Open treatment
1. General consideration
Pediatric orbital roof fractures should be followed closely due to growth.
Unlike in the adult population, nondisplaced orbital roof fractures in pediatric patients should be followed up regularly due to the skull growth and dural pulsations that may lead to bone resorption. These nondisplaced linear fractures may ultimately become growing skull fractures that would require surgical intervention.
Displaced fractures may compromise globe position and movement. These fractures should be reduced, and the orbit should be reconstructed with material that will withstand dural pulsation and bone resorption (alloplastic reconstruction).
2. Approach
The surgical approach is the same as in adults.
Exposure of orbital roof fractures is performed most commonly via coronal approach, via preexisting lacerations, and upper blepharoplasty incisions.
Once the orbital roof is exposed, periorbital dissection is meticulously performed.
Care should be taken at the superior-posterior medial aspect where the optic nerve and the superior oblique muscles can be found.
3. Surgical treatment
Surgical treatment is performed as in the adult section.
4. Case example
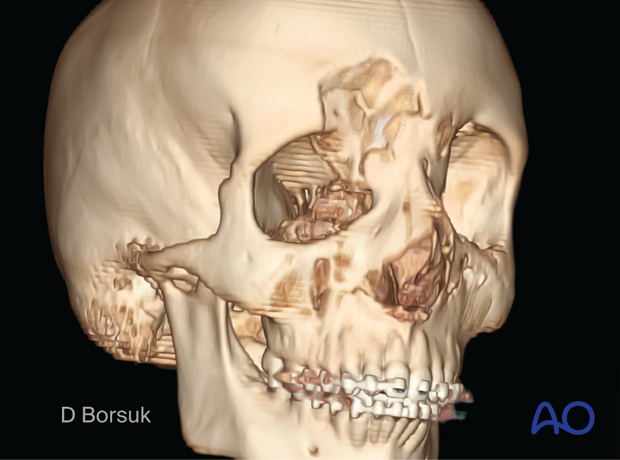
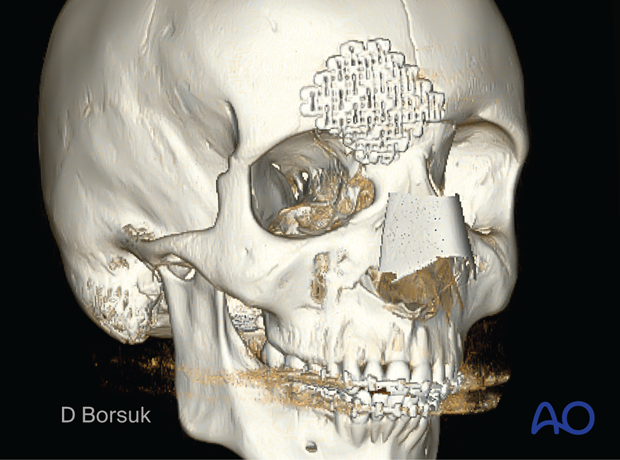
16-year-old boy with right orbital roof and frontal bone fracture.
The clinical examination demonstrates an inferior and lateral (down and out) position of his right globe. This presentation can be observed with an orbital roof fracture that compresses the orbital contents.

CT scan of the same patient demonstrating the intraorbital displacement of the orbital roof fracture.
A coronal incision was used to reduce and reconstruct the orbital roof. The normal anatomy is maintained with a titanium mesh, which withstands the dural pulsations and reduces the risk of bony resorption.
5. Aftercare
Patient vision is evaluated as soon as awakening from anesthesia and then at regular intervals until hospital discharge.
A swinging flashlight test may serve to confirm pupillary response to light in the unconscious or non-cooperative patient; alternatively, an electrophysiological examination while possible is seldom available in the operation area.
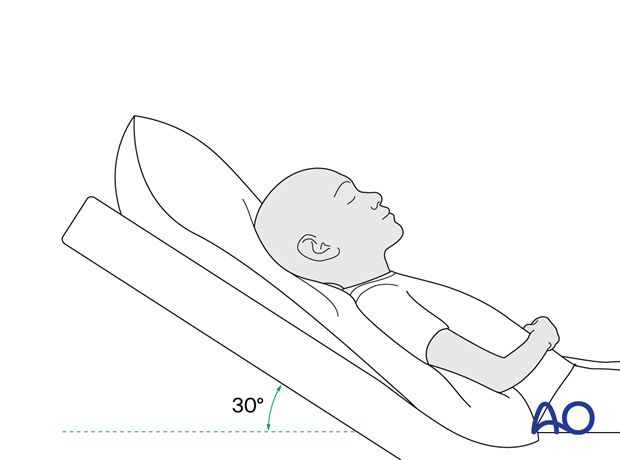
Postoperative positioning
Keeping the patient’s head in an upright position both preoperatively and postoperatively may significantly improve periorbital edema and pain.
Nose blowing
Nose blowing should be avoided for at least ten days following orbital fracture repair to prevent orbital emphysema.
Medication
The use of the following perioperative medication is controversial. There is little evidence to make solid recommendations for postoperative care.
- No aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs) prescribed for seven days.
- Provide analgesia as necessary.
- Antibiotics (many surgeons use perioperative antibiotics. There is no clear advantage of any antibiotic, and the recommended duration of treatment is debatable.)
- A nasal decongestant may be helpful for symptomatic improvement in some patients.
- Steroids, in cases of severe orbital trauma, may help with postoperative edema. Some surgeons have noted increased complications with perioperative steroids.
- Ophthalmic ointment should follow local and approved protocol. This is not generally required in the case of periorbital edema. Some surgeons prefer it. Some ointments have been found to cause significant conjunctival irritation.
Ophthalmological examination
Postoperative examination by an ophthalmologist may be requested. The following signs and symptoms are usually evaluated:
- Vision (except for alveolar ridge fracture, palatal fracture)
- Extraocular motion (motility) (except alveolar ridge fracture, palatal fracture)
- Diplopia (except Le Fort I, alveolar ridge fracture, palatal fracture)
- Globe position (except Le Fort I, alveolar ridge fracture, palatal fracture)
- Perimetric examination (except Le Fort I, alveolar ridge fracture, palatal fracture)
- Lid position
- If the patient complains of epiphora (tear overflow), the lacrimal duct must be checked.
Postoperative imaging
Postoperative imaging has to be performed within the first days after surgery. 3D imaging (CT, cone beam) is recommended to assess complex fracture reductions. An exception may be made for centers capable of intraoperative imaging.
Wound care
Ice packs are effective in the short term to minimize edema.
Remove the sutures from the skin after approximately five days if non-resorbable sutures have been used.
Avoid sun exposure and tanning to skin incisions for several months.
Clinical follow-up
Clinical follow-up depends on the complexity of the surgery and whether the patient has any postoperative problems.
With patients having fracture patterns including periorbital trauma, issues to consider are the following:
- Globe position
- Double vision
- Other vision problems
Other issues to consider are:
- Facial deformity (incl. asymmetry)
- Sensory nerve compromise
- Problems of scar formation
Eye movement exercises
Following orbital fractures, eye movement exercises should be considered.
Implant removal
Generally, orbital implant removal is not necessary except in the event of infection or exposure.
Follow-up
Follow-up should be performed to monitor healing and vision.
Special considerations for orbital fractures
Travel in commercial airlines is permitted following orbital fractures. Commercial airlines pressurize their cabins. Mild pain on descent may be noticed.
No scuba diving should be permitted for at least six weeks.
Children who participate in sports should consider wearing eye protection for the first three months following the fracture.













