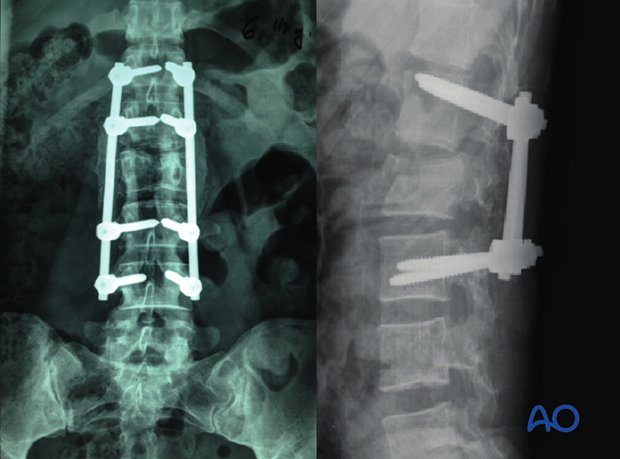
Posterior long segment fixation (C)
1. Introduction
Preliminary remarks
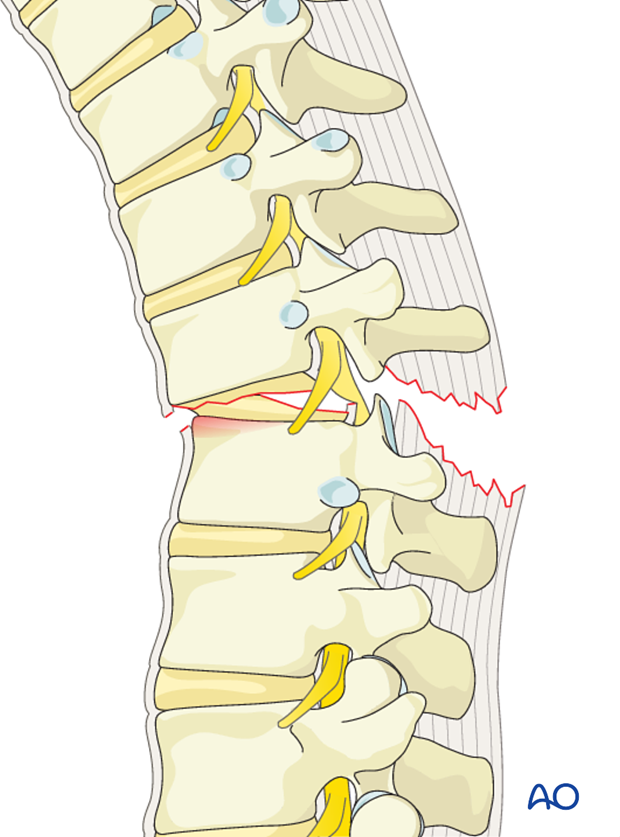
C type injuries are high impact injuries that result in translational and rotational instability of the vertebral column. Most fractures are associated with severe cord injury and complete neurologic deficit. More than 50% of the fractures are associated with dural injuries and cerebrospinal fluid leak. Associated injuries of the intrathoracic and intrabdominal organs are common. Management is aimed at resuscitation, control of life threatening organ injuries, spinal stabilization, and rehabilitation.
Repair of dural laceration
More details on repair of dural laceration can be found here.
2. Patient preparation and approach
The posterior open approach to the midline is used together with the appropriate patient preparation.
3. Reduction with pedicle screws
Preliminary remarks
Due to the fact that bilateral instrumentation is necessary in all cases, all steps described below are repeated on the opposite side unless otherwise described.
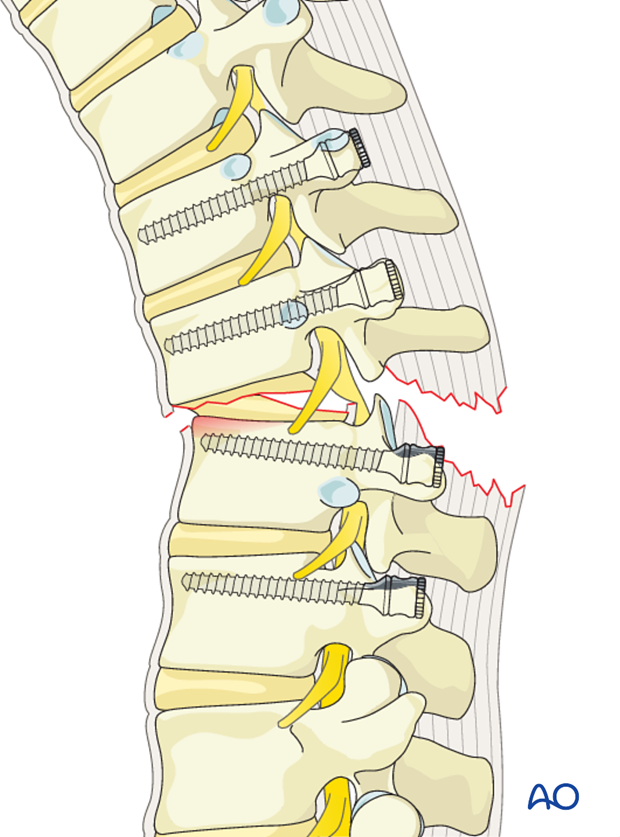
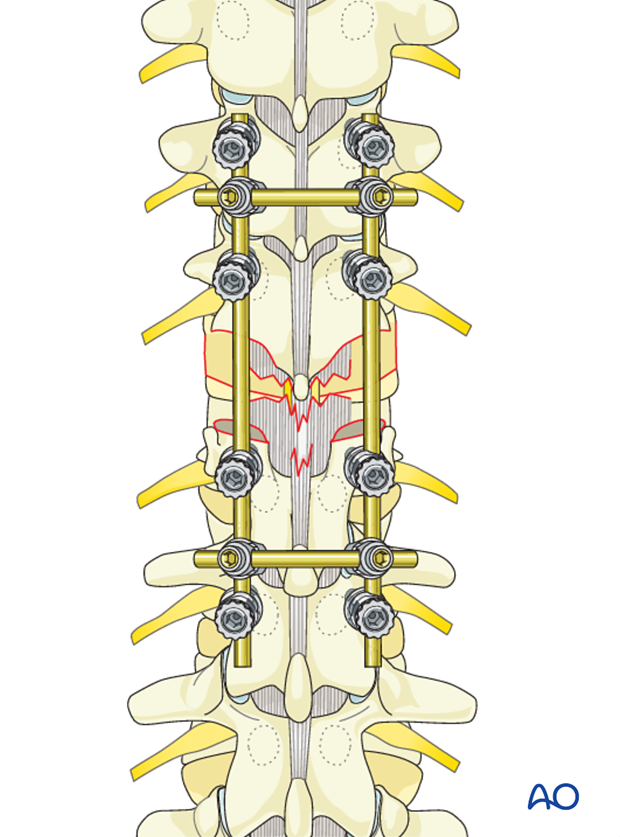
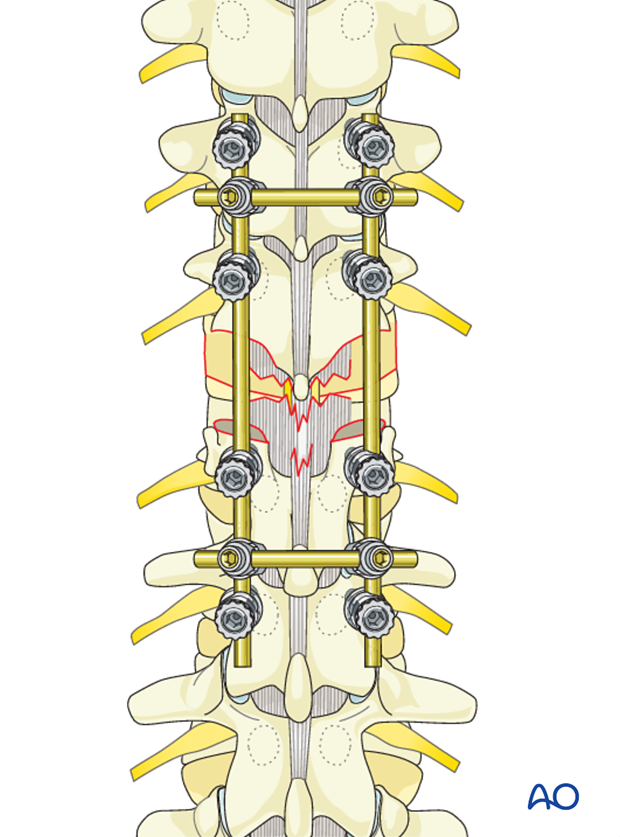
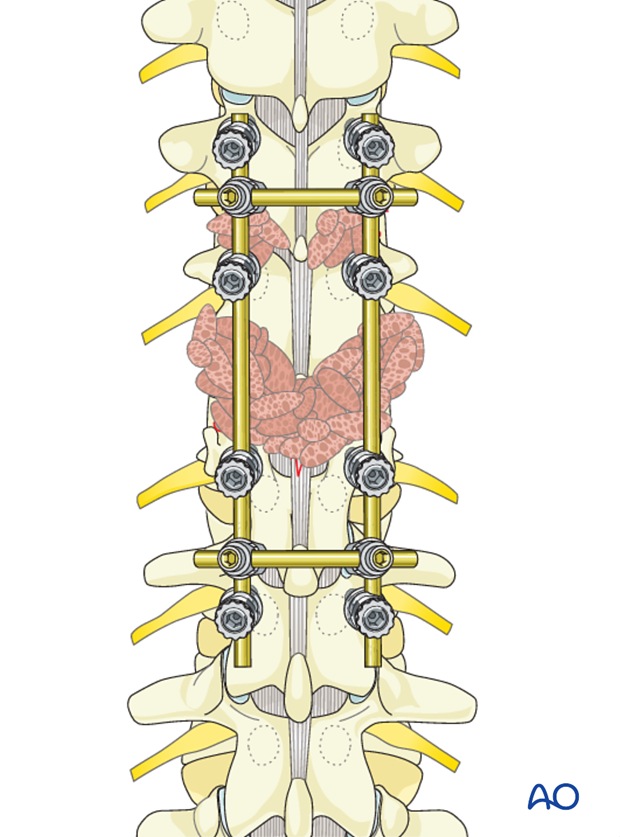
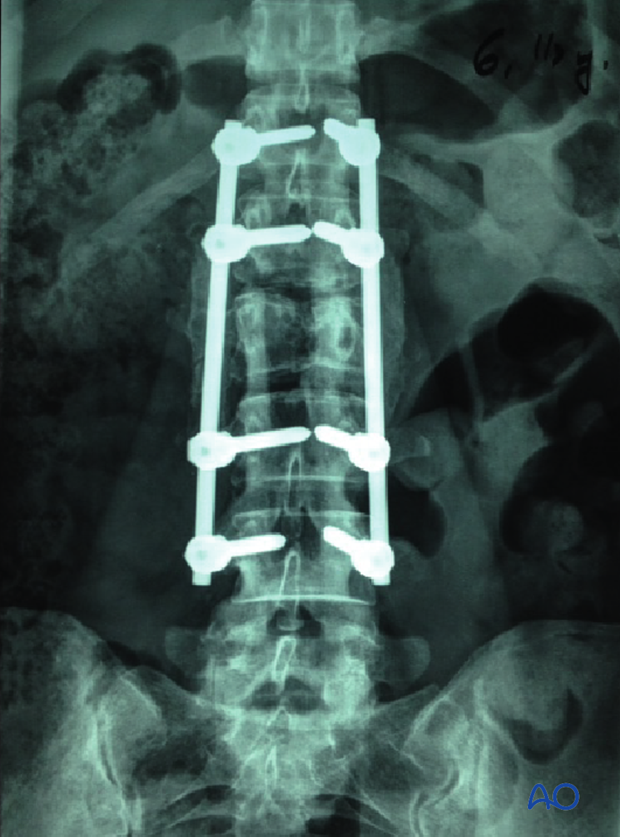
C type injuries are rotationally unstable injuries and hence posterior long segment fixation is performed to provide better reduction forces and biomechanical stability. Short segment constructs lead to increased stress on the posterior implants resulting in implant failure.
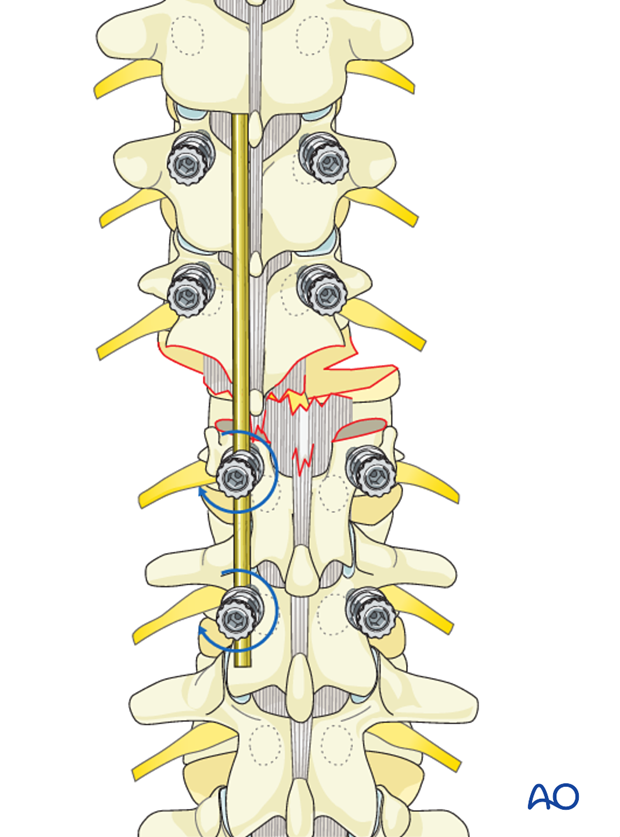
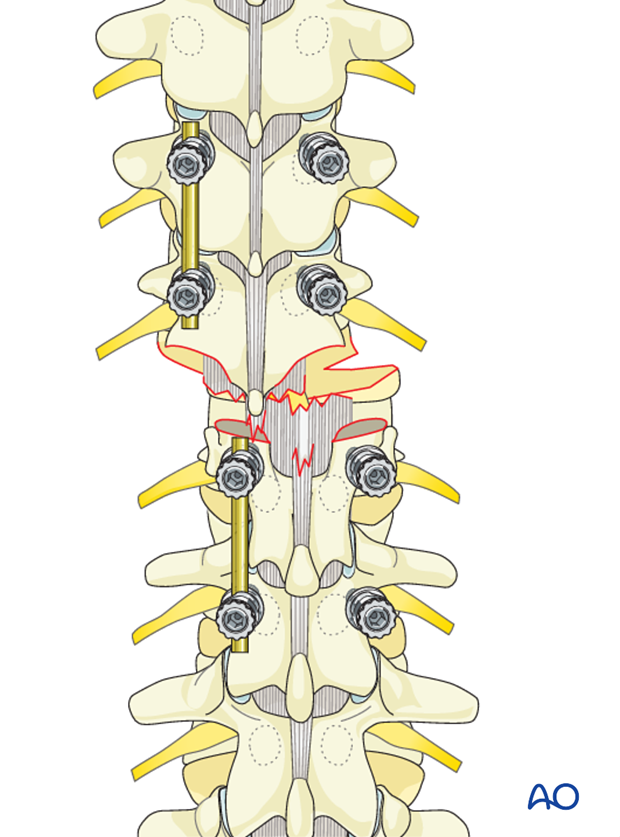
Pedicle screw insertion
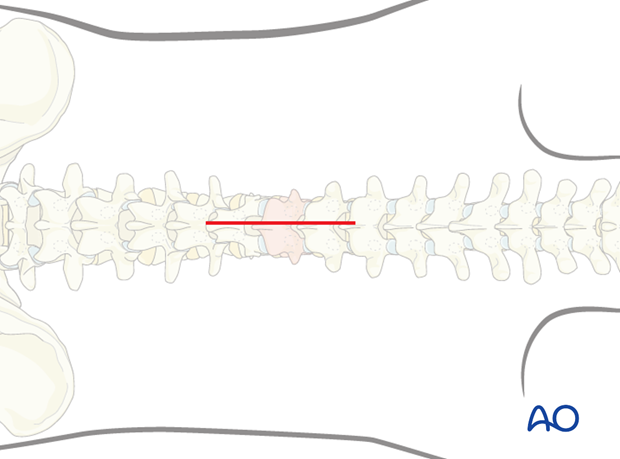
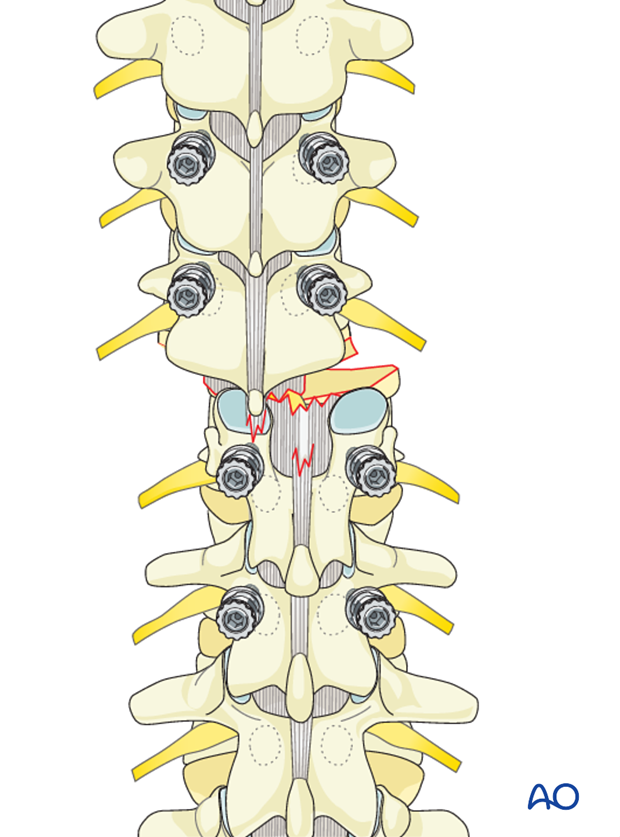
In this technique, pedicle screws are inserted at least two levels above and below the fractured level on both sides.
This is essential in unstable injuries where stress on the posterior implants is high.
Rod contouring
Once pedicle screws are inserted on both sides, long rods are used to connect them.
The contouring of the rod depends on the site of the fracture. A rod contoured in mild kyphosis is chosen for fractures from T1-T10. A straight or a slightly lordotic rod is chosen for fractures from T11-L1, and a rod contoured to lordosis is chosen for lumbar fractures.
4. Reduction techniques for type C fractures
Introduction
A variety of techniques are preferred by surgeons to reduce a dislocation of the thoracolumbar spine. The basic requirement in all these techniques is the use of long segment fixation with at least two screws above and below the injury.
The major impediment to reduction is the presence of dislocated facet joints.
The common first step in all techniques is the removal of the dislocated facets with a nibbler or Kerrison rongeur on both sides.
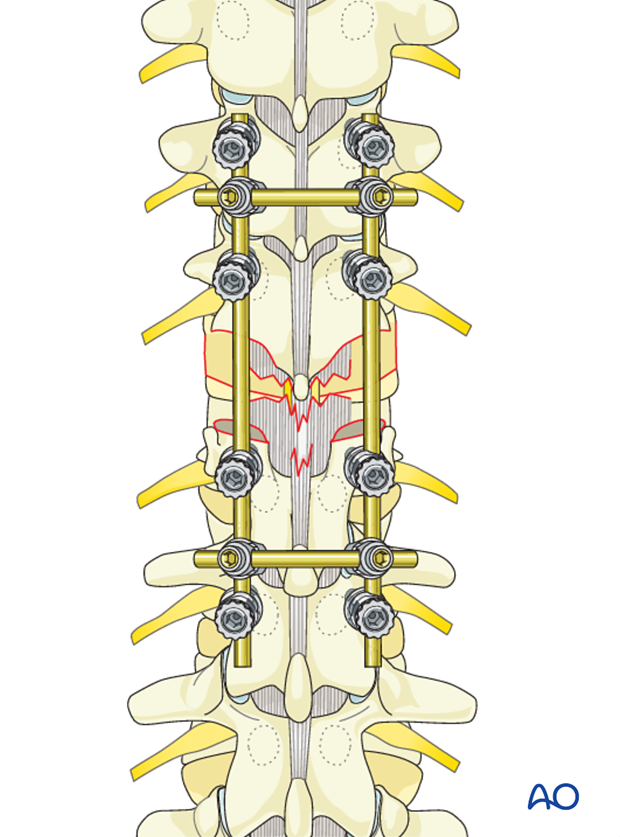
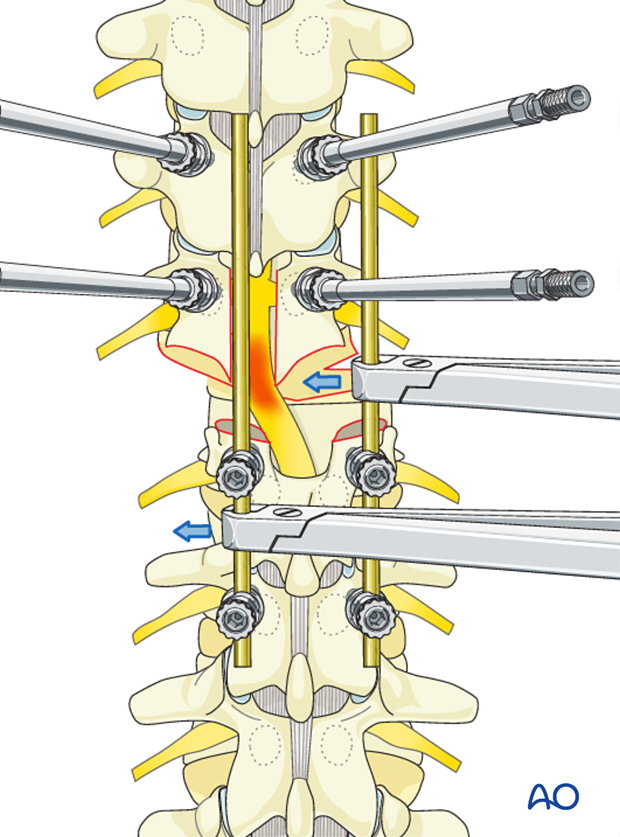
Technique 1
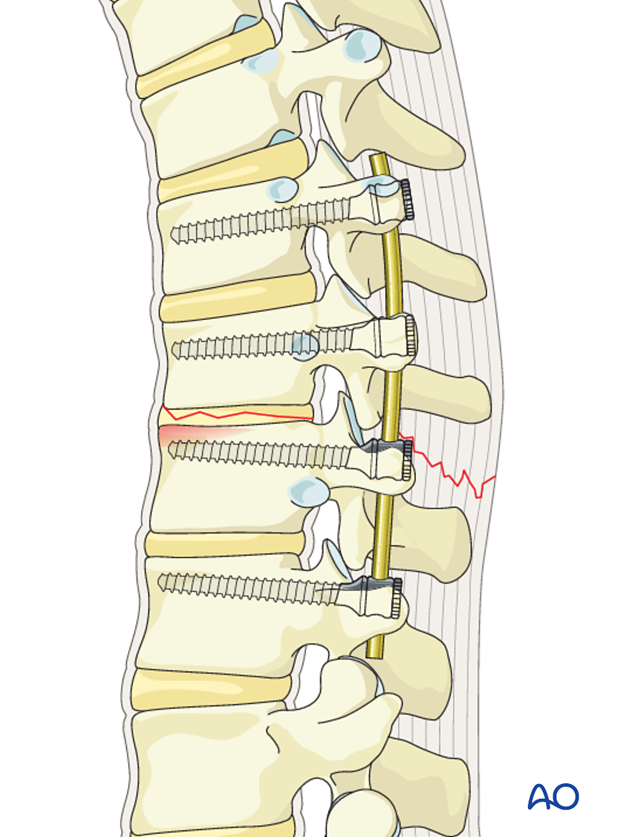
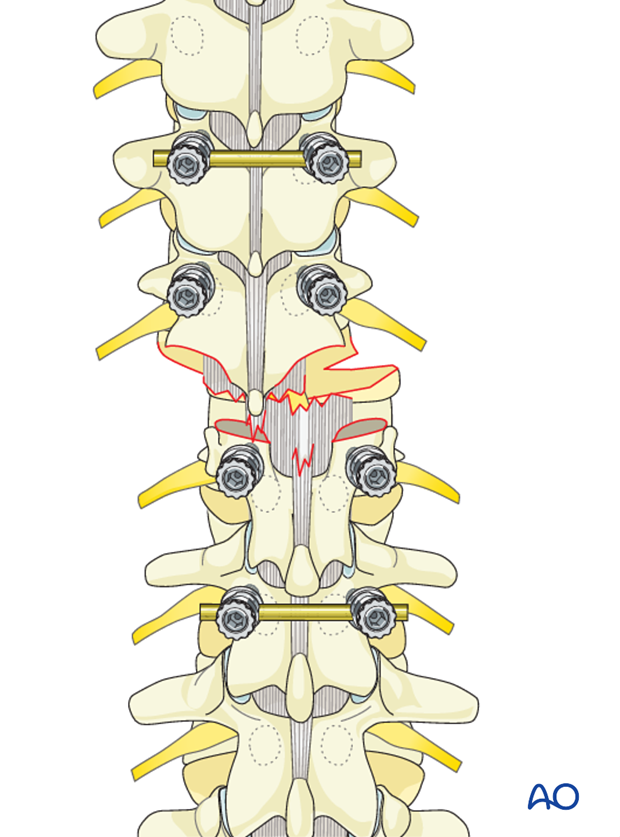
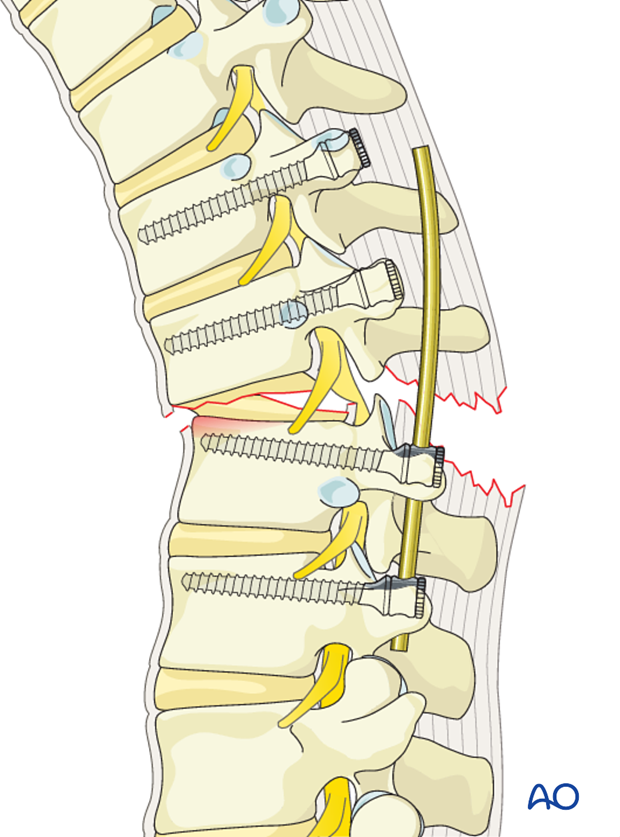
A long rod is placed on the distal two screws on one side. The distal screws are then tightened. Due to the presence of dislocation, the rod stands away from the proximal screw heads.
A lamina spreader is applied in between the spinous processes at the level of dislocation and gently distracted. With distraction, the dislocation gets reduced and the rod is gently guided into the proximal screw heads.
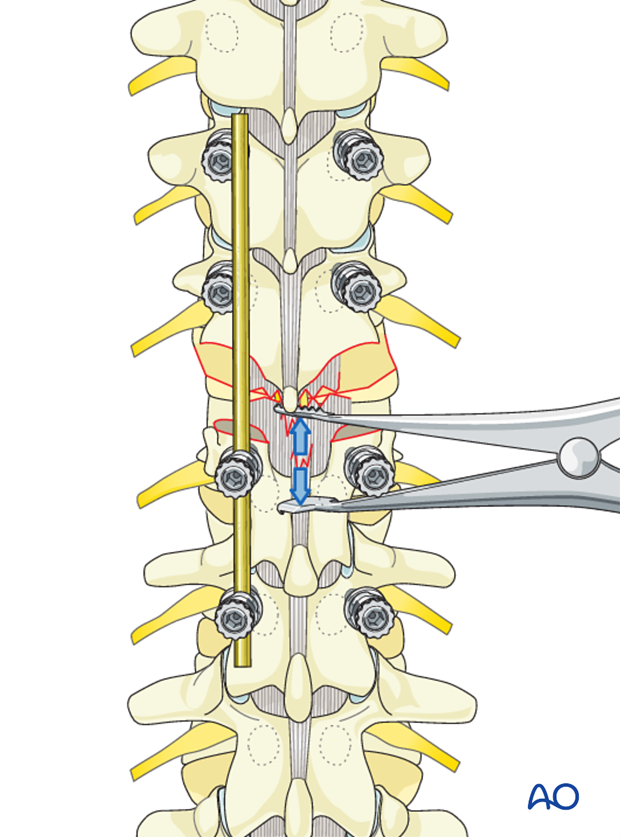
Inner nuts are placed into the proximal screw heads and tightened to secure the reduction achieved.
Another rod is placed on the opposite side and tightened into the screw heads.
Stability is secured, adding two cross links.
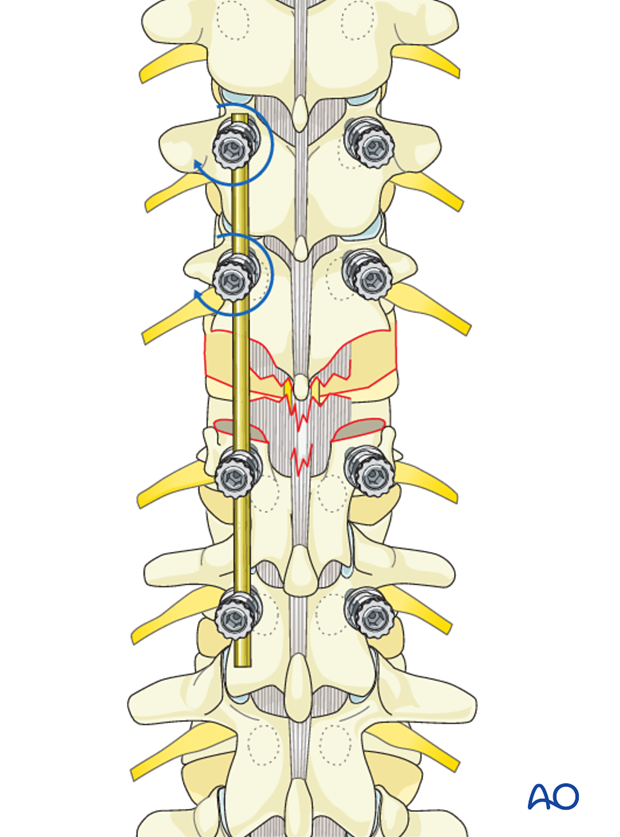
Technique 2
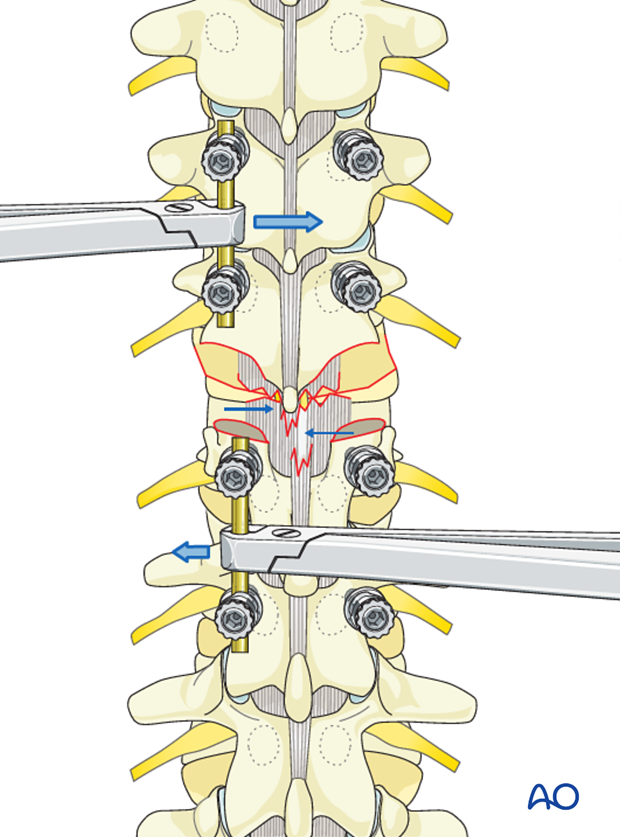
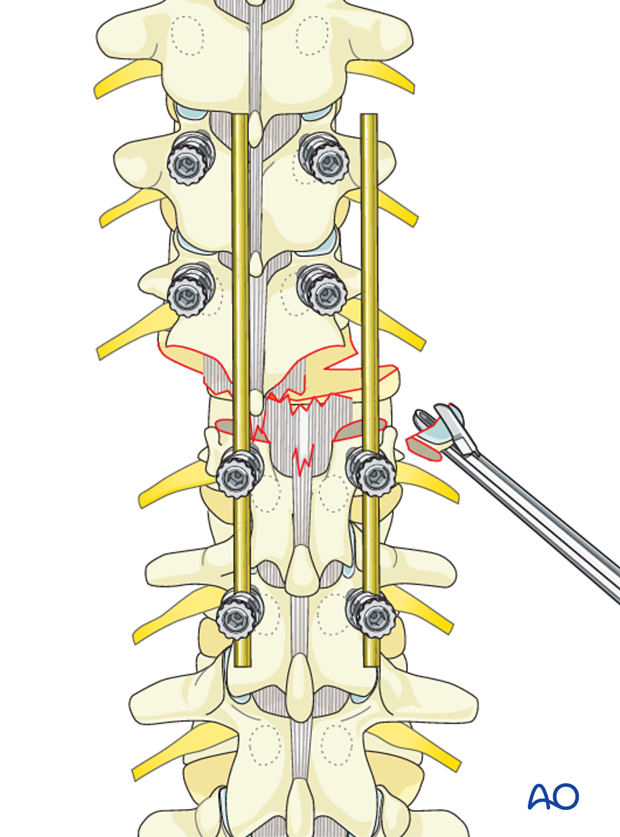
A long rod is placed on the distal two screws. The screw heads are tightened. Due to the presence of dislocation, the rod stands away from the proximal screw heads.
The spinous processes of the proximal and distal vertebra at the level of dislocation is held with a reduction forceps and manually distracted. By gently pulling and maneuvering the distal segments, the dislocation is reduced and the rod is guided into the proximal screw heads.
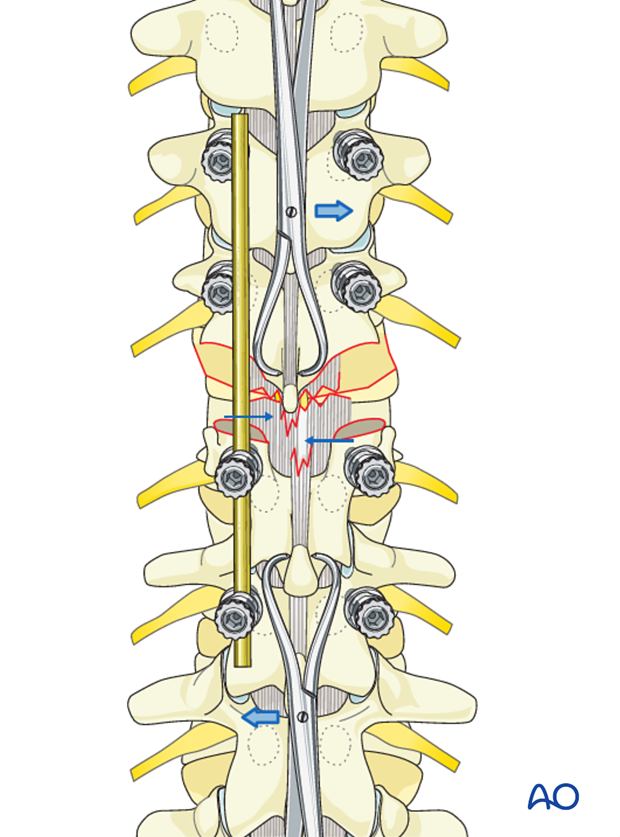
Inner nuts are placed into the proximal screw heads and tightened to secure the reduction achieved.
Another rod is placed on the opposite side and tightened into the screw heads.
Stability is secured, adding two cross links.
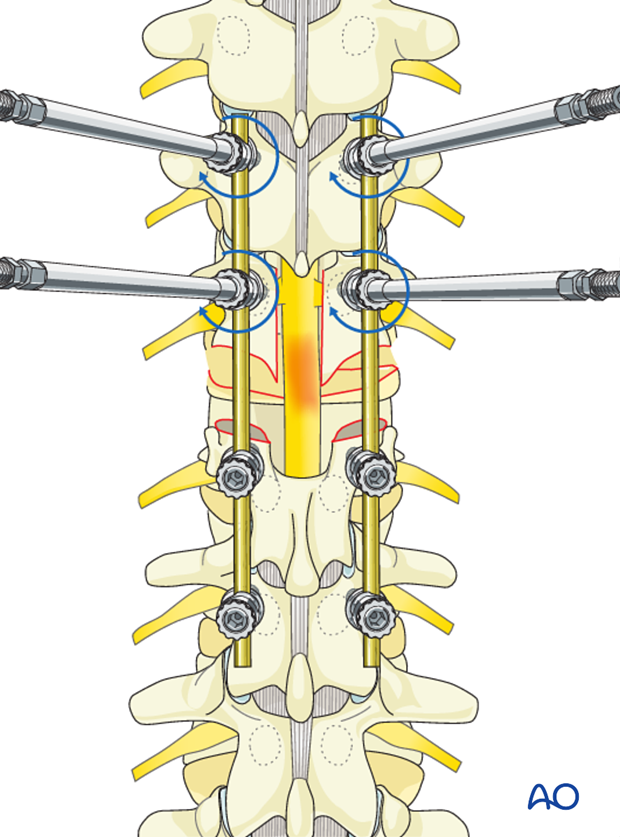
Technique 3
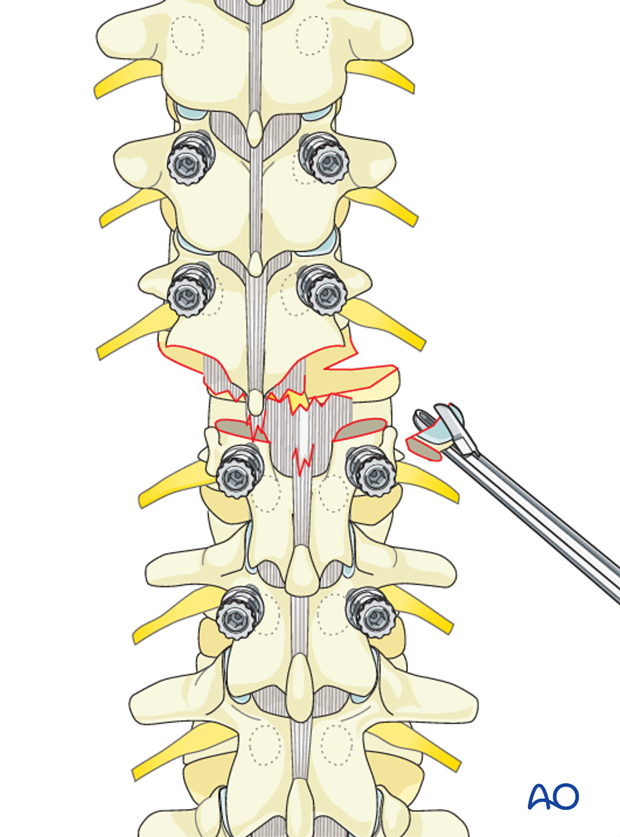
Two temporary rods are inserted horizontally into the two proximal and distal screws above and below the level of injury.
The screw heads are tightened provisionally.
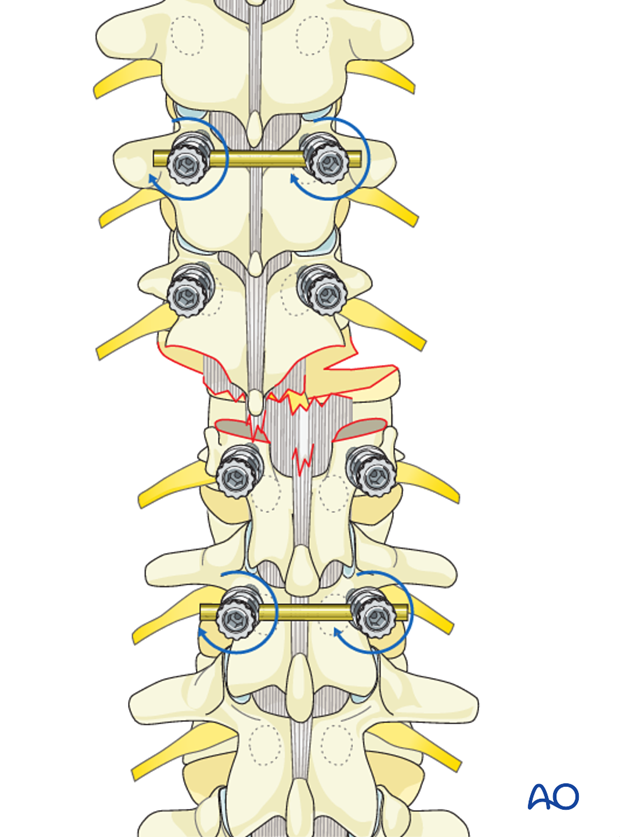
These horizontal rods are held with a rod holder and now used to maneuver reduction.
Instead of using the reduction forceps as in technique 2, this technique allows the surgeon to use stronger forces to manipulate the vertebral segments.
Once reduction is achieved, it can be stabilized by the use of a short rod on one side.
The two horizontal rods are now removed and a long rod is placed on the right side.
The short temporary rod is now removed and a definitive rod is placed and the screw heads tightened.
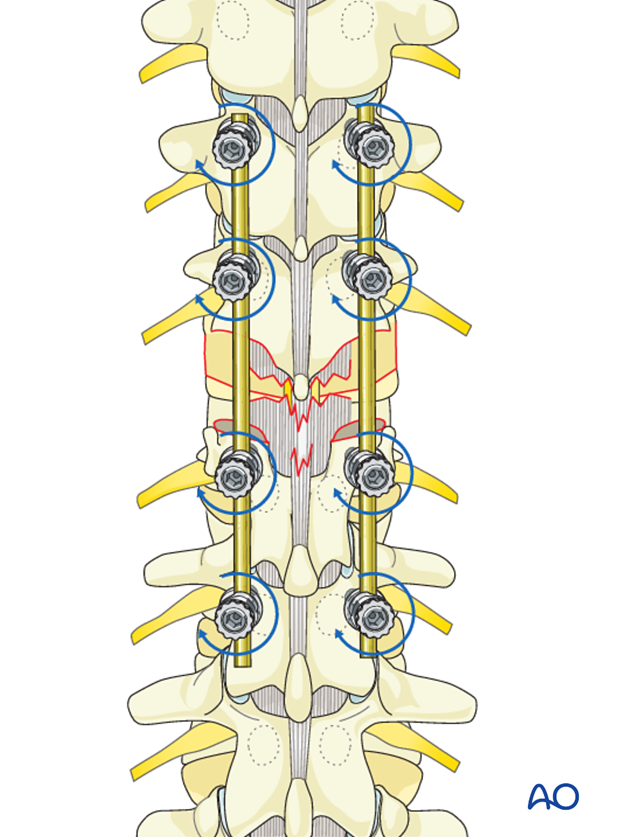
Stability is secured, adding two cross links.
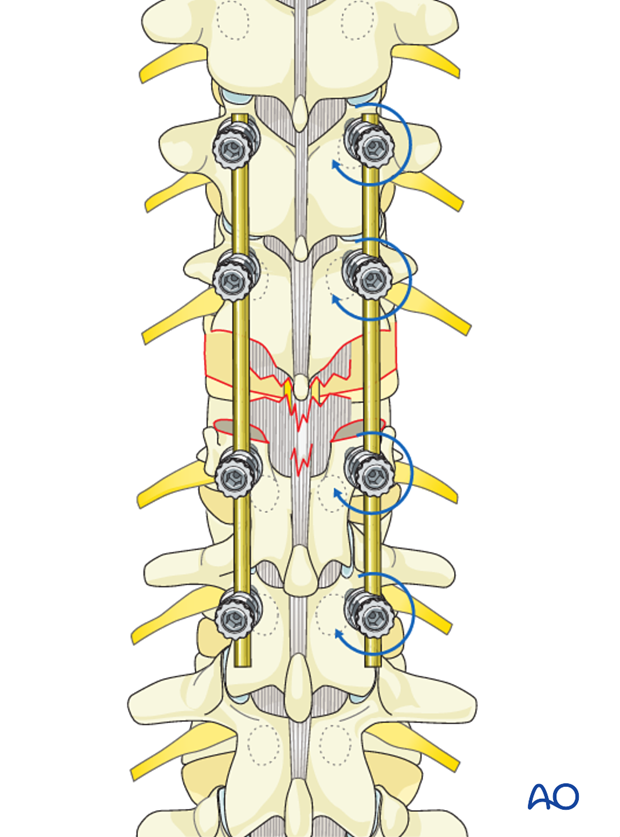
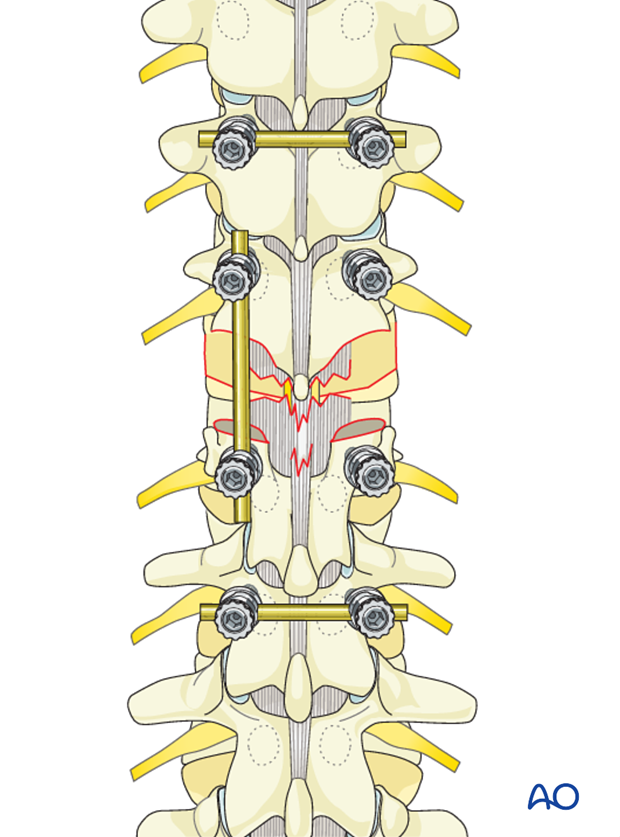
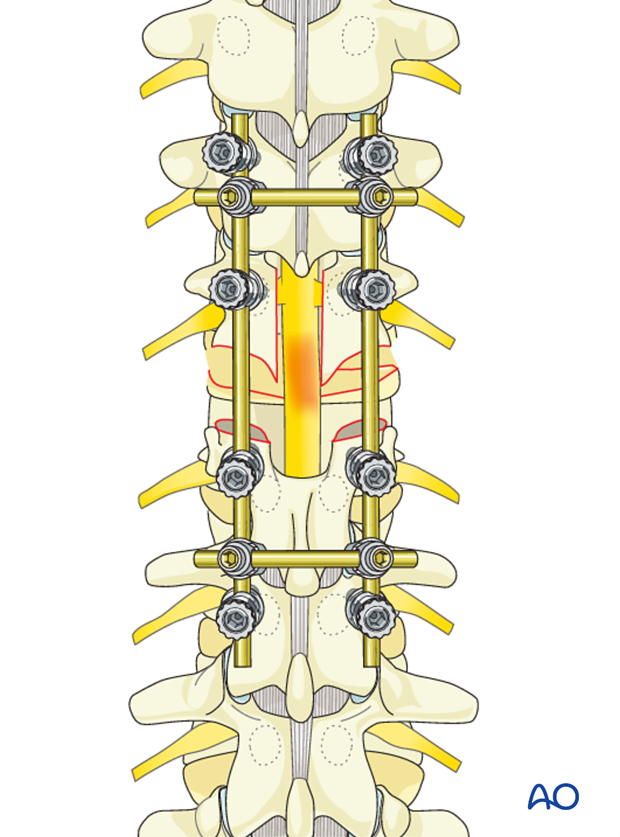
Technique 4
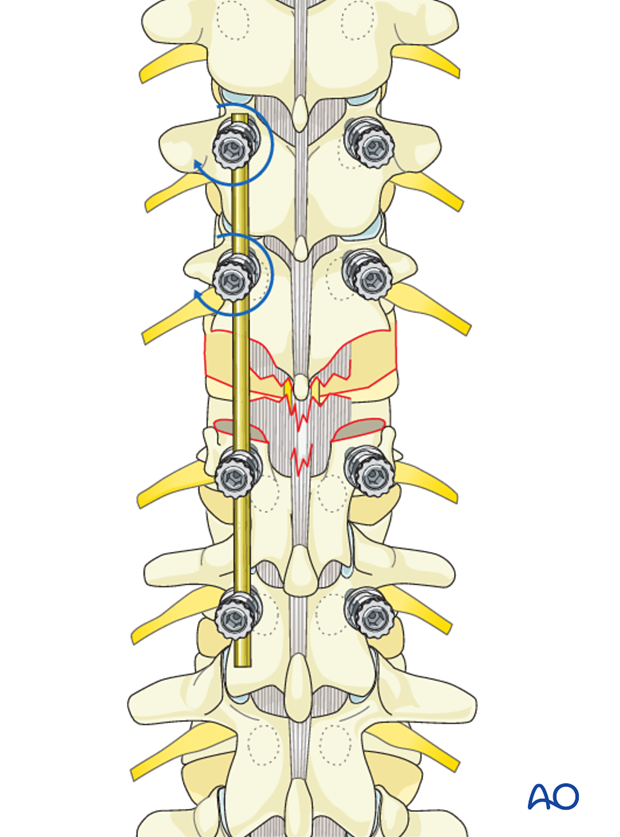
Instead of horizontal application of rods, small vertical rods are inserted above and below the injury level on one side only.
These temporary rods are held with rod holders and used to gently manipulate and reduce the dislocation. Instead of using the reduction forceps as in technique 2, this technique allows the surgeon to use stronger forces to manipulate the vertebral segments.
Once the reduction is achieved, a long rod is placed on the opposite side and tightened.
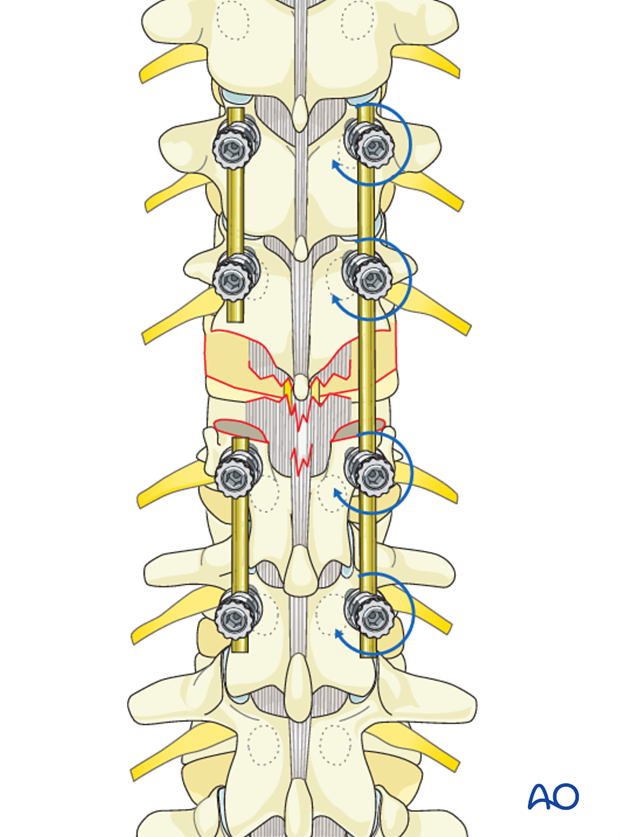
The short rods are removed and replaced by a definitive long rod. The screw heads are then tightened.
Stability is secured, adding two cross links.
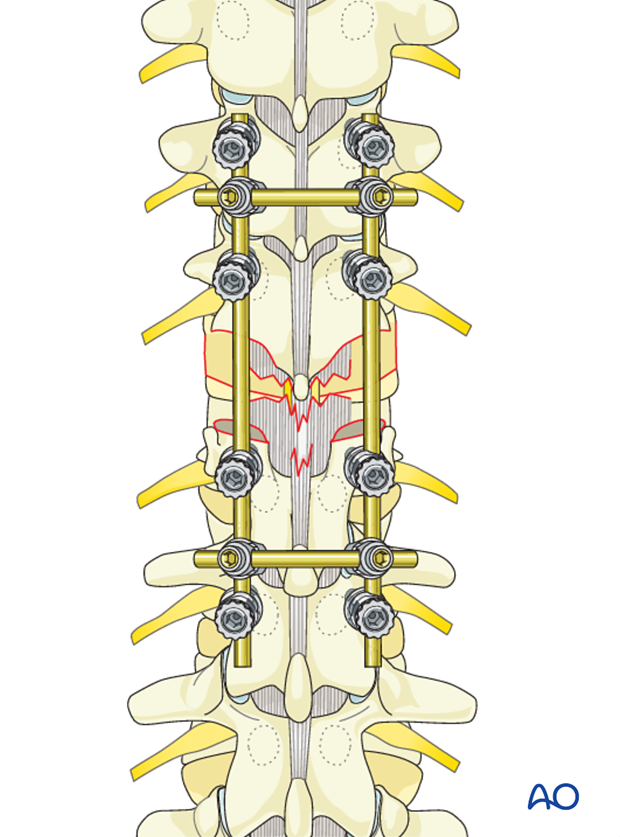
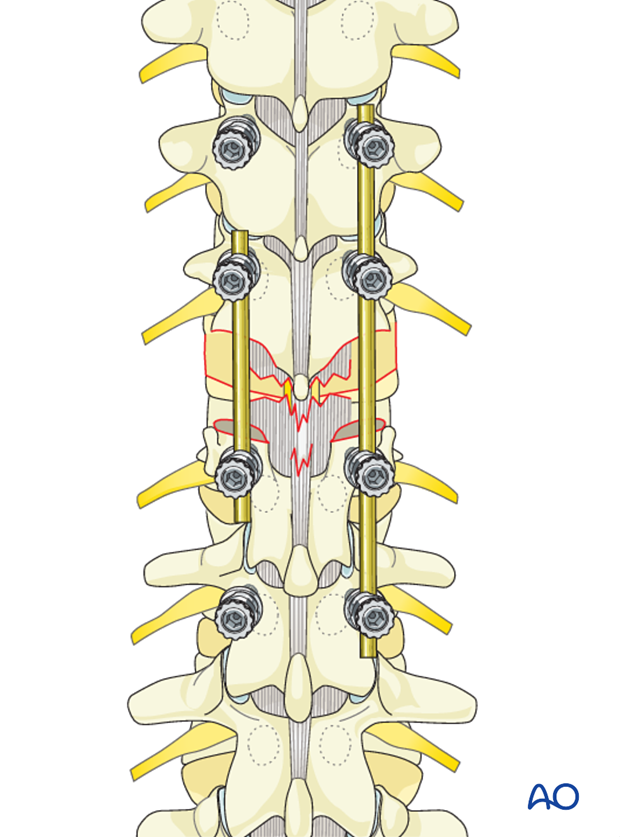
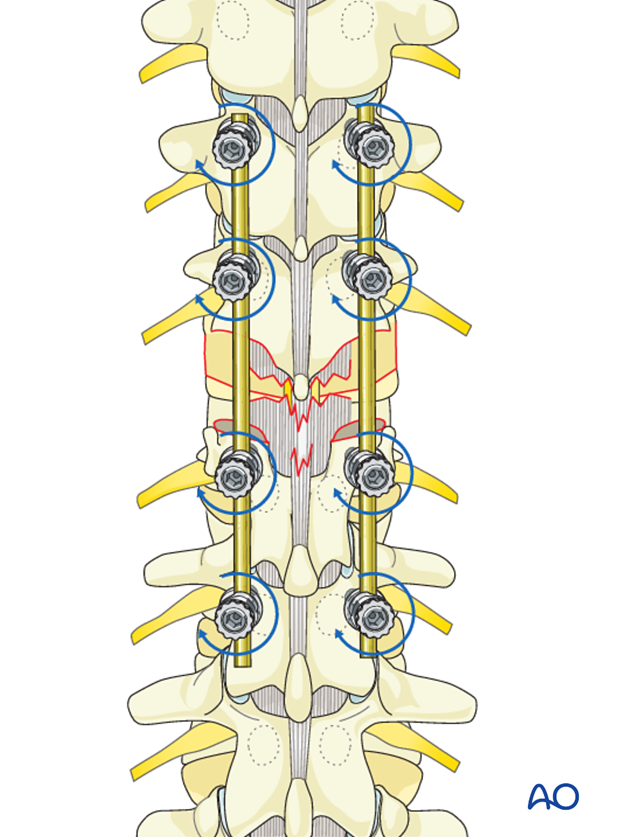
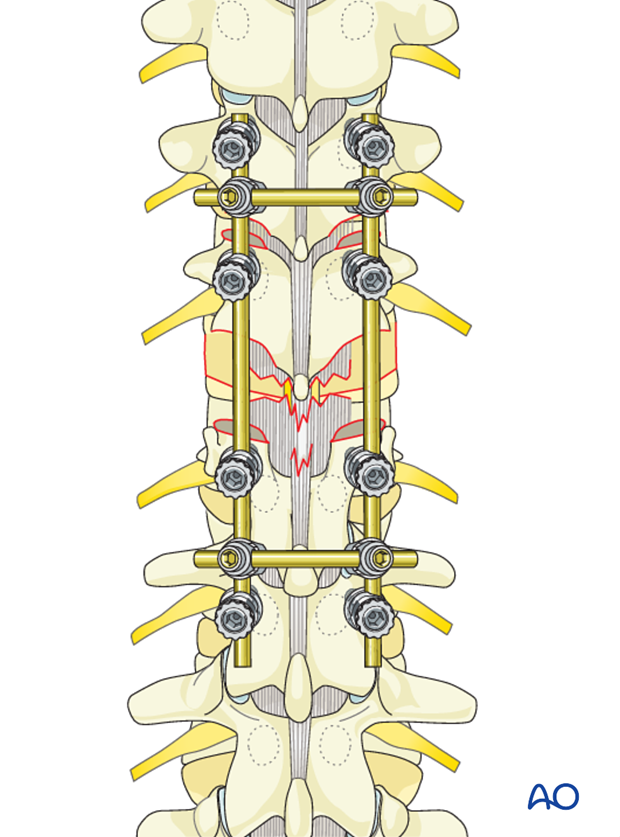
Technique 5
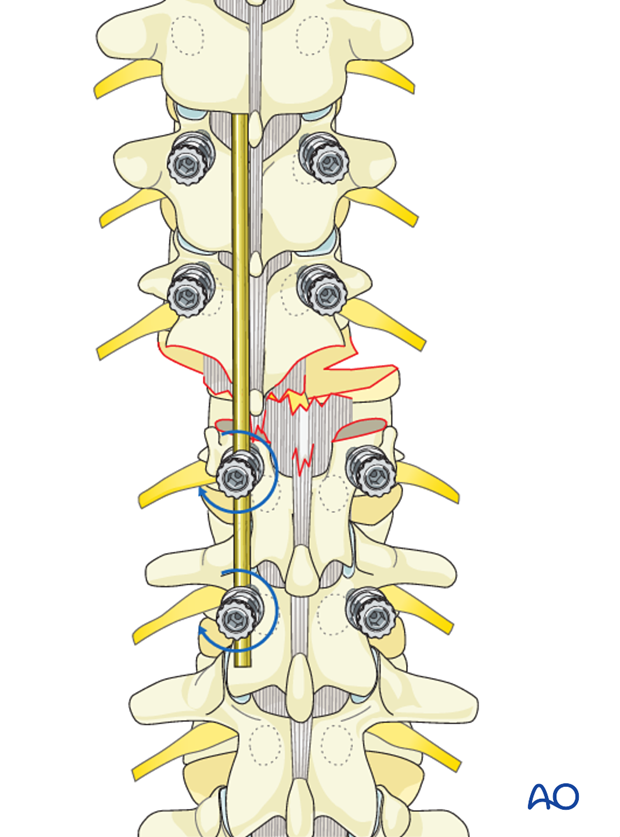
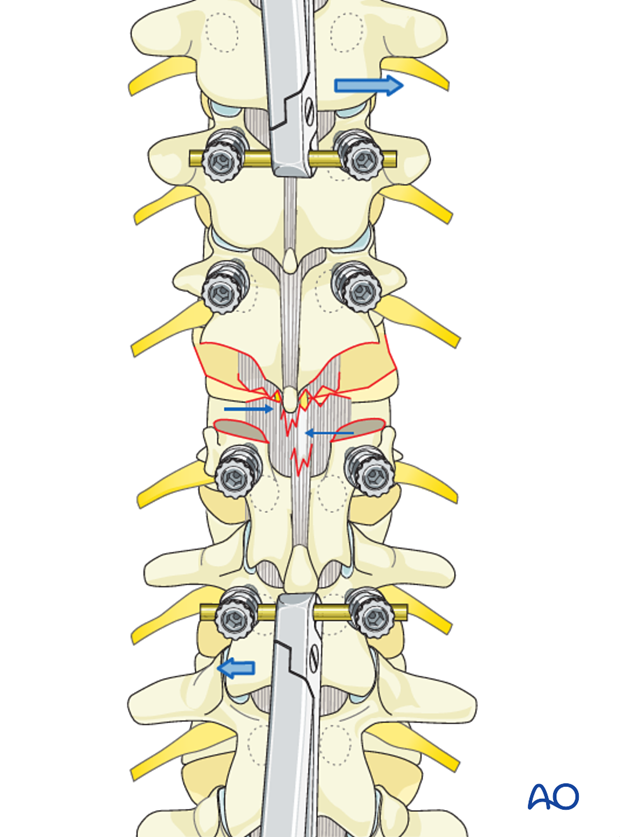
This technique is preferred in patients with incomplete neurology where major reduction forces cannot be applied.
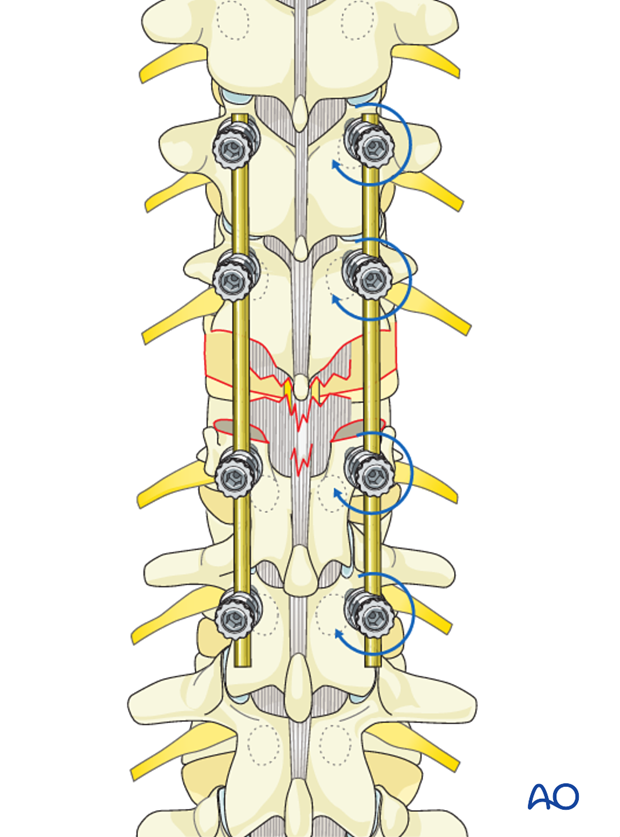
Two long rods, which have been contoured appropriately to the region of the fracture, are placed on the distal two screws on each side. Due to the presence of dislocation, the rods stand away from the proximal screw heads.
The facet joints at the level of dislocation are removed on both sides.
A wide laminectomy is performed to have a direct vision of the neural structures at the level of dislocation.
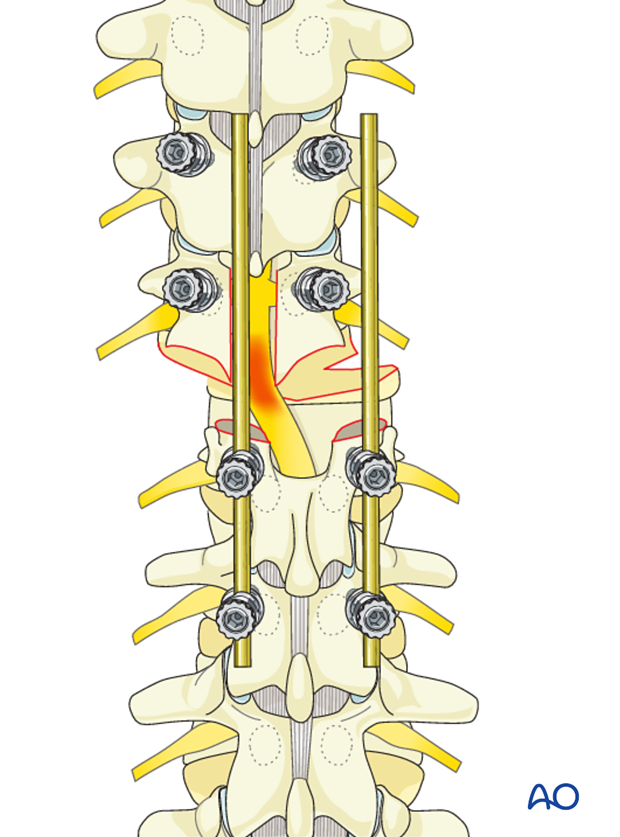
Reduction is gently achieved by the use of two rod holders, one for each rod. Force is applied in the direction of the proximal screws, which are kept in place with screw extenders.
Once the reduction is achieved with the rods inserted into the proximal screw heads, the nuts are tightened with the screw extenders.
Stability is secured, adding two cross links.
5. Fusion
Decision
Although fusion was routinely performed for all spinal fractures, its indications are now being restricted to fractures that are highly unstable.
Nonfusion fixations can be performed for A3, A4, and B1 type injuries.
Fusion is routinely performed for A2, B2, B3, and all C injuries as they are unstable injuries with extensive soft tissue and ligamentous disruption.
If the surgeon plans for a fusion, the facet capsule is excised and the joint cartilage surfaces are denuded/curetted.
Pieces of bone graft (autograft, allograft) are inserted into the decorticated facet joint for fusion.
6. Intraoperative imaging
Prior to wound closure, intraoperative imaging is performed to check the adequacy of reduction, position, and length of screws and the overall coronal and sagittal spinal alignment.
7. Aftercare for posterior procedures
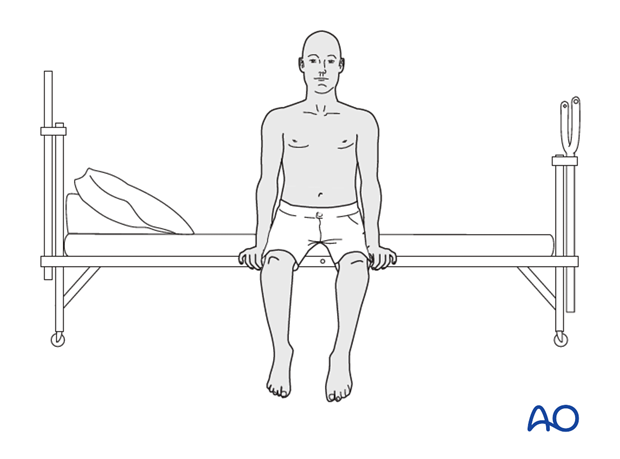
Patients are made to sit up in the bed on the first day after surgery. Bracing is optional. Patients with intact neurological status are made to stand and walk on the second day after surgery. Patients can be discharged when medically stable or sent to a rehabilitation center if further care is necessary. This depends on the comfort levels and presence of other associated injuries.
Patients are generally followed with periodical x-rays at 6 weeks, 3 months, 6 months, and 1 year. Normally, 5-10 degrees of loss of kyphosis can be observed within the first 6 months, which does not affect the functional outcomes. For nonfusion surgeries, the implants can be removed once fusion is confirmed.