Upper eyelid approach
1. General considerations
The upper eyelid approach, also called upper blepharoplasty, upper eyelid crease, and supratarsal fold approach is direct and usually provides a good esthetic outcome. It is the preferred approach to expose the frontozygomatic suture.
If there is no natural crease in the supratarsal fold lending itself for the incision line, the upper eyelid approach follows either the lower or upper limb of an elliptic upper blepharoplasty incision.
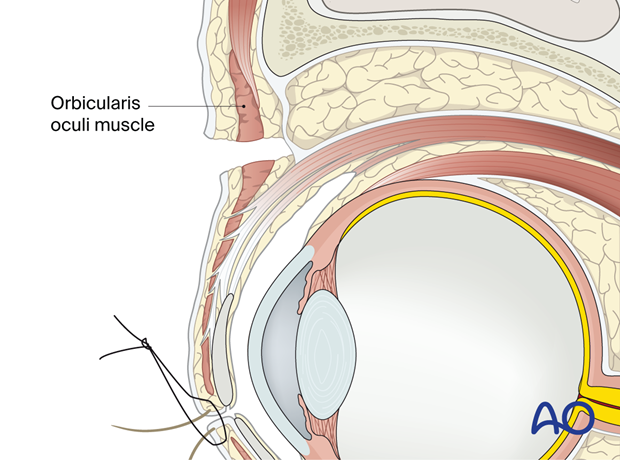
2. Anatomy
Access to the superolateral orbital rim starts at the skin extending through to the orbicularis oculi muscle layer. Skin muscle flaps are raised, leaving the orbital septum intact. The preaponeurotic space and the fat pads inside are not entered and serve as a buffer for critical underlying structures such as the levator aponeurosis. Gentle upward and lateral (temporal) traction of the wound edges facilitates access to the supra-periosteal plane over the lateral bony rim.
3. Protection of the globe
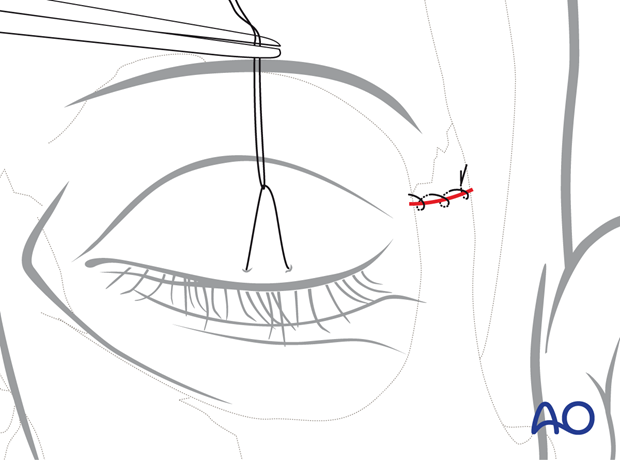
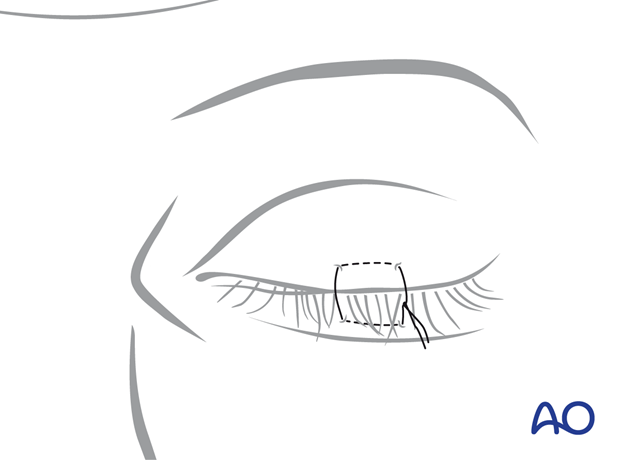
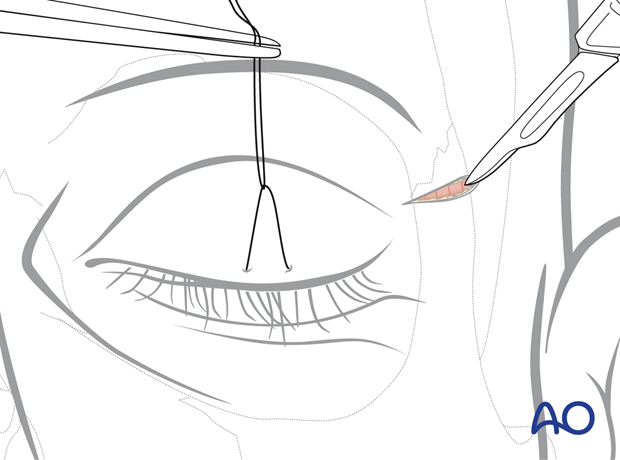
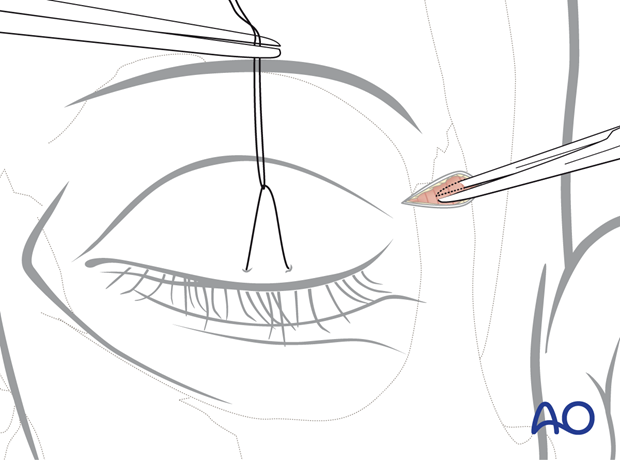
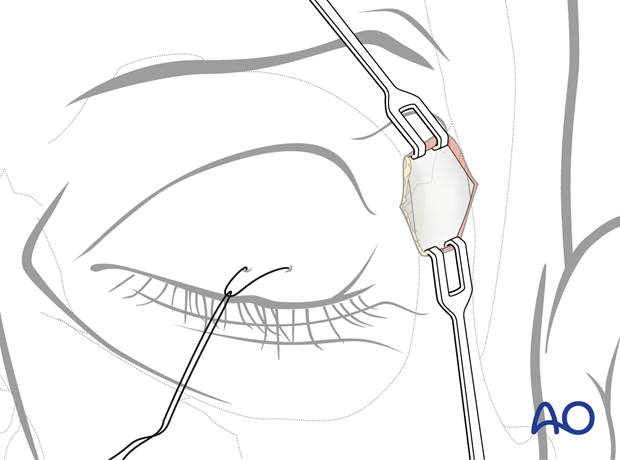
The cornea is protected with a temporary tarsorrhaphy or with a corneal shield.
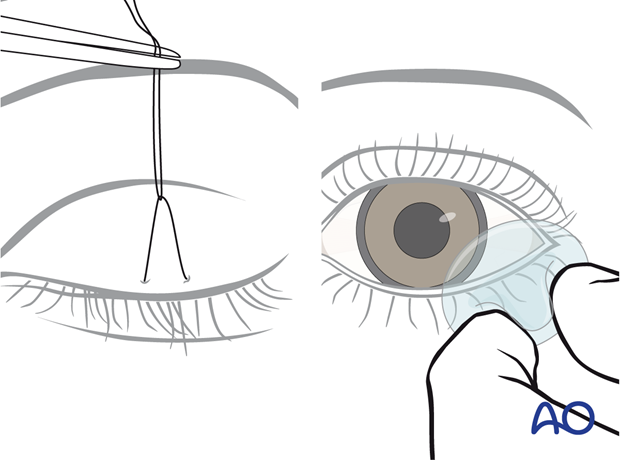
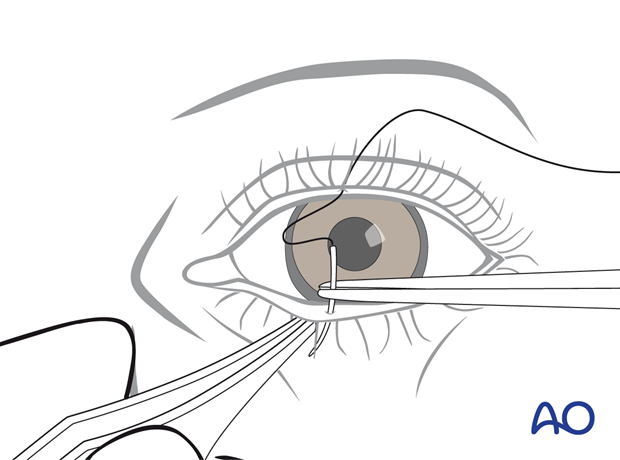
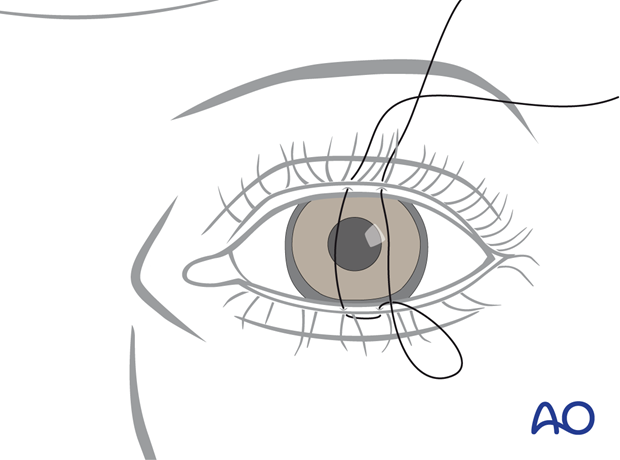
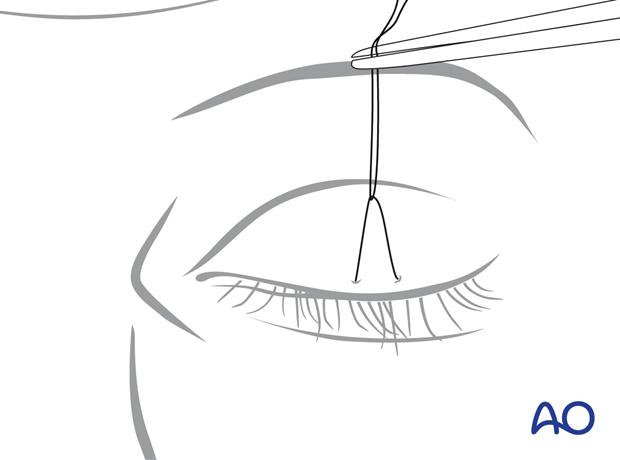
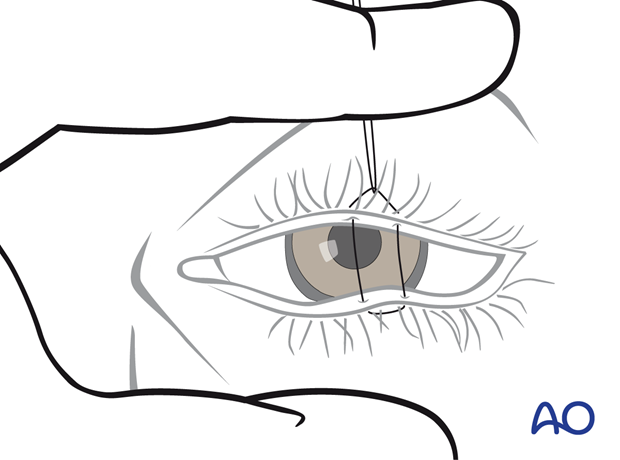
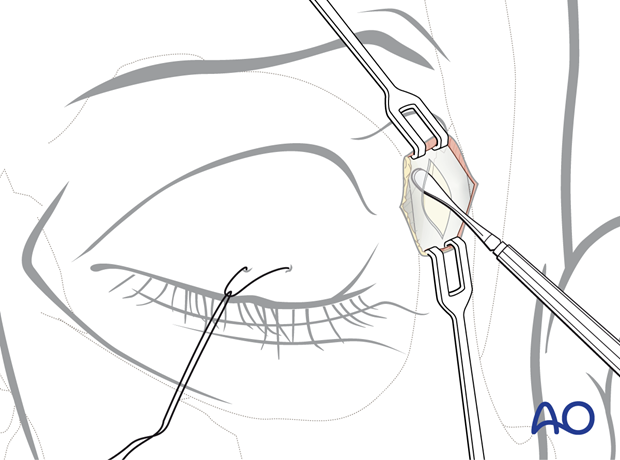
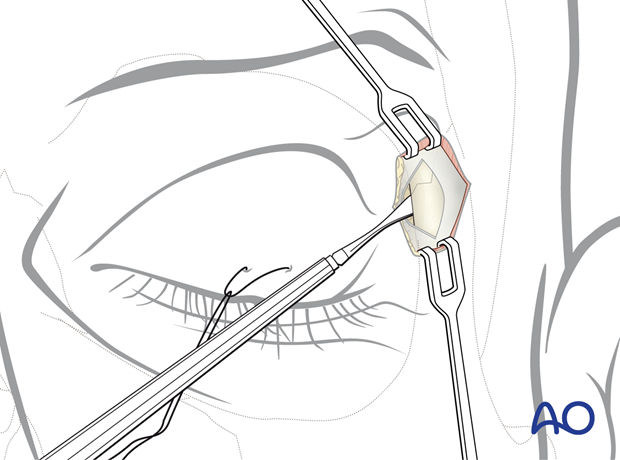
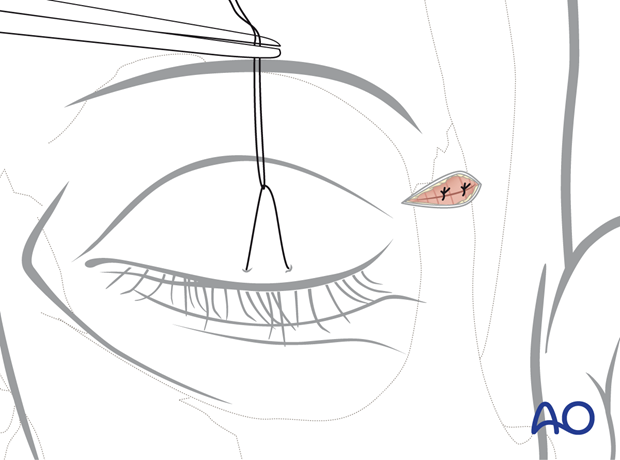
Below, the steps of a temporary tarsorrhaphy are shown.
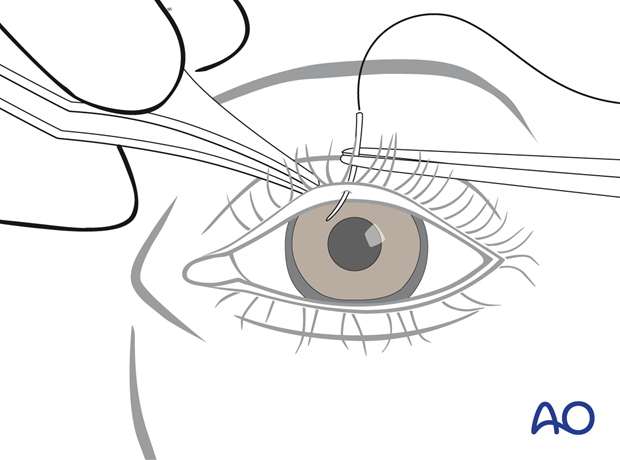
The needle is passed in the lower eyelid from the Gray line into the skin where it exits.
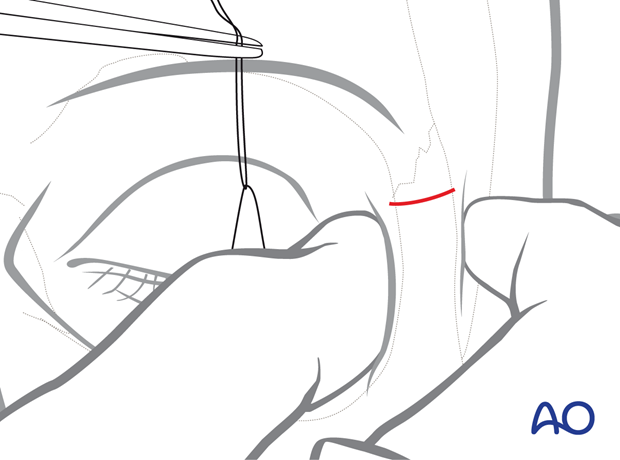
The suture is guided back, picking up the same soft-tissue portions in the lower and upper eyelids to complete the mattress loop.
The tarsorrhaphy is not secured tightly, and some space is left between the knot and the upper-eyelid skin. A hemostatic clamp is used to grasp the suture and apply traction to the lower lid for full eyelid closure during the surgical procedure.
Since the suture was not fully tightened, when the hemostatic clamp is released, the lid may be opened for a forced duction test or evaluation of the pupil during the procedure.
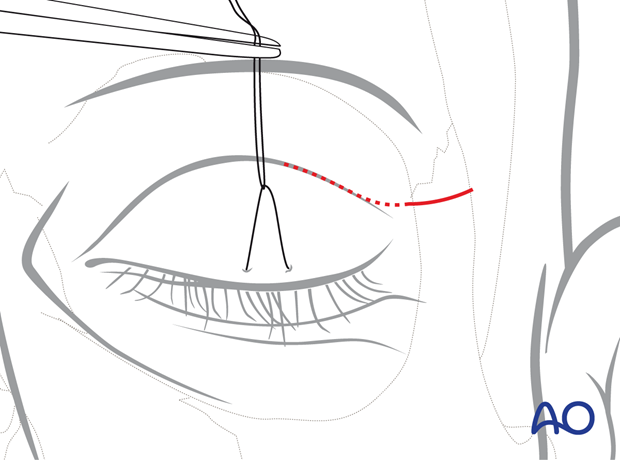
4. Identification and marking of incision line
The skin incision in the lateral (temporal) half of the upper lid is designed and marked in a curvilinear fashion, with the medial portion being convex superiorly and the lateral portion in line with the lateral canthus. Most appropriately, the incision is placed into a natural supratarsal skin crease.
If a lid fold is not detectable, the incision line is determined according to the measurements of the lower edge of a standard upper blepharoplasty: 10 mm above the canthus directly over the lateral orbital rim.
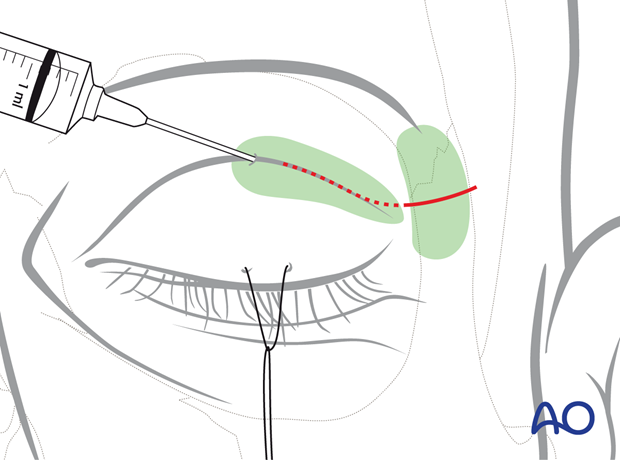
5. Vasoconstriction
The upper eyelid skin can be infiltrated with a mixture of local anesthesia and a vasoconstrictor in the supraperiosteal plane over the superolateral orbital rim to be surgically exposed. Adequate time for hemostasis must elapse before the procedure.
6. Skin incision and undermining of skin muscle flap
The upper eyelid incision is made using a # 5 scalpel blade in a medial to lateral direction under digital traction and light pressure of the skin. The skin may be transected with the orbicularis muscle or separately.
The illustration shows the position of the initial incision through the skin in a supratarsal fold and the underlying orbicularis oculi muscle.
Once the orbicularis muscle is exposed, a small slit is opened at the lateral wound corner to introduce scissors into the preseptal plane, and dissection proceeds medially underneath the muscle.
The orbicularis is divided, leaving the orbital septum intact.
7. Supraperiosteal dissection
The skin muscle flap is elevated from medial to lateral using scissors. The dissection finally arrives over the superolateral rim with exposure of the periosteum. Commonly in the lateral part of the dissection, the retroorbicularis oculi fat will prolapse.
The vasculature of the muscle provides for skin viability.
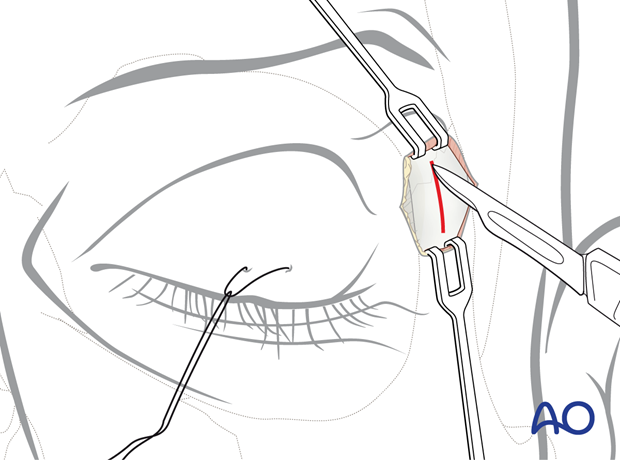
8. Periosteal incision
The periosteum is exposed and sharply incised with a scalpel along the middle of the frontozygomatic suture for a length of 1 cm.
The medial portion of the superolateral orbital rim and frontal process of the zygoma are exposed with a 1 cm periosteal incision over each
9. Subperiosteal dissection of the lateral orbital rim and lateral orbit
The underlying bony structures are exposed using sharp periosteal elevators.
The periosteum is reflected from the zygomaticofrontal area, and the fracture exposed.
Care is taken to avoid injury to the lacrimal gland.
10. Closure
The wound closure is performed in layers.
Muscle
The orbicularis oculi muscle is reapproximated with interrupted sutures. The muscle layer is closed meticulously with several interrupted sutures, particularly over the lateral orbital rim. This helps to prevent thinning of the soft tissues covering the fixation hardware.
Skin
The cutaneous closure is made with an interrupted or running suture, including the skin edges and the underlying orbicularis oculi muscle.