Transcondylar lag screw and bridging plate
1. Principles
Anatomic reconstruction of the joint surface is essential, and this step should be performed prior to fixation of the condyles to metaphysis.
Interfragmentary compression is achieved with a lag screw for anatomical reduction of the major fragments articular fracture. Smaller fragments may be stabilized with additional lag screws or K-wires.
Proper alignment of the femur must be obtained with special attention to angulation and torsion.
Comparison with the contralateral unaffected bone can be useful.
2. Positioning and approach
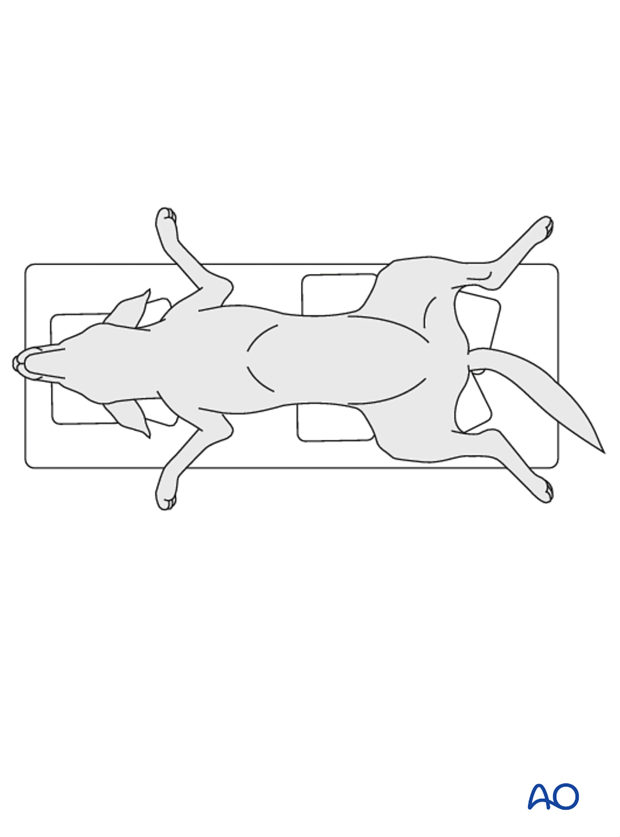
This procedure is performed with the patient placed in dorsal recumbency
One of the following approaches is utilized:
3. Surgical technique
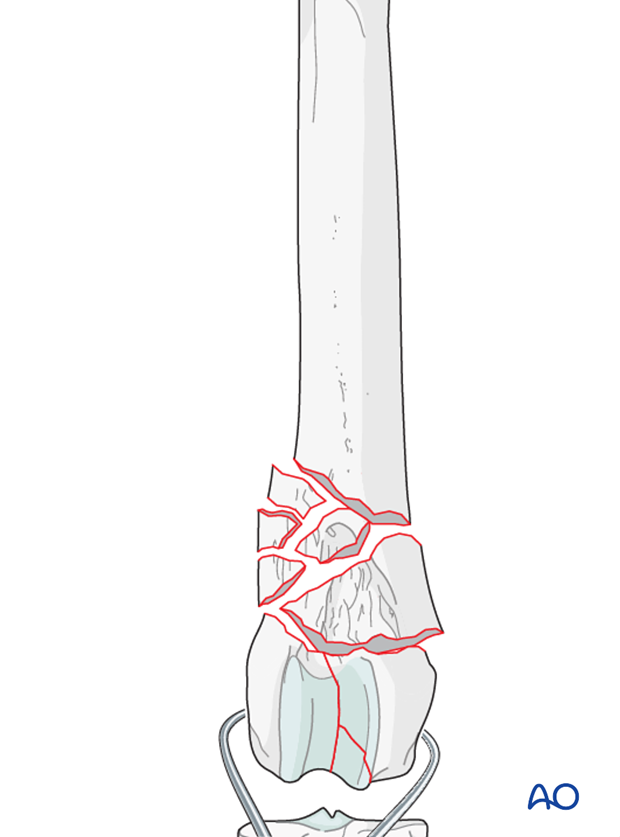
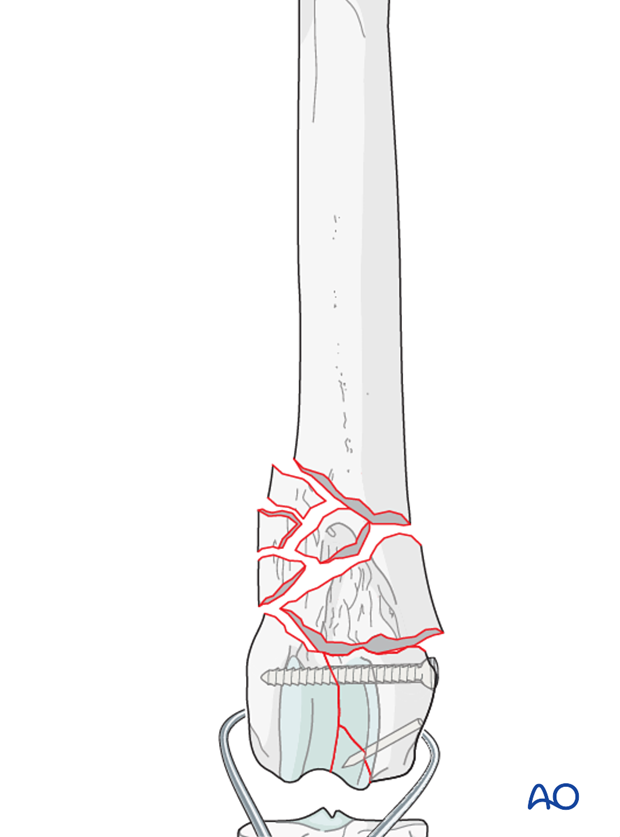
Reduction and stabilization of the femoral condyles
The articular fractures of the condyles are reduced with pointed reduction forceps. Anatomic reduction is essential in all cases.
Note: Bone in juvenile patients is very soft. Care must be taken not to damage it during reduction.
Note: It is important to try to reduce all fractures prior to placement of the first lag screw. Temporary stabilization of these fragments may be performed with K-wires.
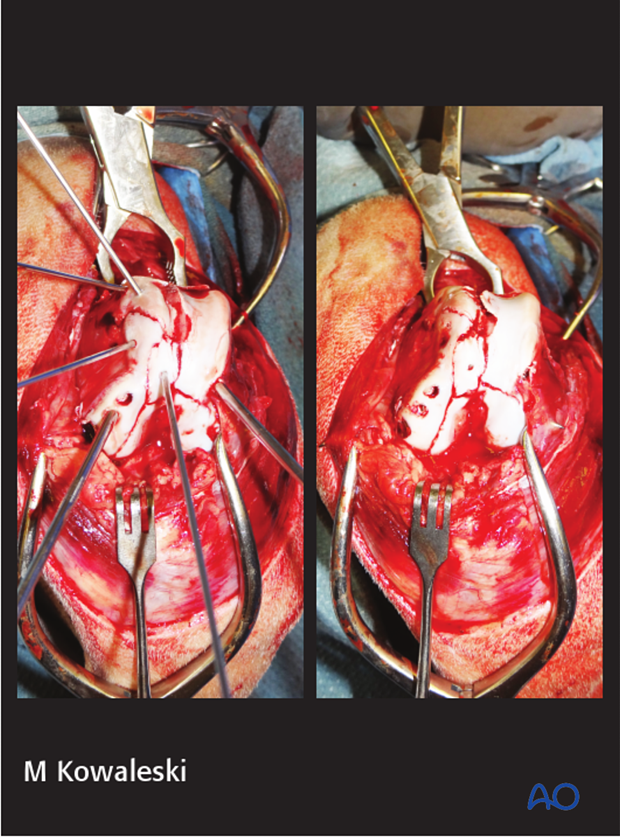
Stabilization is achieved with inserting a lag screw across the condyles perpendicular to the fracture plane. Frequently the screw is placed in lateral to medial direction, starting at the level of the epicondyle.
Note: Care should be taken not to penetrate the articular surface with the screws or K-wires. Do not penetrate condylar fossa to avoid damage to the cruciate ligaments with the screw.
A detailed description of "Lag screw fixation" can be found here.
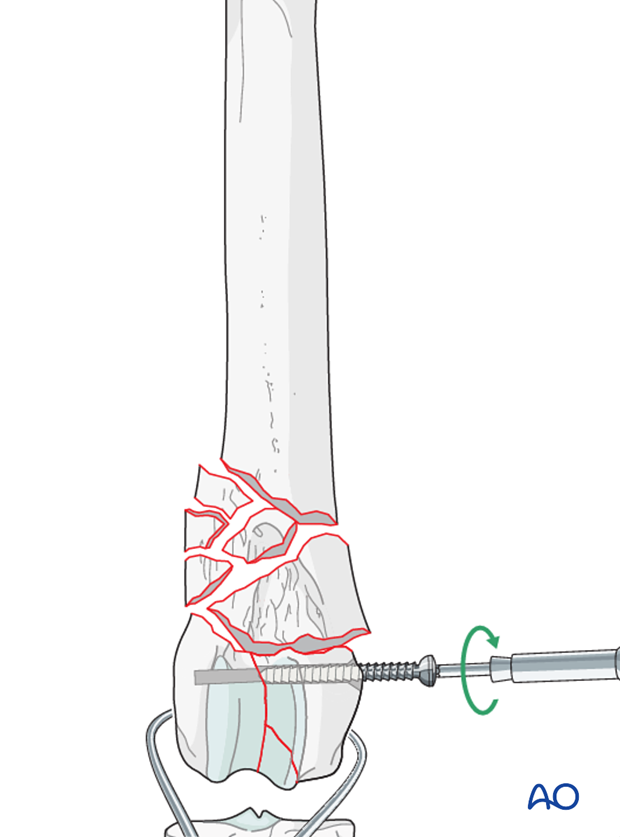
Definitive stabilization of the smaller fragments of the condyles may be performed using lag screws or K-wires.
Note: If the screw head or K-wire is positioned in the articular surface they must be countersunk to avoid interference with intraarticular structures.
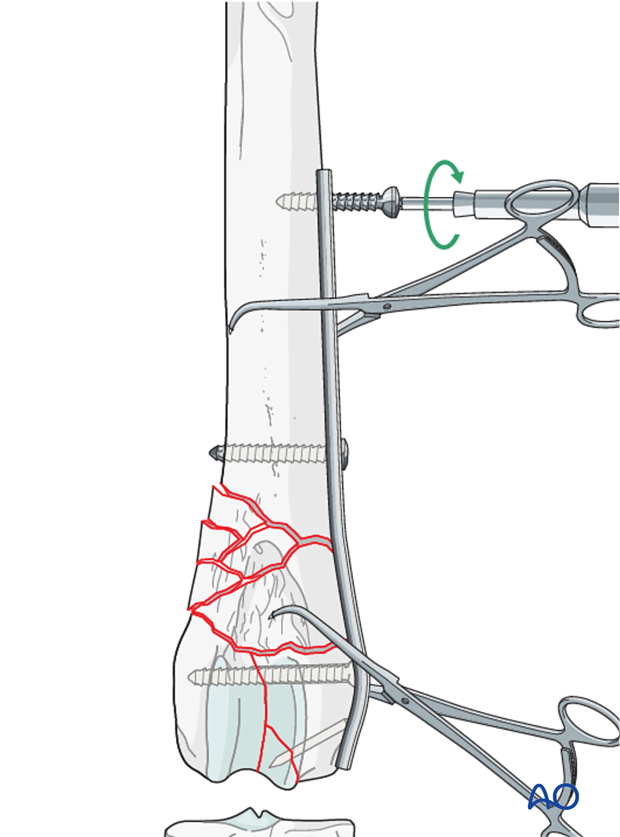
Reduction and stabilization of the femoral metaphysis
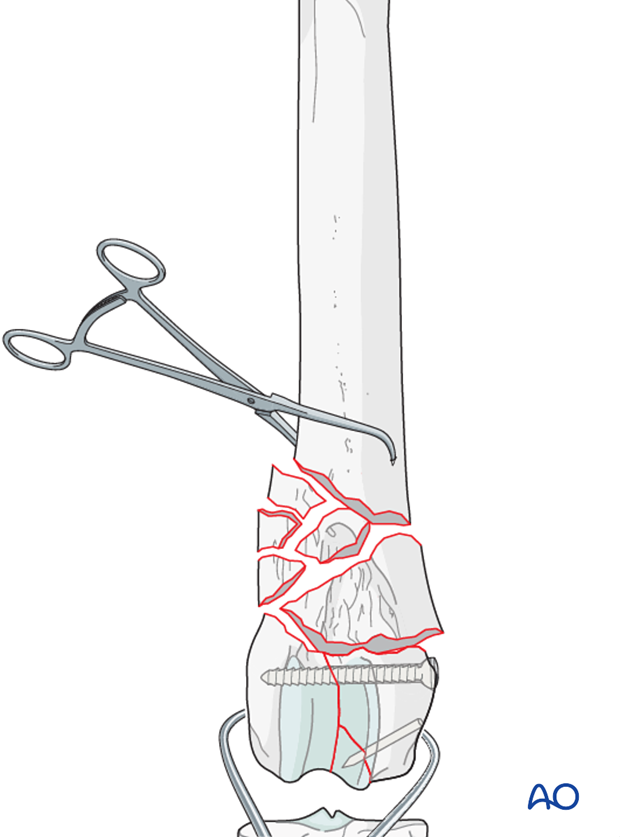
Bone holding forceps are applied to the proximal and distal major fragments for distraction.
Indirect reduction is achieved by distracting and aligning the major bone segments using bone clamps, or traction on the femoral condyles.
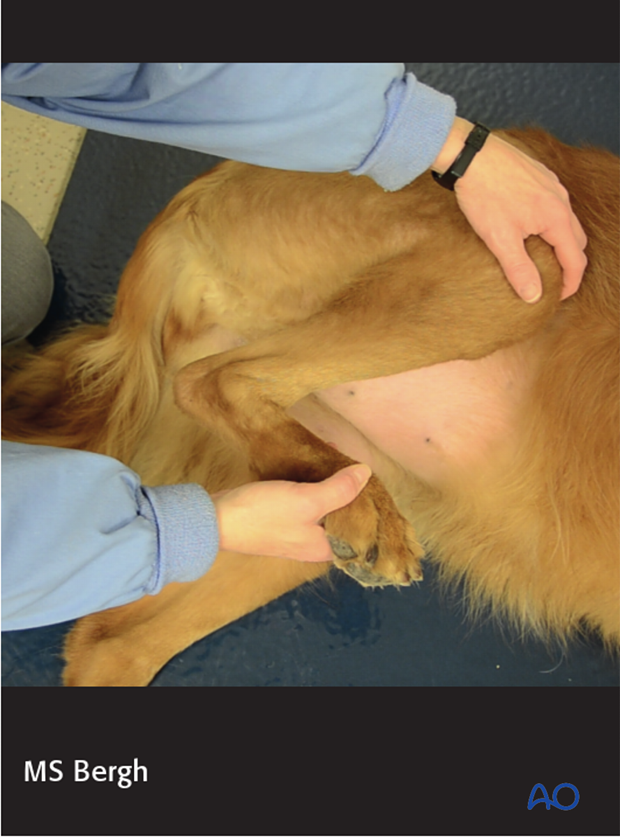
Validation of alignment and rotation
Once the bone length has been restored, it is necessary to check for correct alignment and rotation. Rotational alignment can be judged by palpation or by direct visualization of the greater trochanter and femoral trochlea. The distal part of the femur is held in a true lateral position. The position of the greater trochanter and alignment of the adductor magnus muscle are then inspected.
If the femur is correctly aligned in the axial plane the adductor magnus muscle should be aligned and the greater trochanter should be slightly caudal to the long axis of the bone.
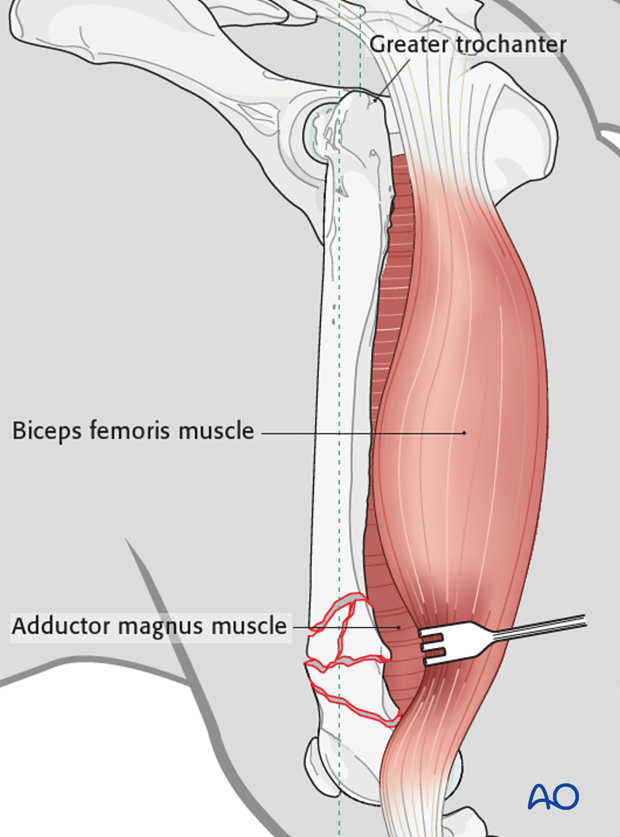
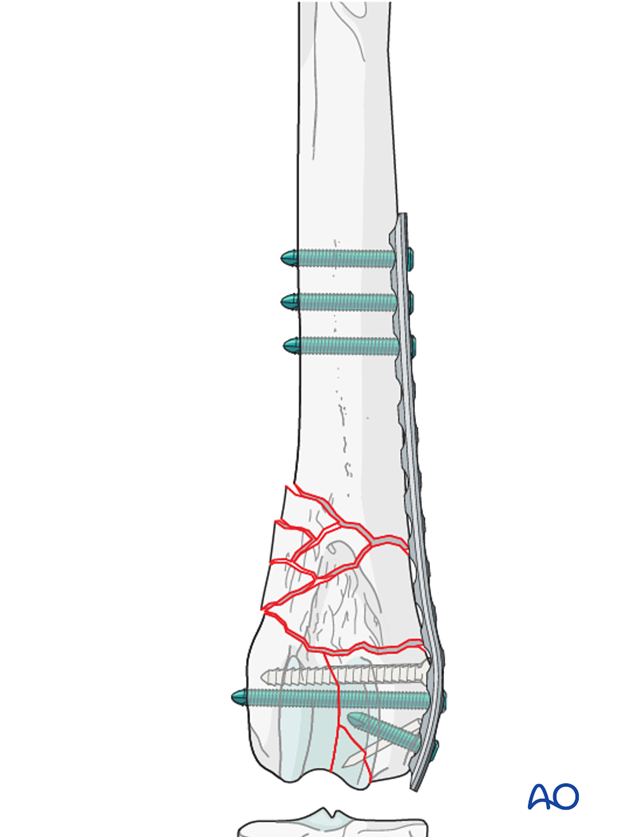
Plate selection
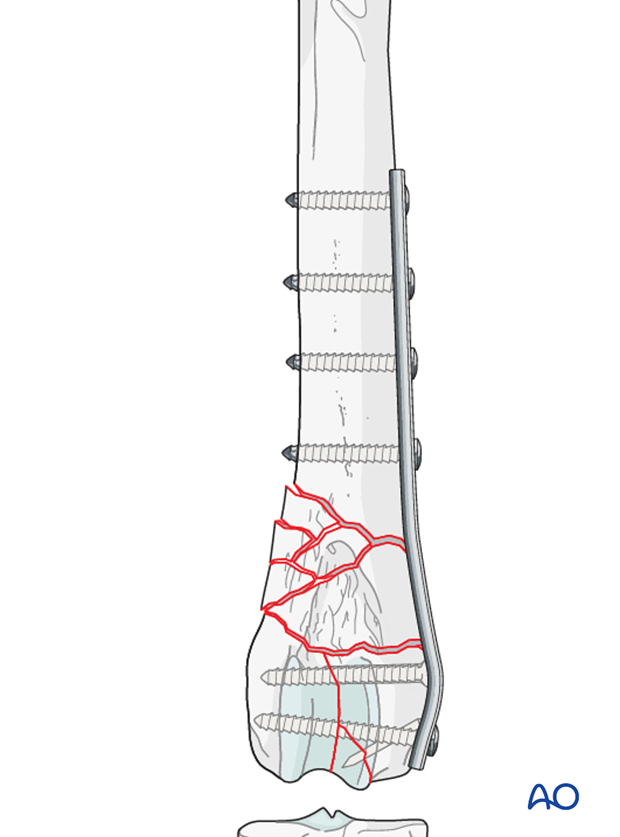
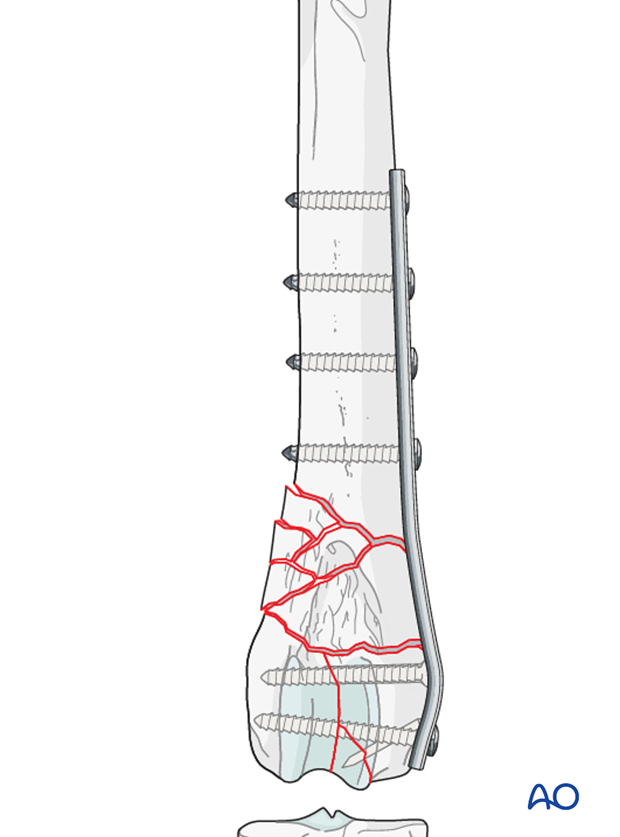
Numerous plate types can be used such as the reconstruction plate. Other specially designed plates for the distal femur are available.
Ideally the plate should be long enough to place at least three screws in either side of the fracture. In the distal femur the use of only two screws in the distal fragment is acceptable.
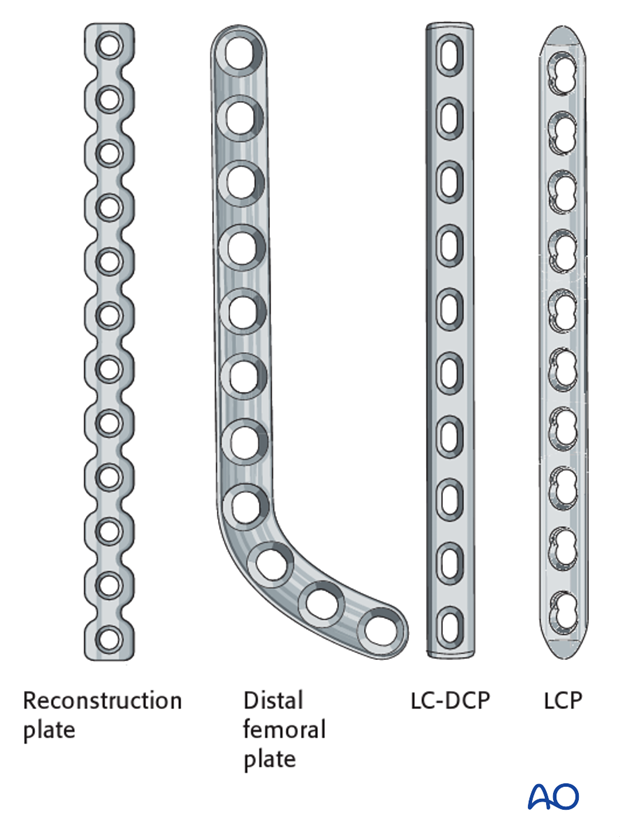
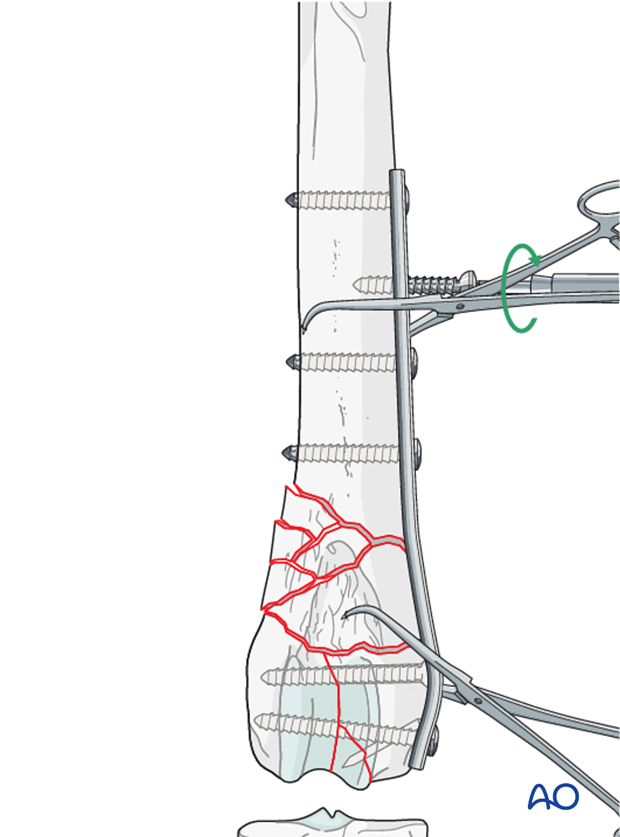
Plate placement
The plate is contoured to the lateral aspect of the distal femur. The plate position and contouring to the bone is checked thoroughly and adjusted, if required.
Note: The plate should be contoured so the distal holes are positioned away from the lag screw.
Note: Care should be taken to avoid placement of the plate high on the lateral trochlear ridge, where it can impinge on patellar tracking and result in pain and discomfort.
A detailed description of "Plate preparation" can be found here.
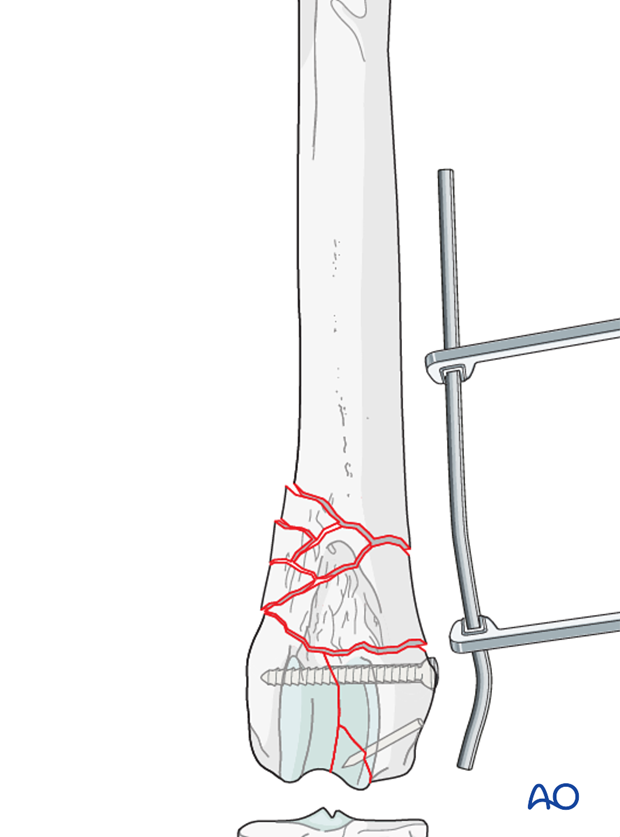
Plate fixation
Screws are placed in a near-near far-far pattern. Limb alignment is reassessed.
The remaining screw holes are filled. If a screw holes lays over the fracture plane it should be left open.
Note: Care should be taken to avoid penetrating the articular surface with the screws. Where possible at least one screw should traverse both condyles.
Fixation with a locking plate
If a locking plate is used, only 2-3 locking bicortical screws are needed per main fragment. One advantage of using a locking plate is that precise contouring is not necessary. Great care must be taken when contouring the distal part of the locking plate to avoid directing screws into the joint.
Note: If a combination of cortex and locking screws is used, the plate must be anatomically contoured at the sites of non-locking screw insertion. The non-locking screws must be inserted and tightened before any locking screws are placed.
Validation of fixation
Postoperative radiographs should be taken to assess the repair.
4. Case example C3
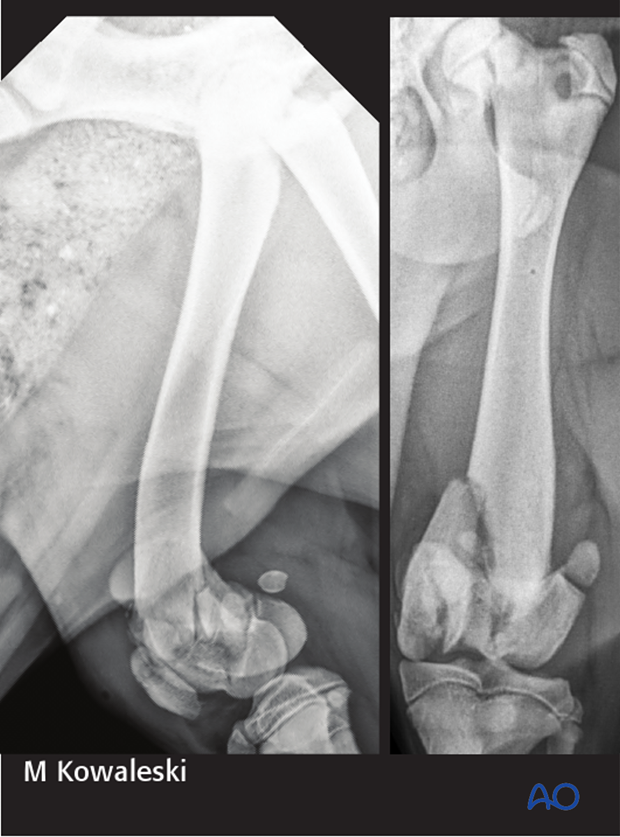
5-month-old Labrador retriever presented for left pelvic limb lameness after jumping out of the window of a moving car, with a 33-C3 fracture of the distal femur, a transverse fracture of the patella, and a 31-B2 fracture.
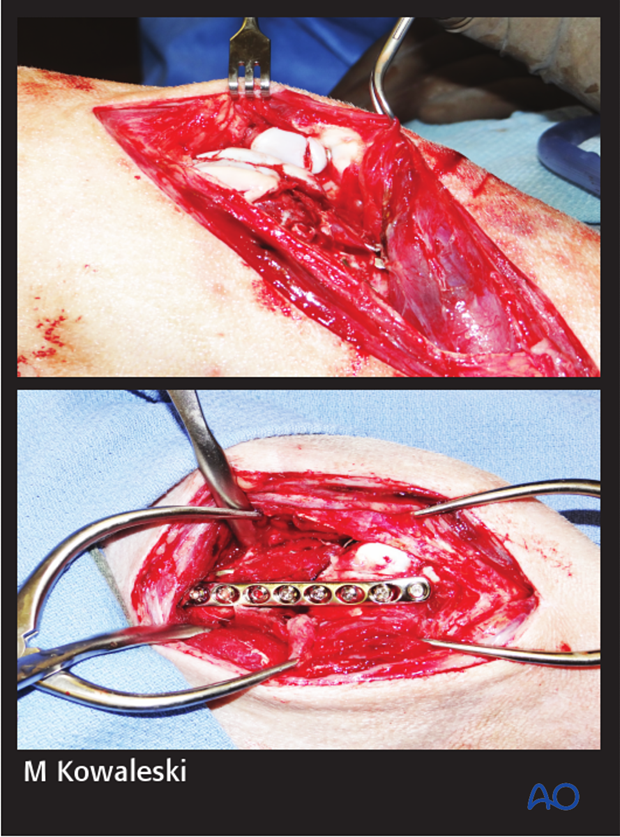
The fracture was approached initially through a lateral parapatellar approach and the articular fractures were visible.
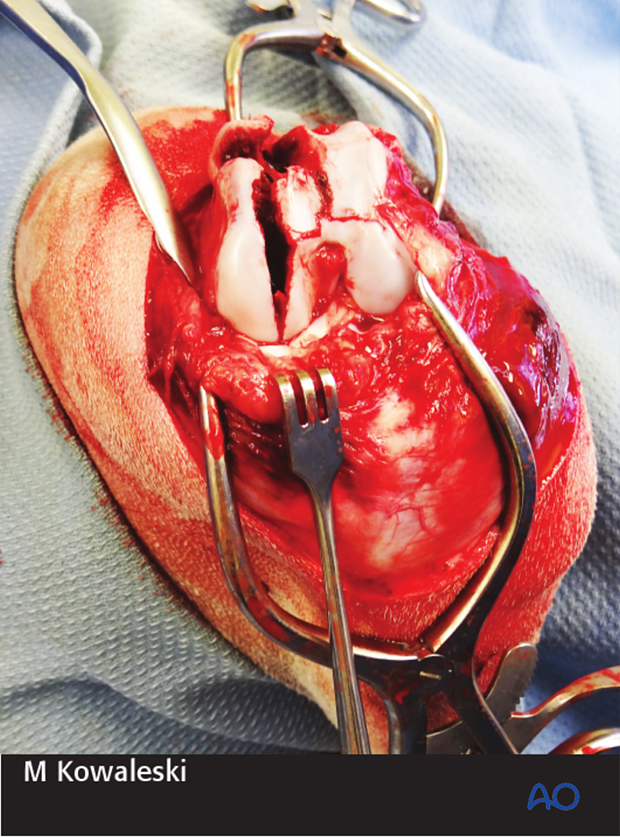
The articular fractures were repaired first using a combination of smooth pins and screws. The implants were countersunk below the articular surface.
A lateral parapatellar arthrotomy was then performed for repair of the patellar fracture with a pin and tension band fixation and bridging plate application on the distal femur with a LC-DCP.
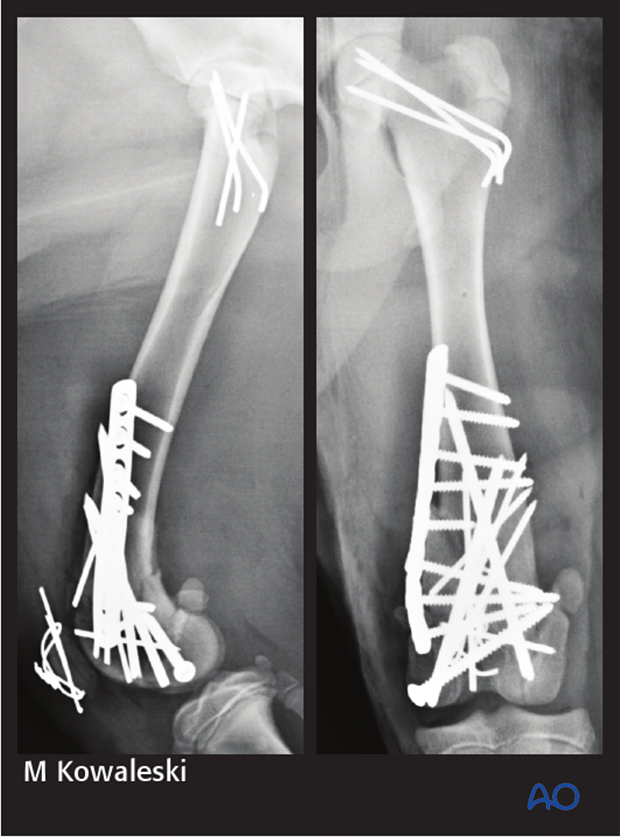
Post-operative radiographs demonstrate good alignment after fracture repair using a combination of screws, pins, and a bridging plate. The patellar fracture was repaired with a pin and tension band technique. The 31-B2 fracture was repaired with smooth pins.
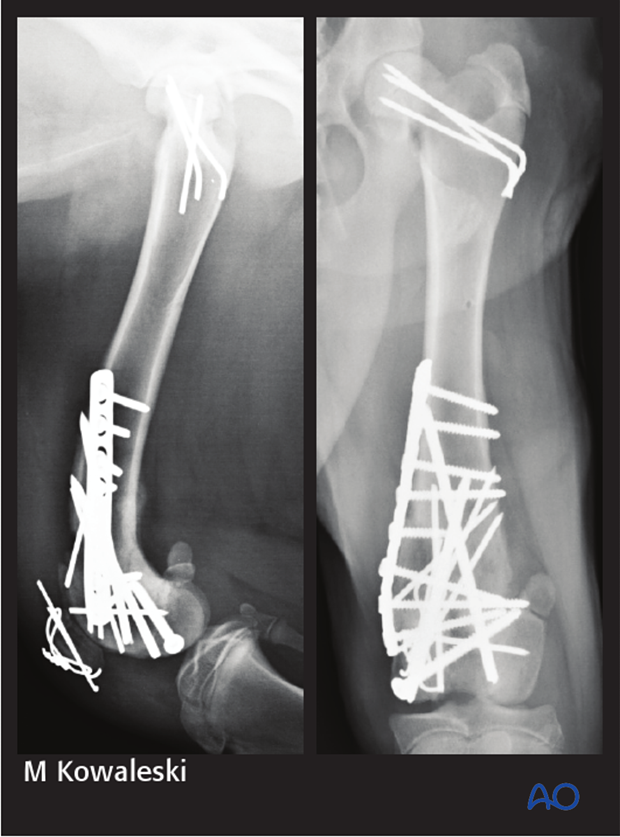
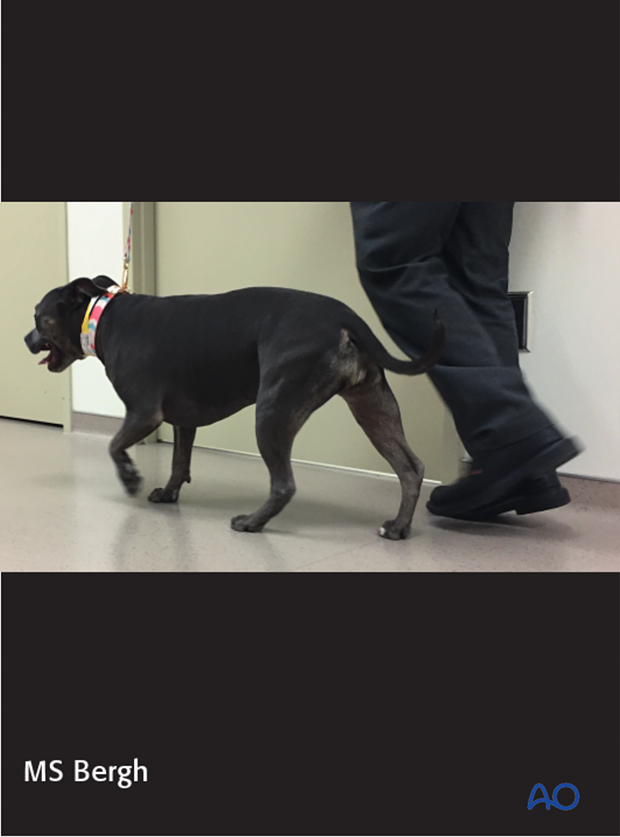
4-week postoperative radiographs demonstrate stable implants and progressive healing. The patient was clinically doing very well. The implants were not removed.
5. Aftercare
Activity restriction and controlled walking is indicated until evidence of bone healing is detected by radiographic examinations.
Phase 1: 1-3 day after surgery
The aim is to reduce the edema, inflammation and pain using anti-inflammatory and analgesic medications.
Passive range of motion of the hip and stifle joint can be initiated to promote mobility and joint health.

Phase 2: 4-10 days after surgery
The aim is to resolve the hematoma, edema and control pain, and prevent muscle contracture.
Anti-inflammatory and analgesic medications are still needed. Rehabilitation and integrative medical therapies can be used.
Special attention should be given to patients less than 1 year of age with a femoral fracture, as they are at risk for developing quadriceps contracture. Early controlled activity and passive range of motion is strongly recommended to help prevent this complication.
If the patient is not starting to use the limb within few days after surgery, a careful evaluation is recommended.
Phase 3: 10 days-8 weeks after surgery
Rehabilitation therapy is continued.
10-14 days after surgery the sutures are removed.
Radiographic assessment is performed every 4-8 weeks until bone healing is confirmed.

Implant removal
Implants may be removed if there is irritation or infection present, however if they are not causing problems for the patient, there is no need for implant removal.













