Posterior MIS
1. Introduction
Preliminary remarks
Minimally invasive surgery reduces the surgical time, blood loss, and trauma for the patient, potentially resulting in a quicker recovery while providing similar clinical mid to long term results. It is therefore the preferred procedure whenever possible.
Preoperative planning
Based on CT and MRI imaging, a plan should be prepared to determine:
- The size and optimal location of implants used
- Whether spinal cord decompression is necessary and if so, the amount of tissue to remove in order to achieve sufficient spinal cord decompression
Every case will be unique, and we will here illustrate just one example.
Length of construct and cement augmentation
In patients requiring posterior lateral decompression, not requiring anterior column reconstruction, bilateral posterior pedicle screw fixation with minimum fixation of at least one level above and below the involved segment should be used.
Short segment constructs lead to increased stress on the posterior implants increasing the risk of implant failure (screw pullout). The risk of implant failure may be decreased by cement augmentation of fenestrated screws and through reconstitution of the anterior column using cement augmentation of the pathological fracture, and/or use of vertebral body fillers/implants.
Fixation of multiple spinal segments does not affect functionality in the thoracic spine due to the presence of rigid rib cage. Adequate screw purchase should be aimed for during initial surgery as revision surgeries are too demanding for these patients.
Embolization
Embolization procedures are recommended to reduce operative blood loss in hyper vascular tumors especially for larger resections. For percutaneous procedures embolization is often not necessary due to limited or no resection of the tumor.
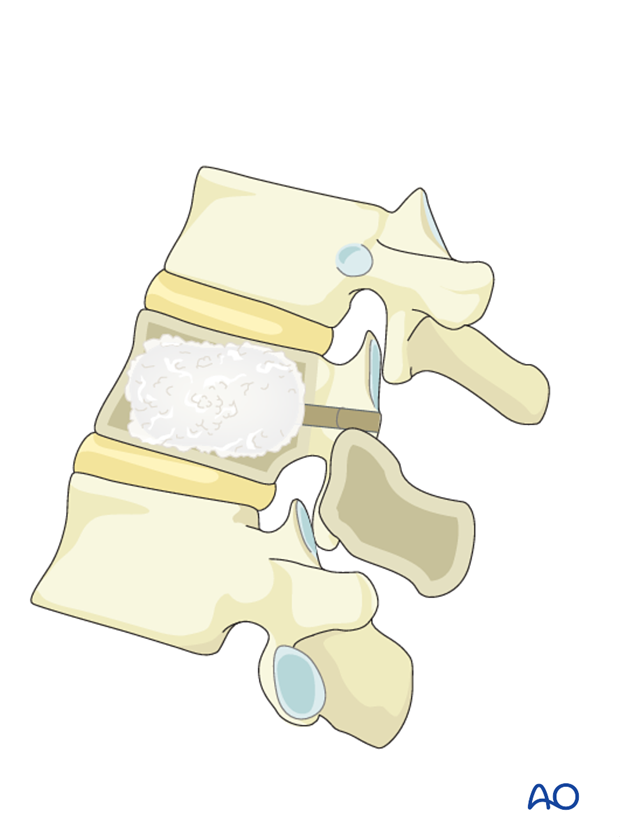
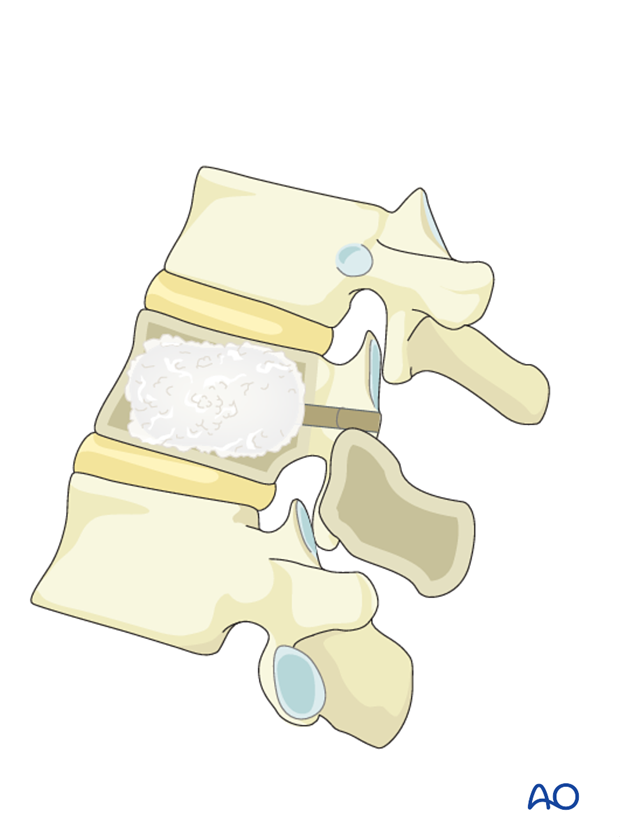
Anterior column support
In cases where the surgeon wishes to provide anterior column support, cement reconstruction using either vertebroplasty, kyphoplasty, or a vertebral body stent can be performed.
2. Patient positioning and surgical approach
For this procedure the patient is placed in the prone position and the minimally invasive approach for pedicle screw insertion is used.

Preoperative planning
Based on CT and MRI imaging, a plan should be prepared to determine:
- The size and optimal location of implants used
- Whether spinal cord decompression is necessary and if so, the amount of tissue to remove in order to achieve sufficient spinal cord decompression
Every case will be unique, and we will here illustrate just one example.
Length of construct and cement augmentation
In patients requiring posterior lateral decompression, not requiring anterior column reconstruction, bilateral posterior pedicle screw fixation with minimum fixation of two levels above and below the involved segment should be used.
Short segment constructs lead to increased stress on the posterior implants increasing the risk of implant failure (screw pullout). The risk of implant failure may be decreased by cement augmentation of fenestrated screws and through reconstitution of the anterior column using cement augmentation of the pathological fracture, and/or use of vertebral body fillers/implants.
Fixation of multiple spinal segments does not affect functionality in the thoracic spine due to the presence of rigid rib cage. Adequate screw purchase should be aimed for during initial surgery as revision surgeries are too demanding for these patients.
Embolization
Embolization procedures are recommended to reduce operative blood loss in hyper vascular tumors especially for larger resections.
Anterior column support
In cases where the surgeon wishes to provide anterior column support, cement reconstruction using either vertebroplasty, kyphoplasty, or a vertebral body stent can be performed.
3. Pedicle screw insertion (MIS)
Pedicle screw insertion
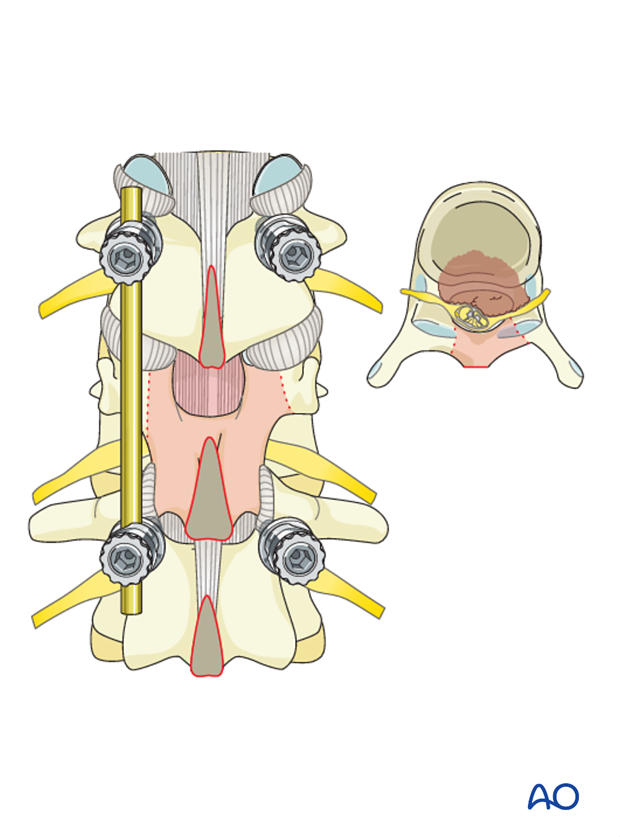
Pedicle screws are inserted one or two levels above and below the tumor on both sides. Mono- or polyaxial top or side loading screws can be used in any combination.
In tumor patients achieving optimal screw purchase is even more important than in trauma patients to minimize risk of pullouts and reduce the number of levels involved.
Optimal pedicle screw purchase will, in order of importance, be achieved by:
- Selecting the largest possible screw diameter
- Selecting the longest possible screw
- Positioning of the screw under the cranial endplate
- Cement augmentation of the screw.
Rod contouring
Rod contouring should mainly follow the curvature of the spine. Reducing preexisting deformities is typically not necessary and may lead to screw pull-out.
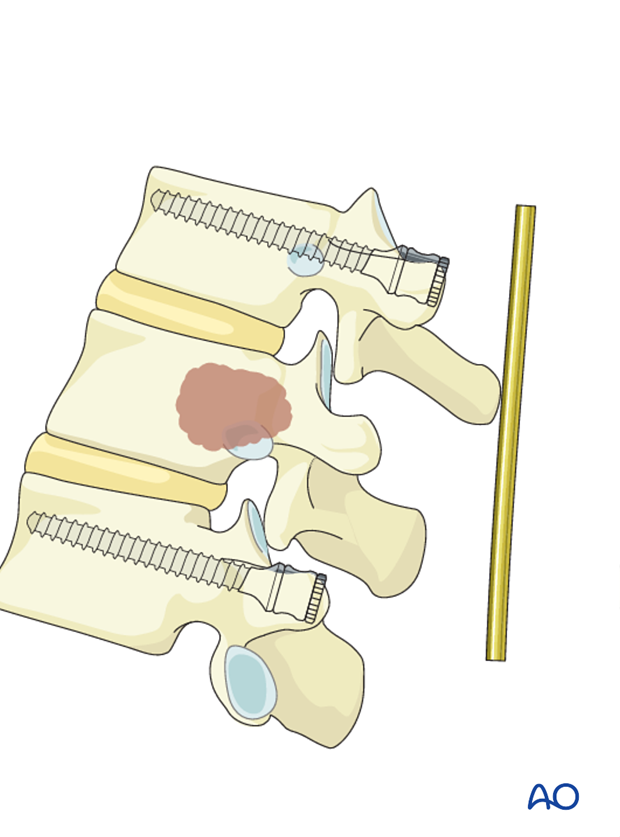
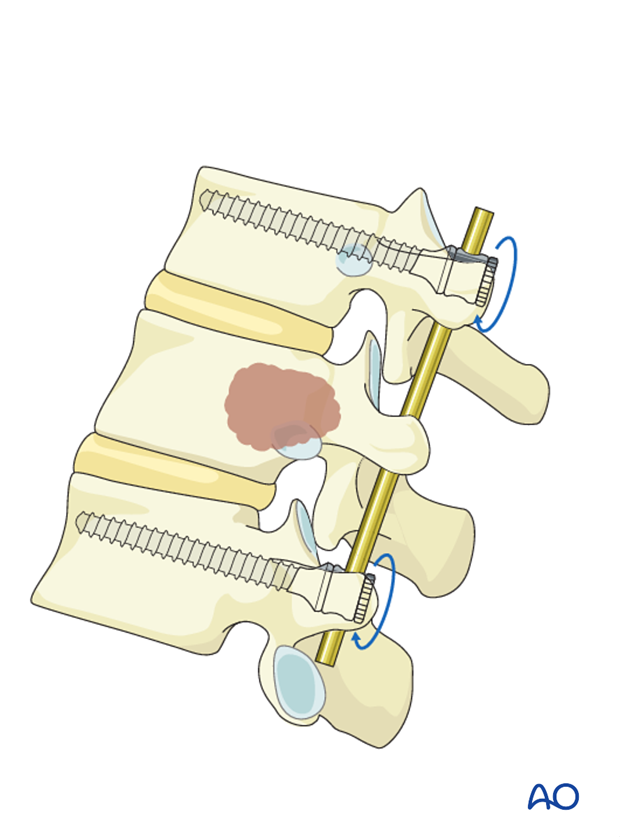
Rod insertion
The rods are inserted into the screw heads and the screw heads are tightened with the inner nuts.
If decompression is performed, one rod is inserted before and one after the compression.
4. Decompression
Timing of decompression
A patient who is experiencing neurologic deficit from solid tumor ESCC resulting in loss in ability to ambulate, in the absence of medical and oncological contraindications, requires urgent surgical decompression.
Expeditious diagnosis and prompt surgery are recommended to improve the probability of neurological recovery.
Technique
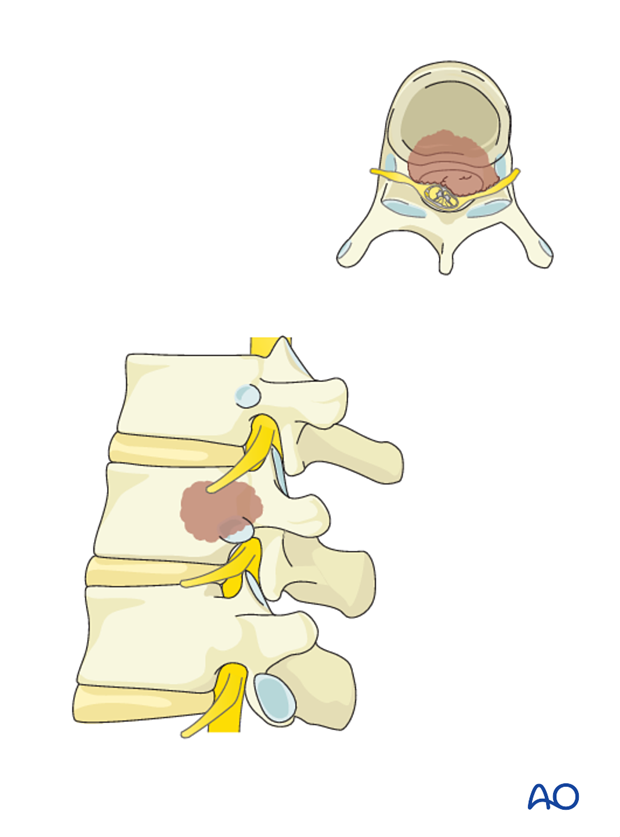
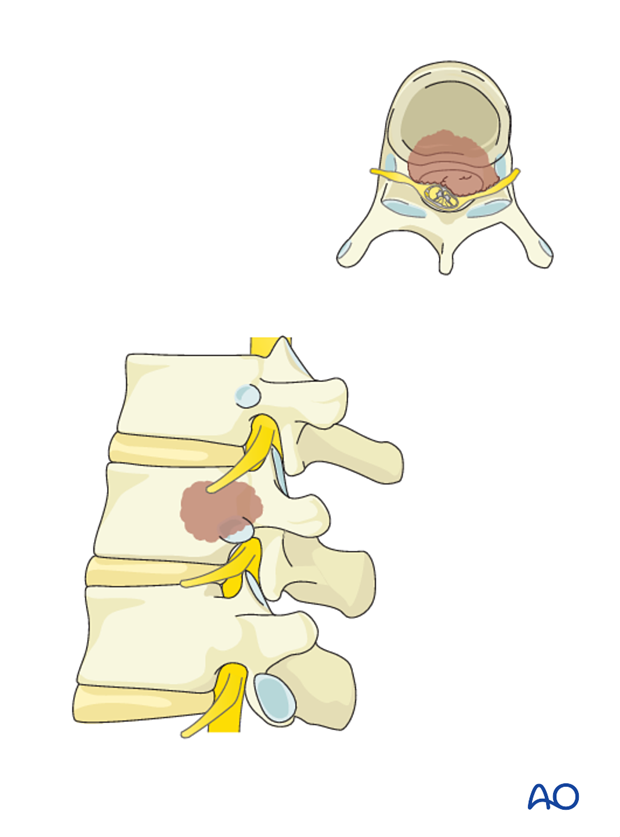
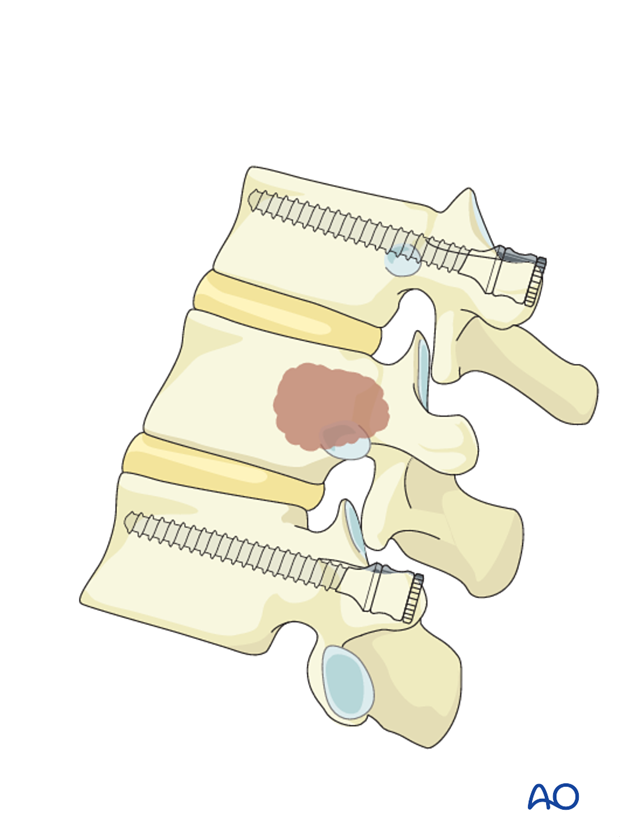
Since most tumors originate in the vertebral body, transpedicular decompression is required in order to provide access to the ventral epidural space in order to achieve full spinal cord decompression, if this is the goal. In this technique commonly known as separation surgery, decompression is performed through the pedicle.
This technique can be performed from T1 to L5 levels, without the risk of retracting the thecal sac.
A laminectomy is performed at the area between the pedicles of the affected vertebra. The laminectomy is performed through a small midline incision centered over the affected level. Alternatively, it can be performed using tubular or expendable retractors. To illustrate the procedure we will here use a small midline incision.
Based on preoperative planning, the amount of lamina to be removed to achieve enough decompression can be determined beforehand.
The adjacent spinous processes and the intervening ligamentum flavum are excised.
Half of the superior and inferior lamina and the medial portion of the facet joint are removed.
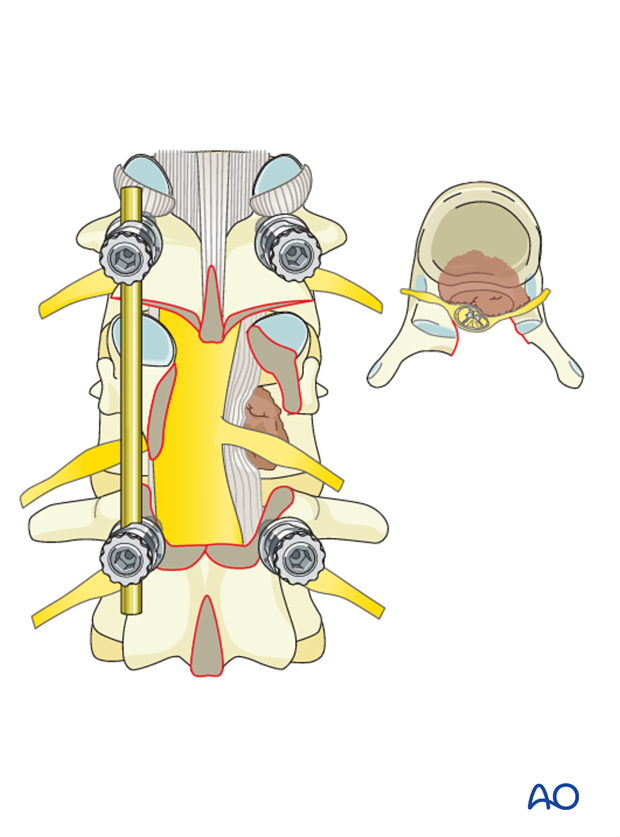
For T2-T12 tumors, the nerve roots may be ligated in order to facilitate exposure of the ventral epidural space and the vertebral body.
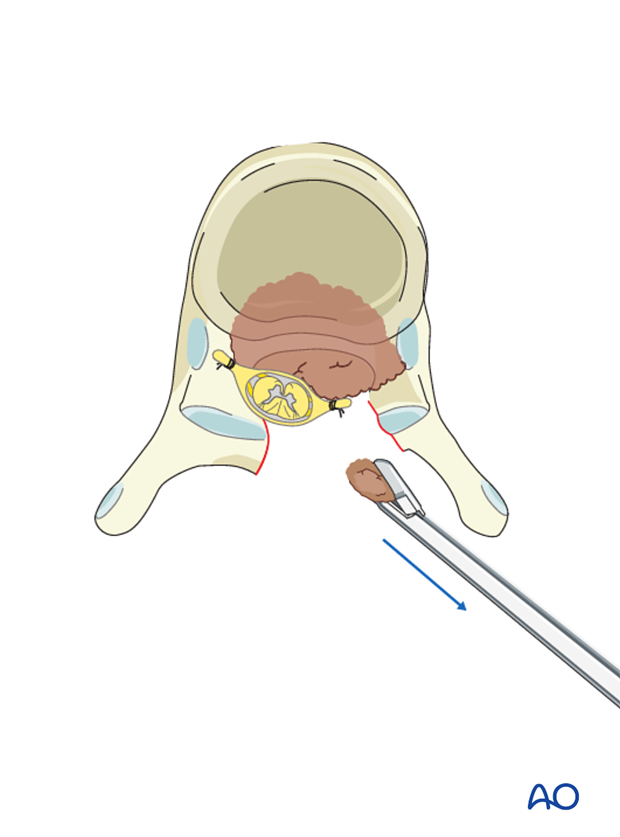
The posterior longitudinal ligament (PLL) should be identified and separated from the dura with a dura dissector. The PLL should be cut in order to expose the vertebral body and the epidural tumor.
The spinal cord, dura, and tumor should be manipulated as little as possible.
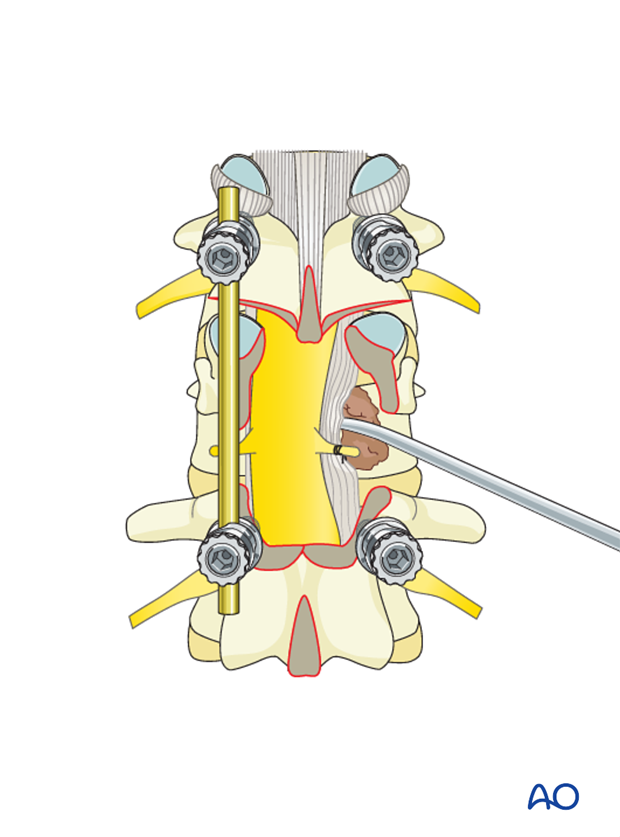
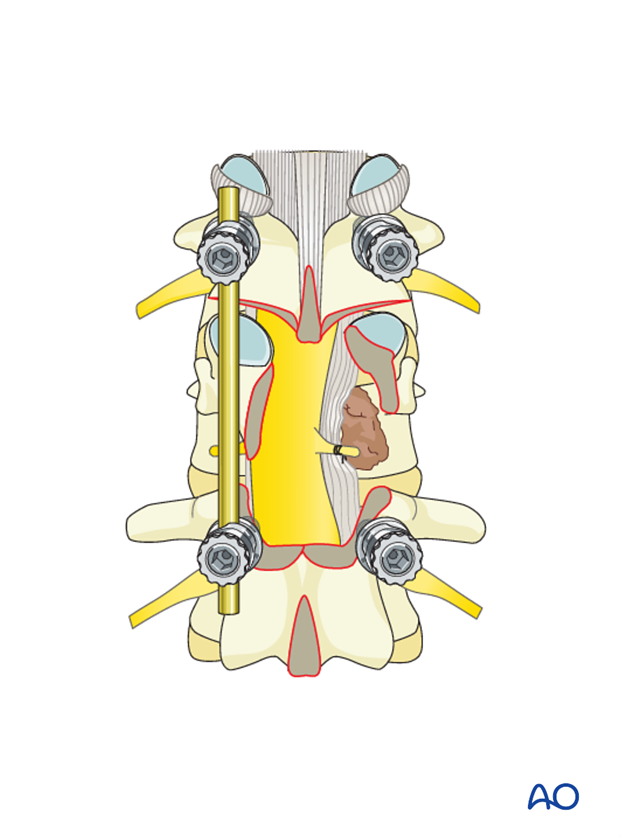
Reverse-angle curettes and pituitary rongeurs can be inserted through this opening, and any tumor and bone fragments compressing the anterior neural elements can be removed or impacted into the vertebral body.
If further decompression is needed, the same technique may be applied on the other side.
If the decompression is adequate on both sides of the canal, with no further decompression, the second rod may be fixed and tightened.

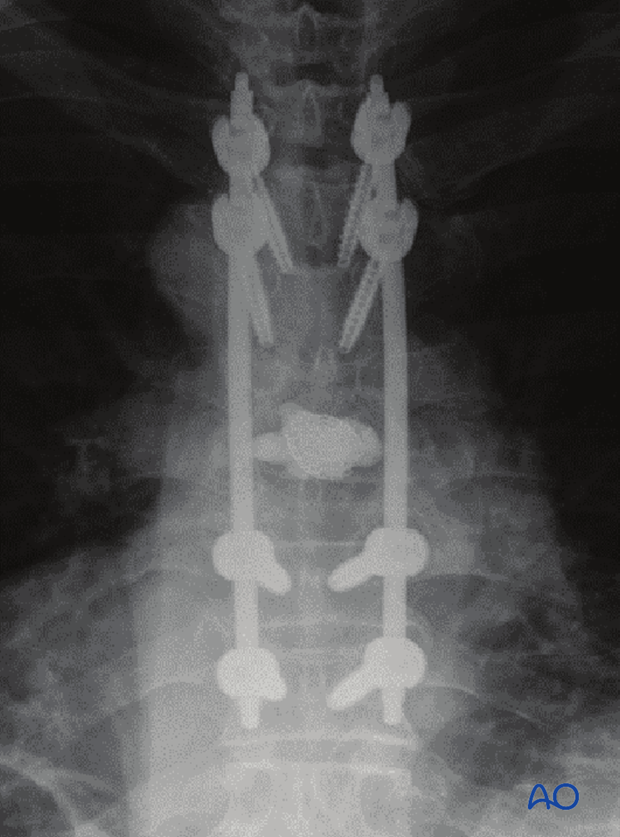
The final construct is shown from a lateral view.

5. Intraoperative imaging
Prior to wound closure, intra-operative imaging is performed to check the adequacy of reduction, position and length of screws and the overall coronal and sagittal spinal alignment.
6. Aftercare
Patients are made to sit up in the bed on the first day after surgery. Bracing is optional but preferably omitted for patient comfort. Patients with intact neurological status are made to stand and walk on the first day after surgery.
Patients can be discharged when medically stable or sent to a rehabilitation center if further care is necessary.
During admission adequate caloric intake of a high-quality diet should be monitored.
Patients are generally followed with periodical x-rays and (optionally) MR imaging at 6 weeks, 3 months, 6 months, and 1 year to monitor for tumor recurrence and hardware failure.
Postoperative radiation is required to avoid tumor recurrence. SBRT is usually initiated within two weeks following surgery. Conventional radiotherapy is usually initiated 2-4 weeks after surgery to reduce the risk of wound healing disturbances.
The radiation modality is selected based on tumor histology and history of prior radiation.













