Plate fixation
1. Principles/General considerations
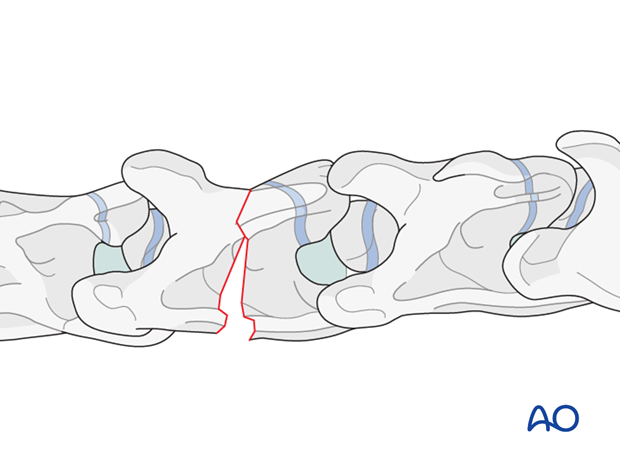
Compression fractures of the vertebral body may be associated with articular process fractures.
Vertebral body
Fractures of the vertebral body can be stabilized with plates. The goal of surgery is to provide decompression at the fracture site by realigning the vertebrae and providing stability with some form of fixation.
If more than one vertebra is affected, intervertebral fusion is attempted during the fixation of the fracture.
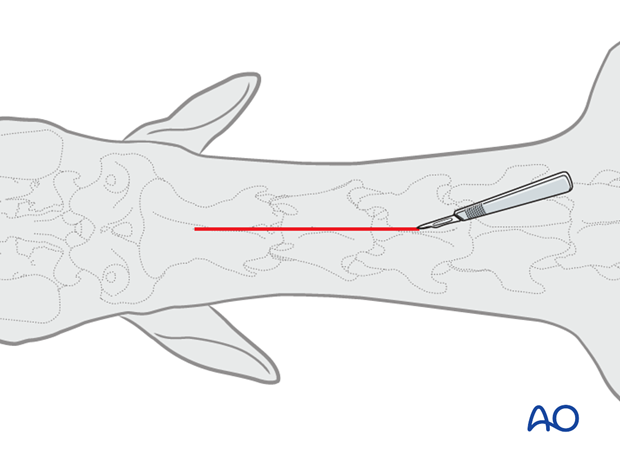
2. Preparation and approach
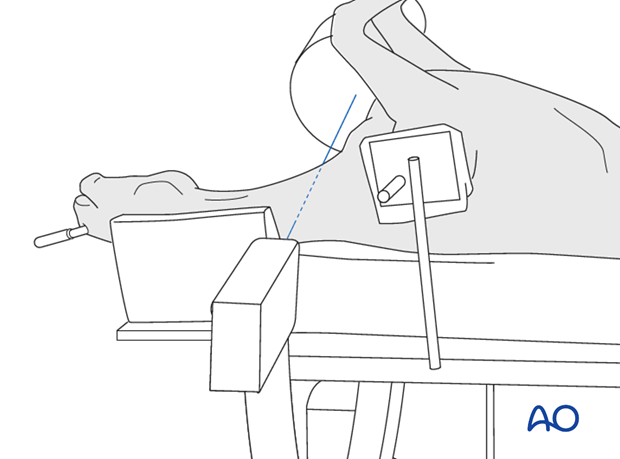
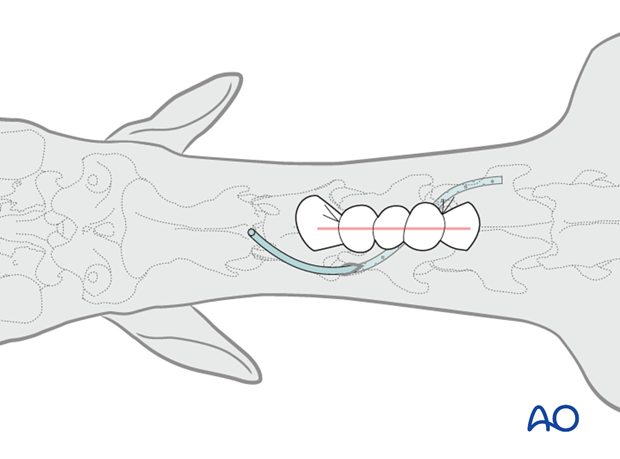
This procedure is performed with the patient positioned in dorsal recumbency through the ventral midline approach to the cervical spine.
3. Reduction
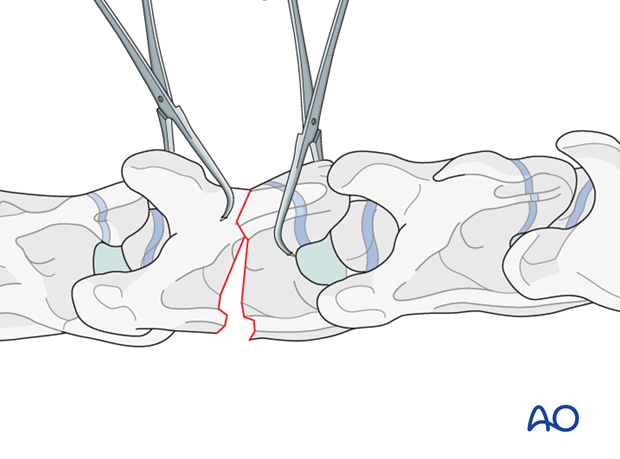
Reduction with only one vertebra affected
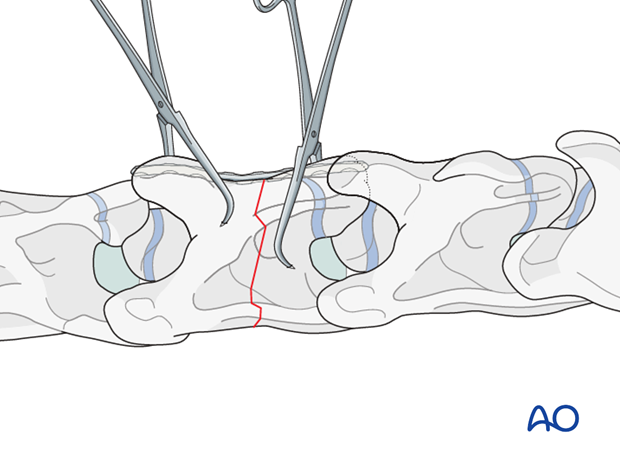
After exposing the ventral surface of the vertebra, the alignment is corrected and maintained with pointed reduction forceps.
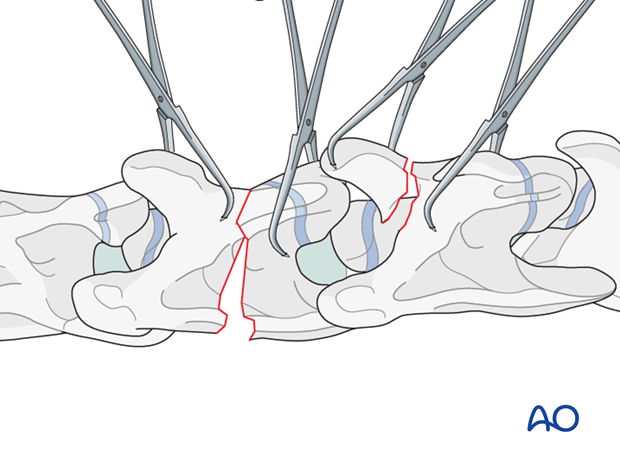
Reduction with more than one vertebra affected
4. Fixation
Plate selection
Either (a) locking compression plate (LCP) or (b) dynamic compression plate (DCP) is used for fracture fixation of the vertebrae. According to the size of the patient, a small or broad 3.5-4.5 mm DCP or 3.5/4.0 or 4.5/5.0mm LCP is used.
Pearl: Advantages of the LCP over the DCP:
- The plate does not have to be accurately contoured to the bone surface; therefore less bone from the ventral spine needs to be removed in preparation for plate application.
- Locking the screws to the plate provides a more stable fixation.
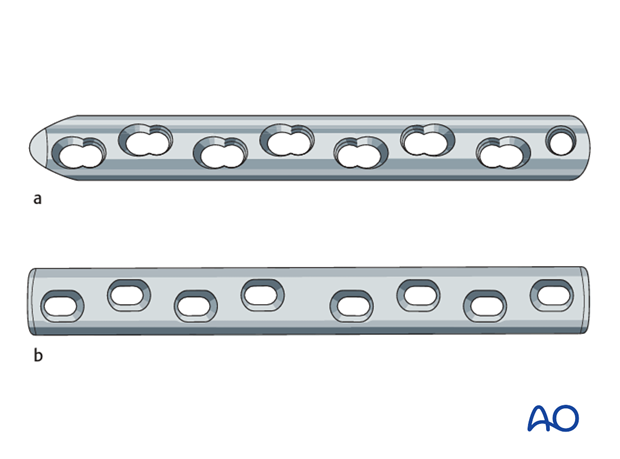
Plate preparation
Minimal plate contouring is needed.
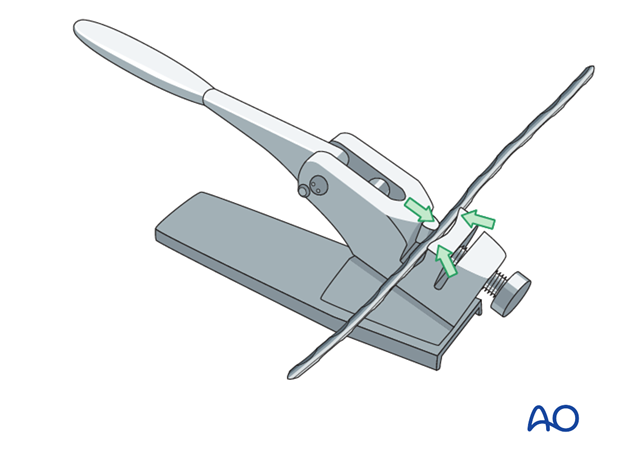
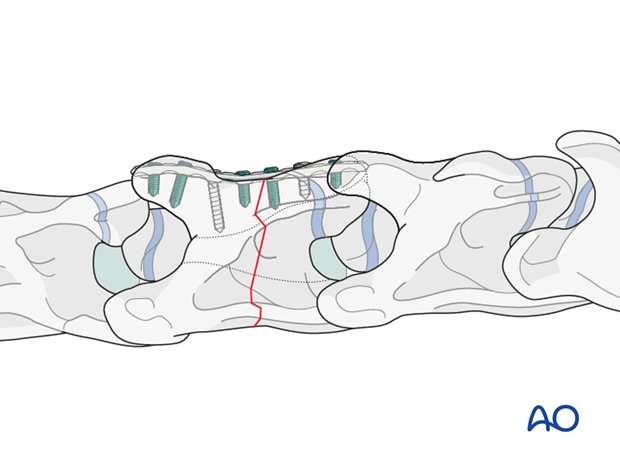
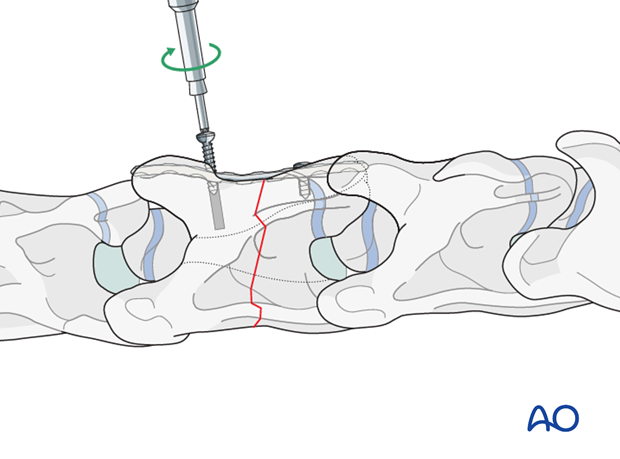
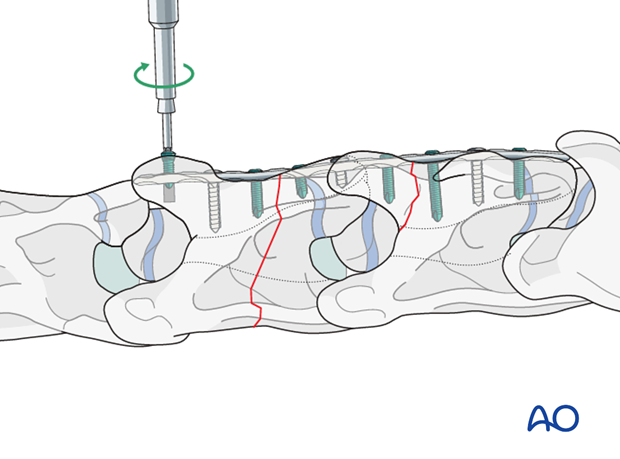
Plate application if only one vertebra is affected
With the reduction forceps in position, the appropriately sized plate is applied to the ventral aspect of the vertebra. The plate should be as long as possible to achieve better stabilization.
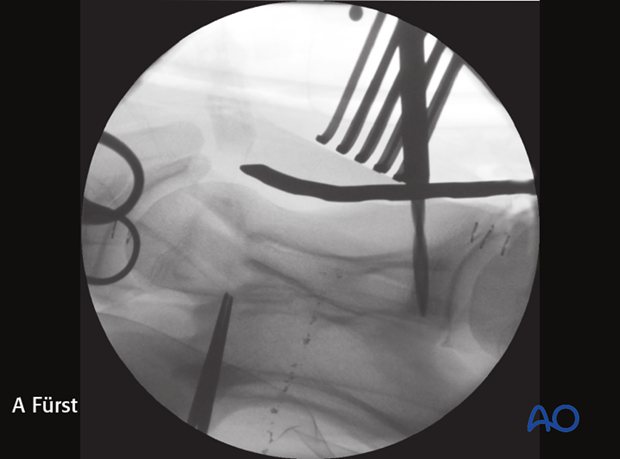
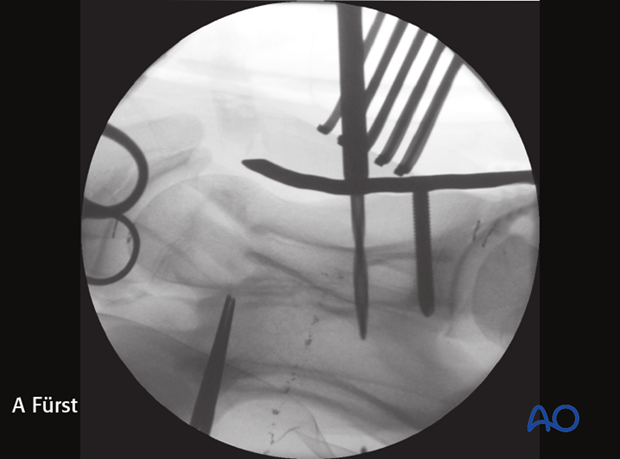
Intraoperative radiographic control of the drilling depth and screw positioning is critical to prevent penetration of the vertebral canal.
The image shows intraoperative radiographic control of the drilling depth and screw positioning.
Note: Penetration of the spinal canal with the drill must be avoided.
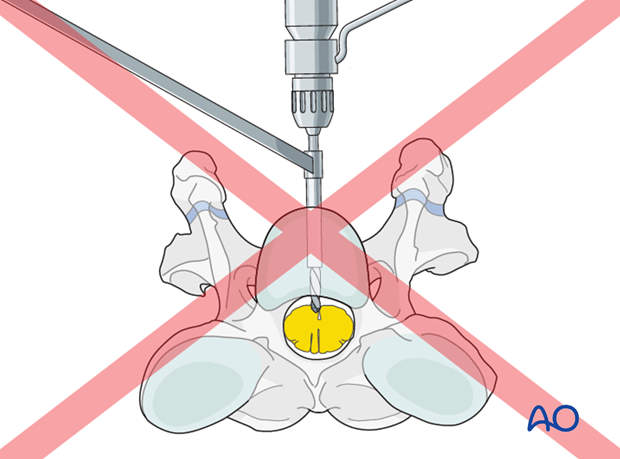
Intraoperative image showing penetration of the spinal canal.
Cortex screws are used in lag fashion on both sides of the fracture to compress the fragments. The correct length of the screws is determined with the help of fluoroscopy.
Note: Attention must be paid not to damage the spinal cord.
Note: It is difficult to get a secure screw purchase in vertebral bone, particularly in foals, because of the thin vertebral cortex .
The remaining holes are filled with locking-head screws.
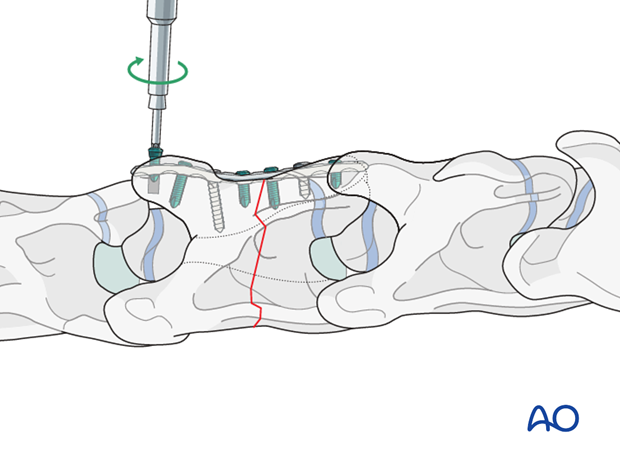
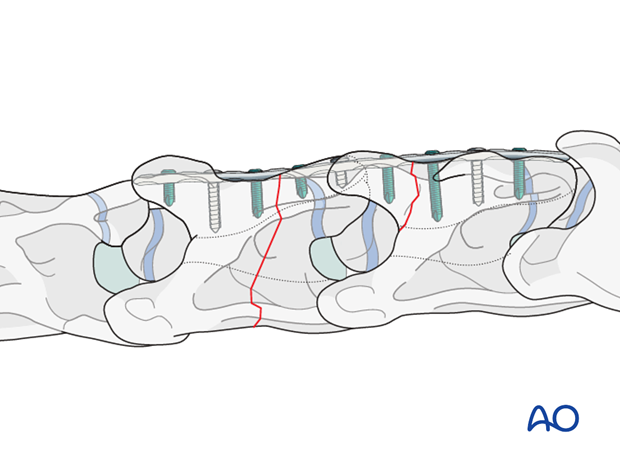
Plate application if more than one vertebra is affected
Cortex screws are used in lag fashion on both sides of the fracture to compress the fragments. The length of the screws is determined with the help of fluoroscopy.
Note: Attention must be paid not to damage the spinal cord.
Note: It is difficult to get a secure screw purchase in vertebral bone, particularly in foals, due to the thin cortex of the vertebrae.
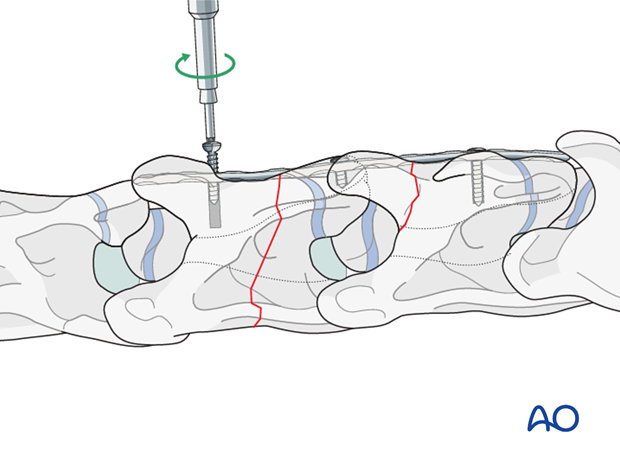
The remaining holes are filled with locking-head screws.
5. Closure
The muscles, subcutaneous tissue, and the skin were closed in a continuous fashion. A close active drain can be placed at the level of the plate, exiting the skin near the incision and sutured to the skin.
A stent bandage is applied, and covered with an adhesive barrier drape to keep the incision clean and dry during recovery.
6. Aftercare
Following surgery, antibiotics and NSAIDs are routinely administered for 3 days. If indicated, they need to be continued.
Routinely follow up radiographs are taken immediately after surgery and after 2 and 4 months.
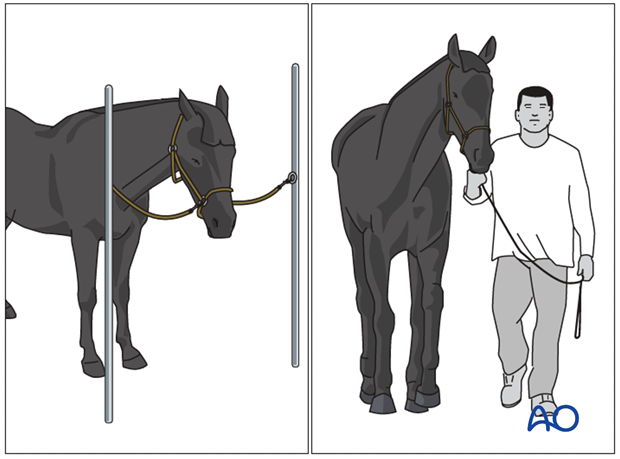
The rehabilitation protocol includes 2 months of stall confinement, followed by 1 month of hand-walking, and 2 months of progressive exercise.
Only when the ataxia has completely disappeared, the horse can return to training or other activities.
Implant removal
There is no need for implant removal, except in cases of implant loosening or surgical site infection.













