Plate fixation (dorsally)
1. Principles/General considerations
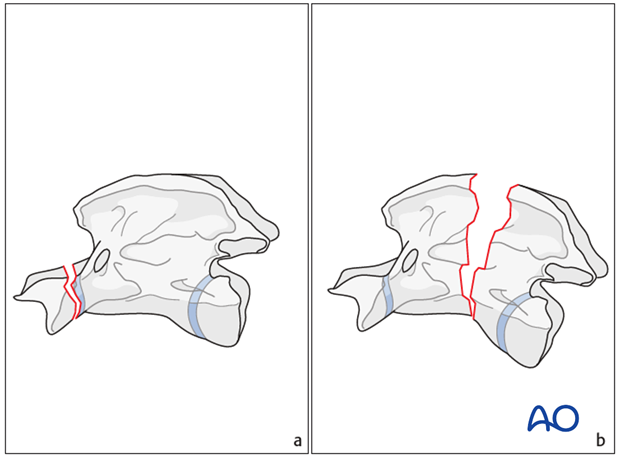
Fractures of C2 (Axis) can occur in the axial dens (a) or the axial body (b), with or without involvement of the spinal canal.
Axial body
Fractures of the axial body are stabilized with plates. The goal of surgery is to provide decompression at the fracture site by realigning the vertebrae and providing stability with some form of fixation.
2. Preparation and approach
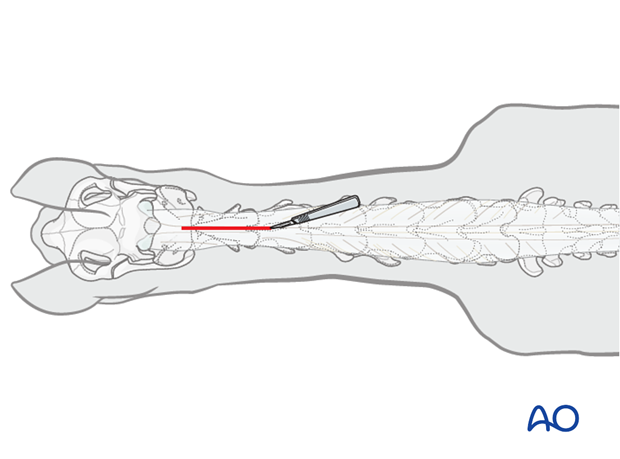
This procedure is performed with the patient positioned in sternal recumbency through the dorsal midline approach to the cervical spine.
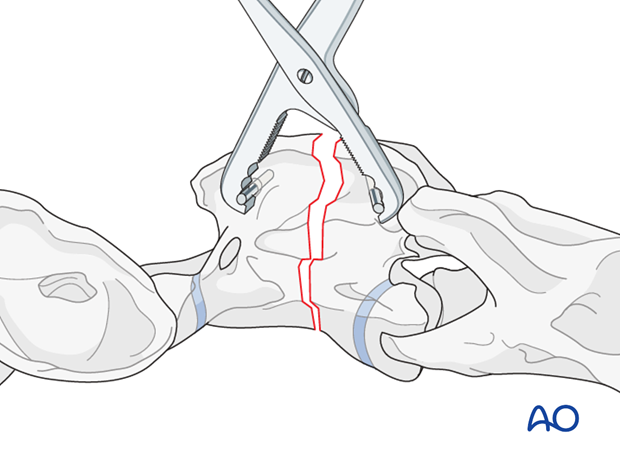
3. Reduction
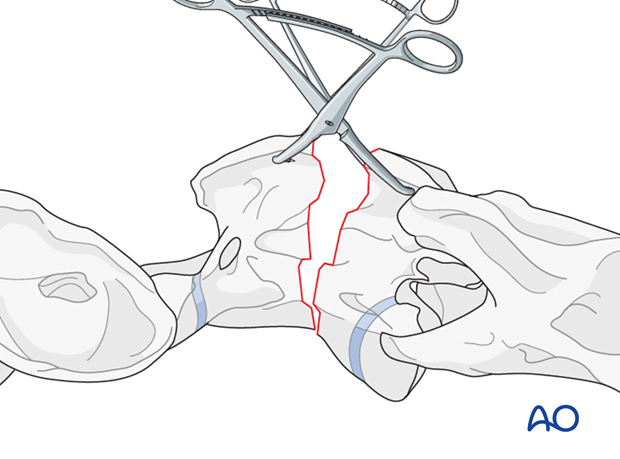
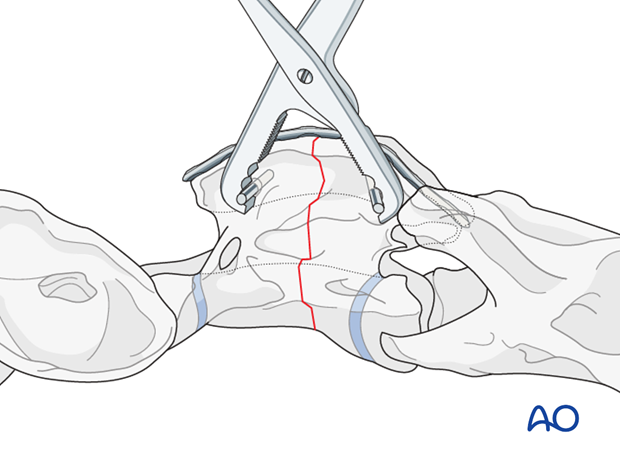
After exposing the dorsal surfaces of the atlas and axis, the alignment of the vertebrae is corrected and maintained with bone-holding forceps.
Steinmann pins are inserted in horizontal direction into the cranial and caudal fragment to facilitate the reduction
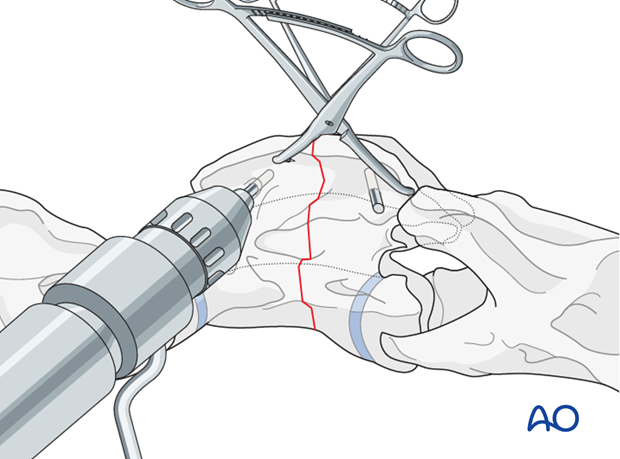
Pearl: Large bone-holding forceps and a large bone clamp can facilitate the reduction of the fracture.
4. Fixation
Plate selection
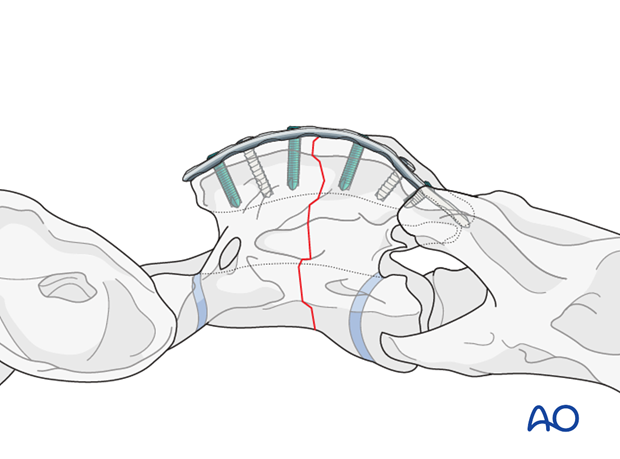
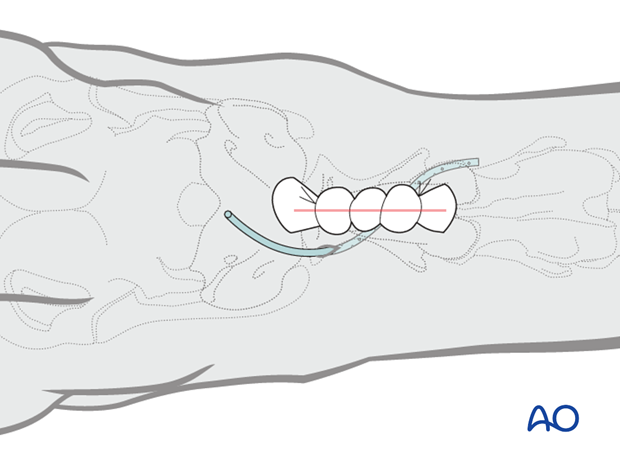
The use of the locking compression plate (LCP) is preferred for fracture fixation of the vertebrae. According to the size of the patient, a small or broad 3.5/4.0 or 4.5/5.0mm LCP is used.
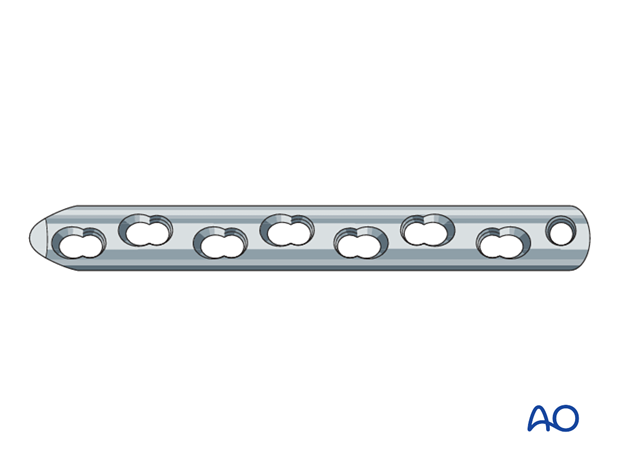
Plate preparation
Plate contouring is needed to fit the anatomical shape of the vertebra.
Accurate contouring of locking compression plates is not necessary, but it improves the closure of the soft tissue over the plate.
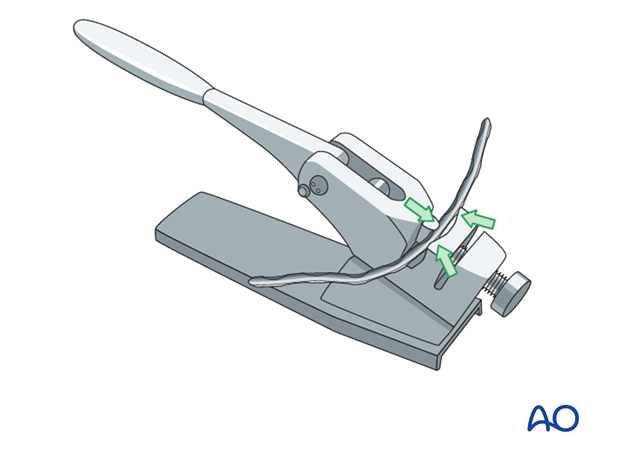
Plate application
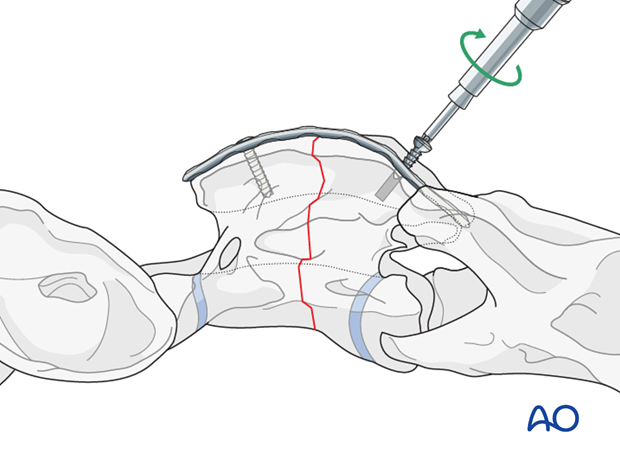
With the reduction forceps in position, the appropriately sized plate is applied on the dorsal spinous process.
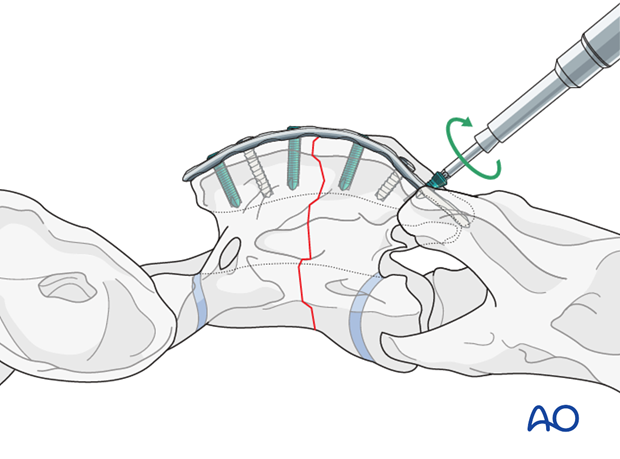
One cortex screw is inserted into each fragment in load fashion. The correct length of the screws is determined with the help of fluoroscopy.
The remaining holes are filled with locking-head screws.
5. Closure
One deep layer under the nuchal ligament, the nuchal ligament, and the subcutaneous tissue are closed in layers with simple continuous patterns. The skin is closed with staples. A stent bandage is applied and covered with an adhesive barrier drape to keep the incision clean and dry during recovery.
6. Case example
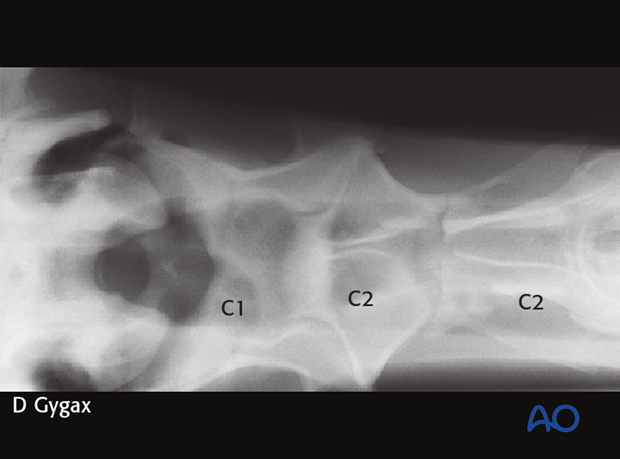
A 7-year-old Warmblood gelding was admitted with a 3-week history of neck stiffness. The horse had an acute onset of neck stiffness with no known trauma. According to the owner, the horse had initial mild signs of ataxia and weakness in the hind limbs.
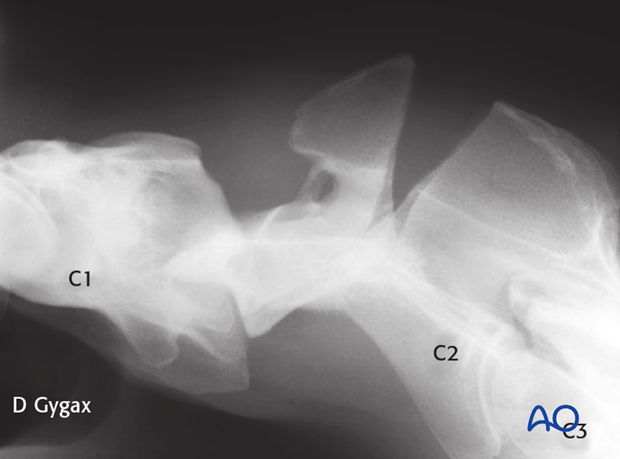
Marked swelling was detectable in the proximal third of the neck at the level of the second cervical vertebra (C2).
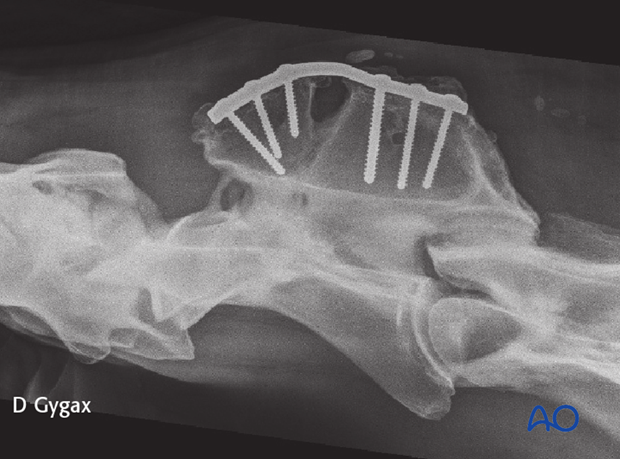
The fracture was repaired using a 7-hole 4.5mm DCP. Optimal positioning of the plate and the length of the screws were facilitated by fluoroscopy.
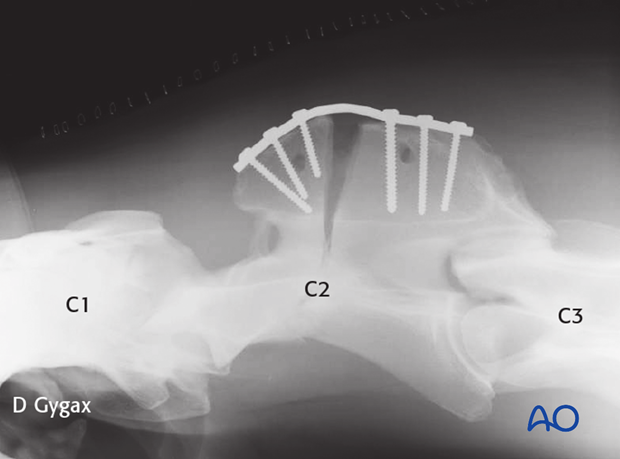
The horse had an excellent outcome with complete healing of the main vertebral body and returned to its previous activity level.
7. Aftercare
Following surgery, antibiotics and NSAIDs are routinely administered for 3 days. If indicated, they need to be continued.
Routinely follow up radiographs are taken immediately after surgery and after 2 and 4 months.
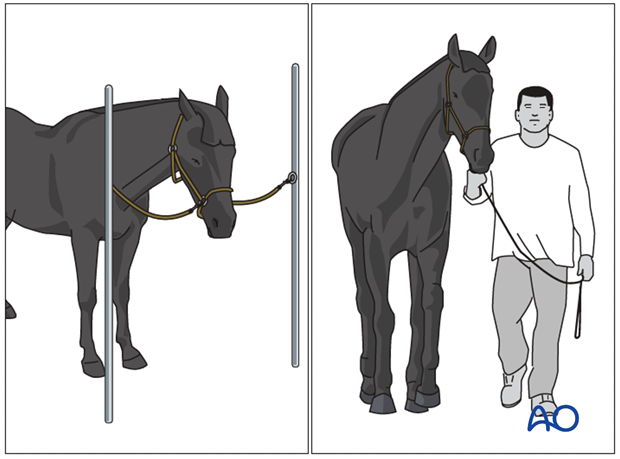
The rehabilitation protocol includes 2 months of stall confinement, followed by 1 month of hand-walking, and 2 months of progressive exercise.
Only when the ataxia has completely disappeared, the horse can return to training or other activities.
Implant removal
There is no need for implant removal, except in cases of implant loosening or surgical site infection.













