ORIF without orbital reconstruction
1. General consideration
Due to the high incidence of greenstick fractures and the rapid reossification and remodeling, conservative treatment is often the best treatment in a pediatric patient.
Reduction alone may be adequate in some pediatric zygomaticomaxillary complex (ZMC) fractures due to the higher incidence of greenstick fractures. Moreover, multibuttress reconstruction is also less frequently indicated.
2. Approach
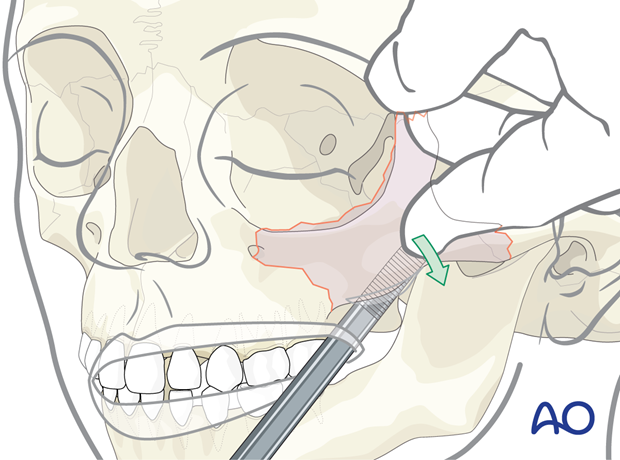
A vestibular incision is most commonly used to approach these fractures. A combination of lower eyelid incision and upper blepharoplasty incision may be added depending on the severity and the displacement of the fracture.
3. Reduction
The height, width, and projection of the midface should be restored.
An intraoral vestibular approach, such as the Keen approach, is used to reduce the zygomatic complex. A lateral/anterior force is applied with a Langenbeck periosteal elevator to the posterior surface of the zygoma. Other approaches are the Dingman and the Lothrop.
It is more common to have a stable reduction in children than in adults due to the greenstick nature of the fractures.
4. Aftercare
Patient vision is evaluated as soon as awakening from anesthesia and then at regular intervals until hospital discharge.
A swinging flashlight test may serve to confirm pupillary response to light in the unconscious or non-cooperative patient; alternatively, an electrophysiological examination while possible is seldom available in the operation area.
Postoperative positioning
Keeping the patient’s head in an upright position both preoperatively and postoperatively may significantly improve periorbital edema and pain.
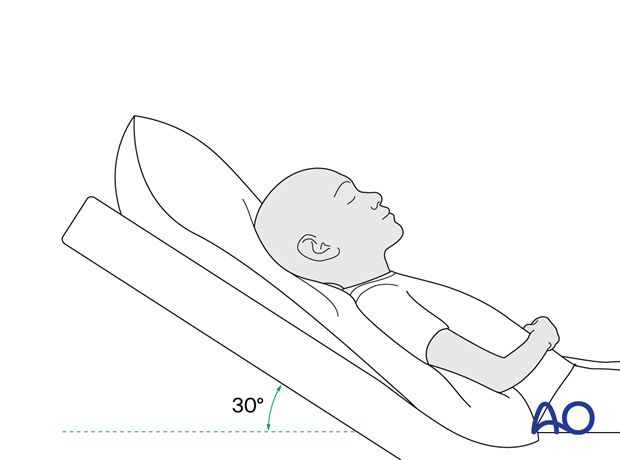
The patient is instructed not to lie down on the side of zygomatic fracture for at least 2 to 3 weeks postoperatively. A convenient method is to put two pillows beside the patient and a travel pillow around the neck to prevent direct pressure on the reduced fracture.

Nose blowing
Nose blowing should be avoided for at least ten days following orbital fracture repair to prevent orbital emphysema.
Medication
The use of the following perioperative medication is controversial. There is little evidence to make solid recommendations for postoperative care.
- No aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs) prescribed for 7 days.
- Provide analgesia as necessary.
- Antibiotics (many surgeons use perioperative antibiotics. There is no clear advantage of any antibiotic, and the recommended duration of treatment is debatable). More information can be found in the article: Mundinger GS, Borsuk DE, Okhah Z, et al. Antibiotics and facial fractures: evidence-based recommendations compared with experience-based practice. Craniomaxillofac Trauma Reconstr. 2015 Mar;8(1):64-78.)
- A nasal decongestant may be helpful for symptomatic improvement in some patients.
- Regular perioral and oral wound care must include disinfectant mouth rinse, lip care, etc.
Ophthalmological examination
Postoperative examination by an ophthalmologist may be requested. The following signs and symptoms are usually evaluated:
- Vision
- Extraocular motion (motility)
- Diplopia
- Globe position
- Visual field examination
- Lid position
- If the patient complains of epiphora (tear overflow), lacrimal duct function must be checked.
Postoperative imaging
Postoperative imaging should be performed within the first days after surgery to assess reductions and possible malpositioning. 3D imaging (CT, cone beam) is recommended to assess complex fracture reductions. An exception may be made for centers capable of intraoperative imaging.
Especially in fractures involving the alveolar area, orthopantomograms (OPG) are helpful.
Diet
Diet depends on the fracture pattern.
A soft diet can be taken as tolerated until there has been adequate healing of the maxillary vestibular incision.
Nasogastric feeding may be considered in cases with oral bone exposure and soft-tissue defects.
Clinical follow-up
Clinical follow-up depends on the complexity of the surgery and whether the patient has any postoperative problems.
Issues to consider are:
- Facial deformity (incl. asymmetry)
- Sensory nerve compromise
- Problems of scar formation
Oral hygiene
A soft toothbrush (dipped in warm water to make it softer) should be used to clean the surfaces of the teeth Chlorhexidine oral rinses or nonalcoholic mouth wash should be prescribed and used at least three times a day and after meals to help sanitize the mouth.













