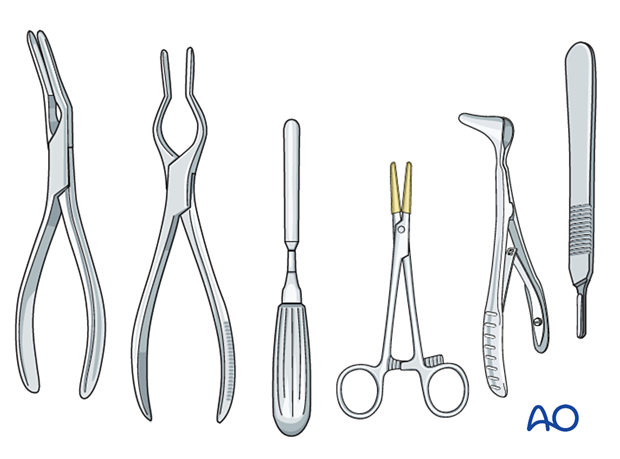
Instruments commonly used for closed treatment of nasal fractures are:
- Asch septum-straightening forceps
- Walsham septum-straightening forceps
- Boies nasal fracture elevator
- Mayo hemostat with rubber tubing
- Killian nasal septum speculum
- Back of a number 3 scalpel handle (without blade)
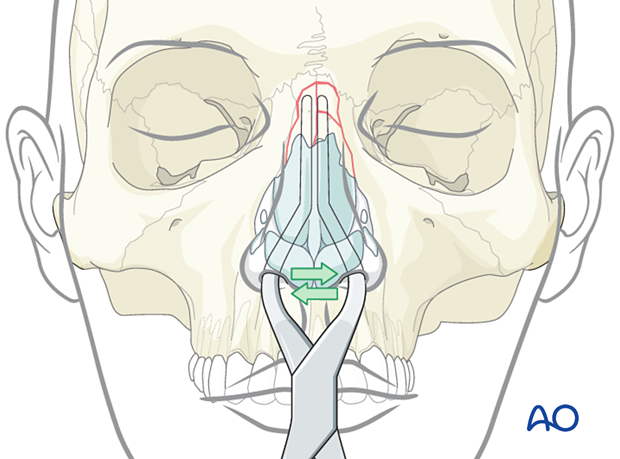
3. Reduction of nasal bones
In laterally displaced fractures
Laterally displaced fractures on one side are commonly medially depressed on the other side. They are often partially fractured or incomplete on both sides. If the fracture is not satisfactorily completed on both sides, repeat displacement is likely.
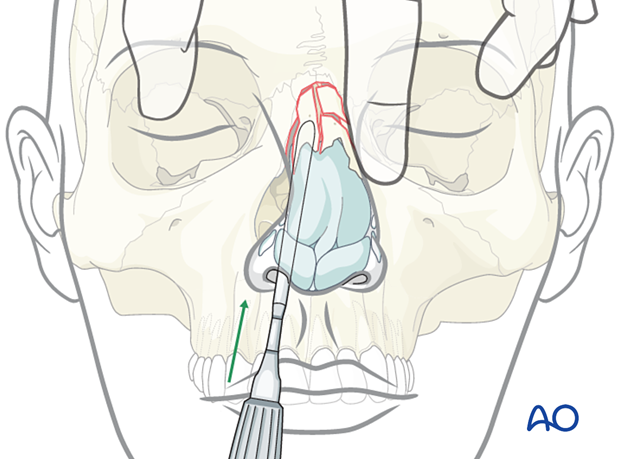
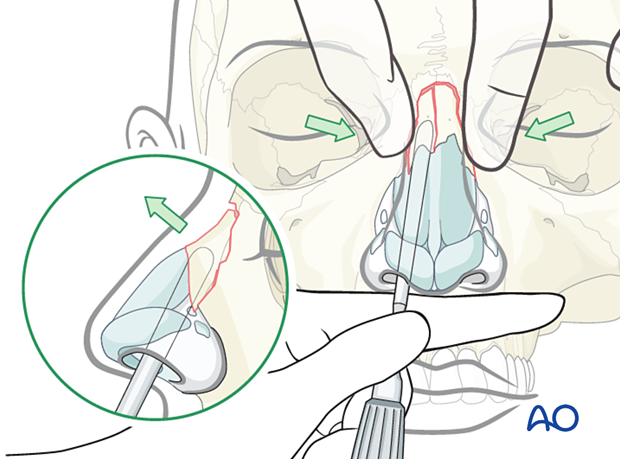
An instrument such as a Boies elevator, or the back of a #3 scalpel handle, may be placed under the nasal bone on each side, one at a time. The elevator is placed between the nasal septum and the nasal bone.
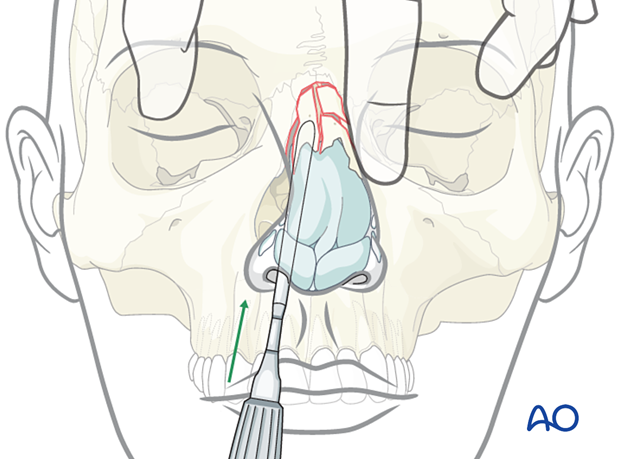
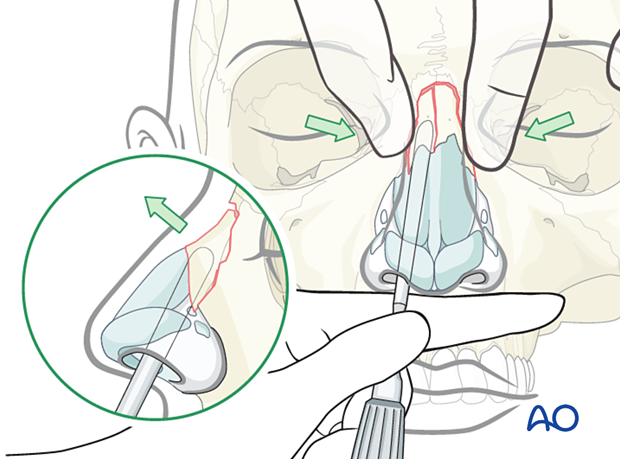
Place the elevator up against the ipsilateral nasal bone and rotate with a simultaneous movement directed upward and outward. This will allow the completion of the fracture. The procedure is then repeated on the contralateral side.
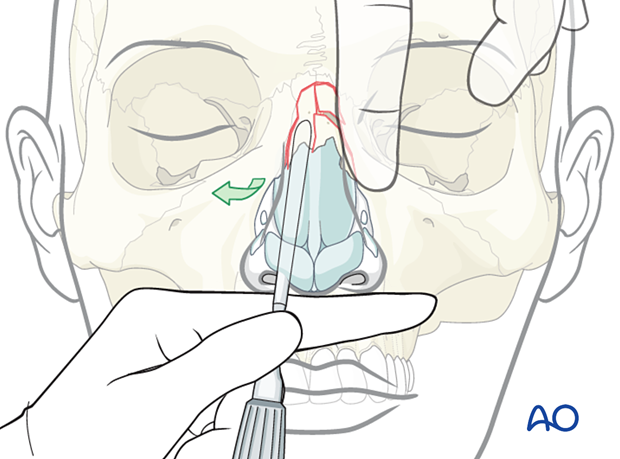
The nasal bone remains outwardly dislocated and rotated away from the nasal septum.
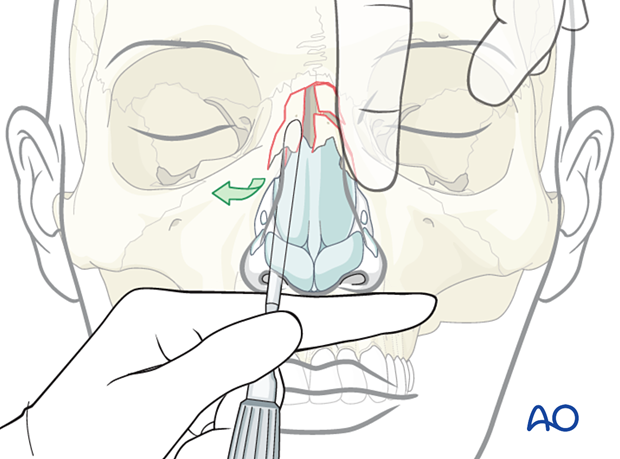
Using finger pressure, the nasal bone may be maneuvered towards the septum and into the correct position. The reduction is confirmed by visual inspection.
If there is resistance to maneuvering the nasal bone to the correct position, or if there is resistance to keeping it in the reduced position, refracture displacement maneuvers should be repeated until the nasal bone does not resist remaining in the reduced position.
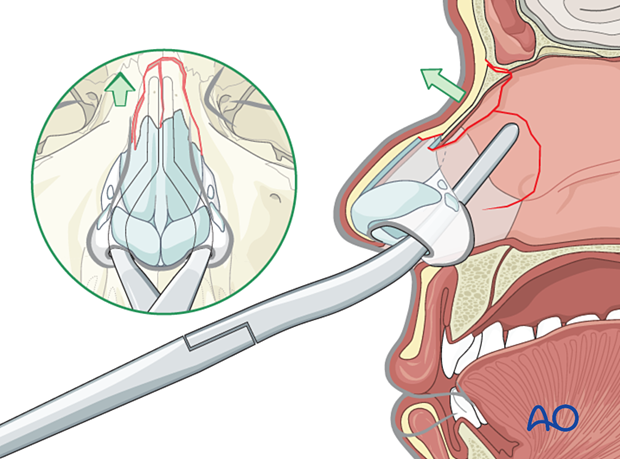
Posteriorly dislocated nasal fracture
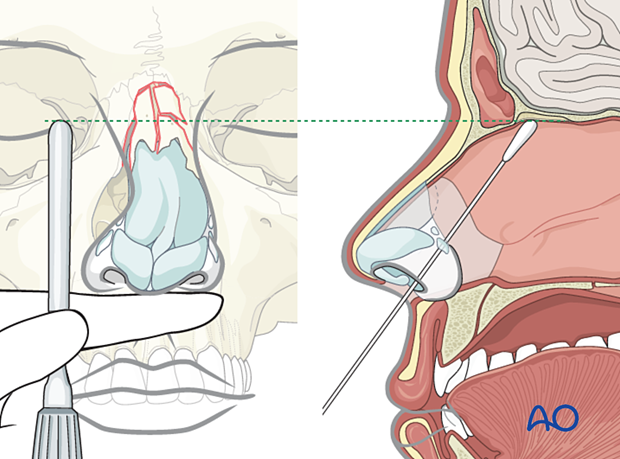
Sometimes the nasal bones are dislocated posteriorly.
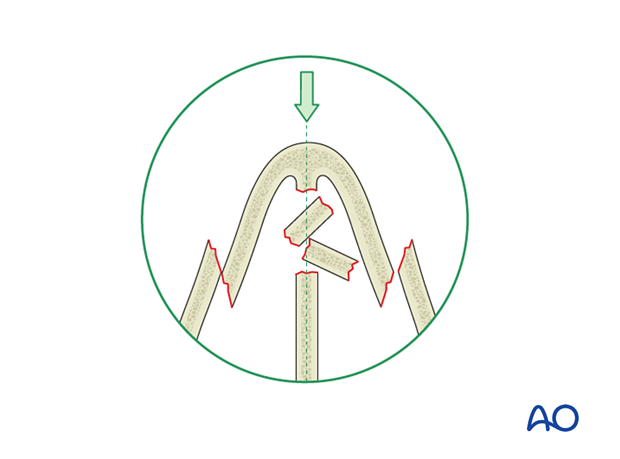
Reduction requires elevation and stabilization of the posteriorly displaced nasal bones.
The elevator is placed under each posteriorly displaced nasal bone fragment one at a time. Each dorsal nasal pyramid half is elevated superiorly, one at a time, until a better position for that fragment is achieved by palpation.
Any adhesions or partial fractures are disrupted or completed respectively.
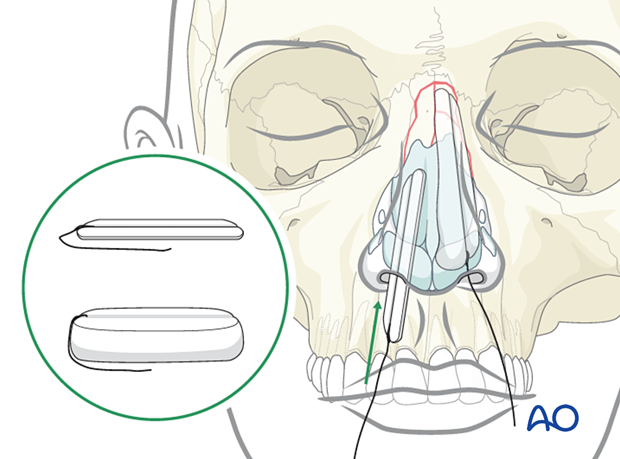
Then, packing material is placed in the nasal cavity, between the septum and the nasal bone.
As the packing material absorbs moisture within the nasal cavity, it expands to provide additional support to the nasal bone.
4. Closed reduction
Alternative technique
In some cases, Asch or Walsham forceps can elevate the dorsum and disimpact the displaced septum.
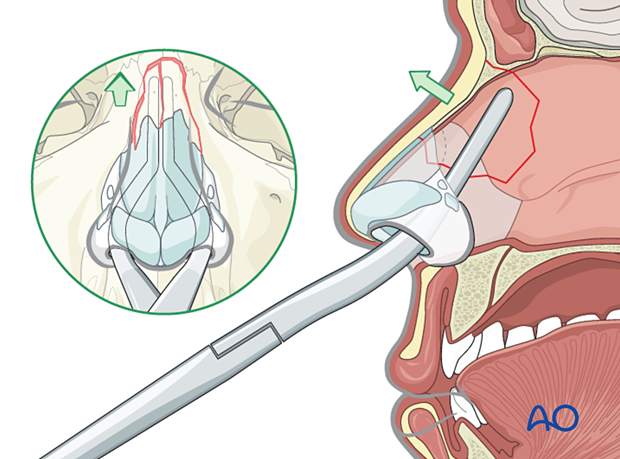
Closed reduction requires indirect elevation of the nasal bones to restore the architecture of the nasal pyramid.
5. Reduction of the nasal septum
Asch or Walsham septum-straightening forceps are also used to straighten the nasal septum.
The nasal septum is grasped with the blades of the instrument and gently manipulated into proper alignment.
Centrally depressed fractures require posterior to anterior elevation, which can often be achieved by reducing the nasal septum.
6. Splinting
Nasal bones
After reduction, adhesive strips are placed over the skin of the nasal dorsum, and the nasal bones are splinted using an external splint that conforms to the patient’s nose. If the nasal bones are comminuted or loose, they should be supported with intranasal packing, which should be placed before placing the external splint.
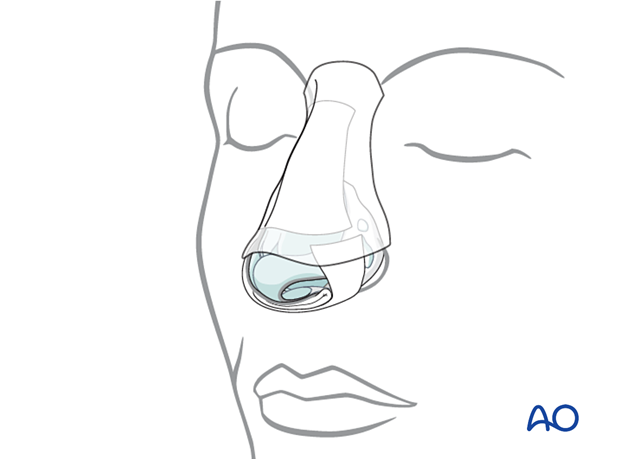
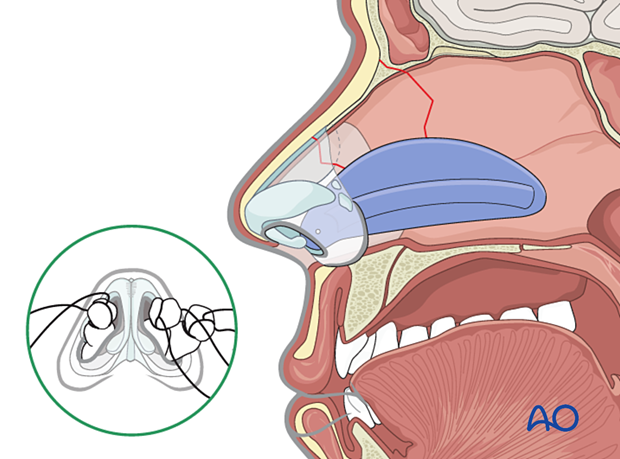
Nasal septum: Doyle splint
The nasal septum can be stabilized with splints (Doyle) or packs.
Doyle splints are made from silicone and are placed on either side of the septum, secured by one or more sutures. They are designed to prevent the formation of a septal hematoma, splint septal cartilage, and maintain an open airway.
Removal of packing and splints
Packing used for control of acute bleeding can be removed after 24 hours.
Any packing supporting the nasal bones must be left in place for 5–7 days and for as long as the external splint is in place.
The patient should be prescribed antibiotic treatment for as long as the nasal packing is in place to avoid toxic shock syndrome.
7. Aftercare
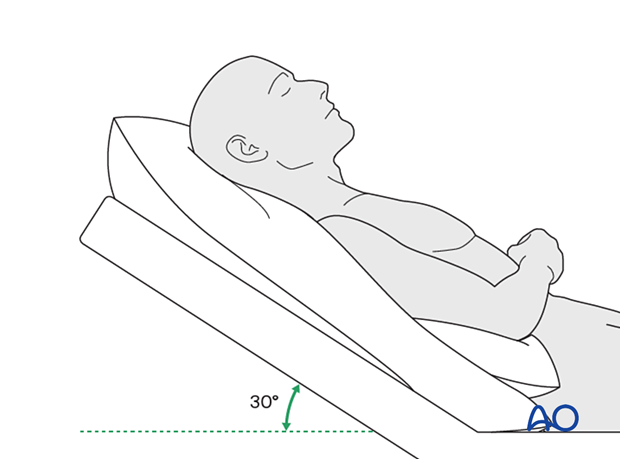
Postoperative positioning
Keeping the patient’s head in a raised position both preoperatively and postoperatively may significantly reduce edema and pain.
Nose blowing
Nose blowing should be avoided for at least ten days following fracture repair to prevent orbital emphysema.
Medication
The use of the following perioperative medication is controversial. There is little evidence to make strong recommendations for postoperative care.
- No aspirin for seven days (nonsteroidal anti-inflammatory drugs (NSAIDs) use is controversial).
- Analgesia as necessary.
- Antibiotic ointment may be smeared over the Doyle splint or intranasal packing to retard infection.
- Oral antibiotics given as long as nasal packing is in place. Sepsis has occurred from tight nasal packing.
- A nasal decongestant may be helpful for symptomatic improvement in some patients.
Postoperative imaging
For nasal fractures, postoperative CT imaging is usually not necessary except in severely comminuted fractures.
Wound care
Ice packs are effective in the short term to minimize edema.
Avoid sun exposure and tanning to skin incisions for several months.
Diet
Diet depends on the fracture pattern and the patient’s condition, but there are usually no limitations.
Clinical follow-up
Clinical follow-up depends on the complexity of the surgery and the patient’s postoperative course.
In all patients with nasal bone trauma, all the following should be periodically assessed:
- Nasal airway status
- Excess compression from the splint or intranasal material
- External nasal deformity
Other issues to consider are:
- Facial deformity (including asymmetry)
- Sensory nerve compromise
- Problems of scar formation
- Anosmia
- Epiphora and dacryocystitis













