MIS Anterior Stabilization
1. Preliminary remarks
In general, all surgical stabilizations for thoracolumbar spine fractures should start posteriorly.
In some cases a posterior reduction and stabilization procedure is followed by an anterior decompression and fusion when a) additional anterior column support is required or b) additional anterior decompression is indicated.
The anterior stabilization is a useful method to relieve pressure on the compromised neurological elements or to provide anterior column support. This is particularly indicated:
- If anterior spinal cord compression persists
- If residual instability persists
- If initial loss of correction occurs
- If the vertebral body is significantly destroyed and a secondary loss of correction might be anticipated
- If the disc is destroyed.
The anterior stabilization can be used as a stand-alone method.
The anterior approach should be followed by a posterior reconstructive procedure to provide further stabilization in the setting of posterior ligamentous disruption or poor bone quality (osteopenia).
Keep in mind that during additional anterior stabilization the reduction is normally limited by the posterior screw/rod system in place.
Repair of dural laceration
More details on repair of dural laceration can be found here.
2. Patient preparation and approach
T4-T10
The minimally invasive right sided thoracic approach to T4-T10 can be used together with the appropriate patient preparation.
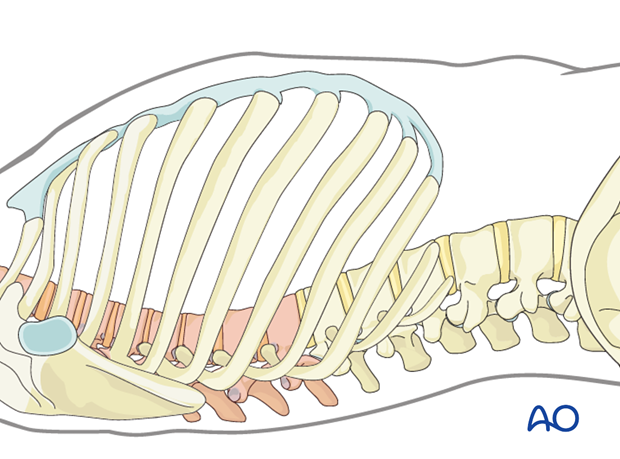
T10-L2
The minimally invasive left sided thoracic approach to T10-L2 can be used together with the appropriate patient preparation.

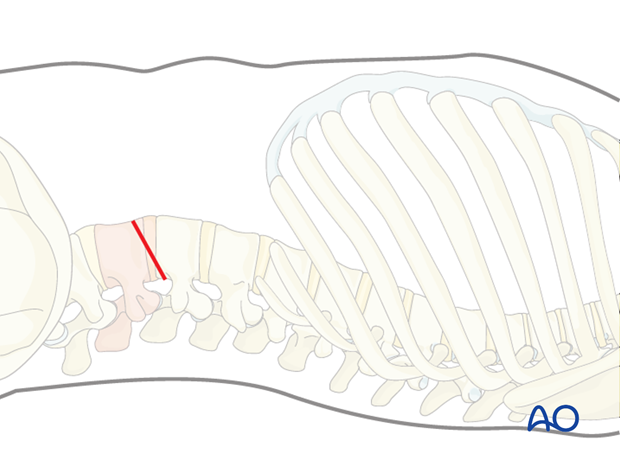
L2-L4
The minimally invasive lumbotomy approach to L2-L4 can be used together with the appropriate patient preparation.
L4-S1
The mini open retroperitoneal approach L4-S1 can be used together with the appropriate patient preparation.

3. Anterior decompression
Indications
A decompression anteriorly is usually necessary for several reasons.
The indications include:
- The presence of a traumatic disc herniation causing neurologic injury
- The need to remove a portion or entire vertebral body followed by reconstruction for stability, or for relief of symptomatic neural compression
- Ventral epidural hematoma
- Kyphotic angulation with ventral compression.
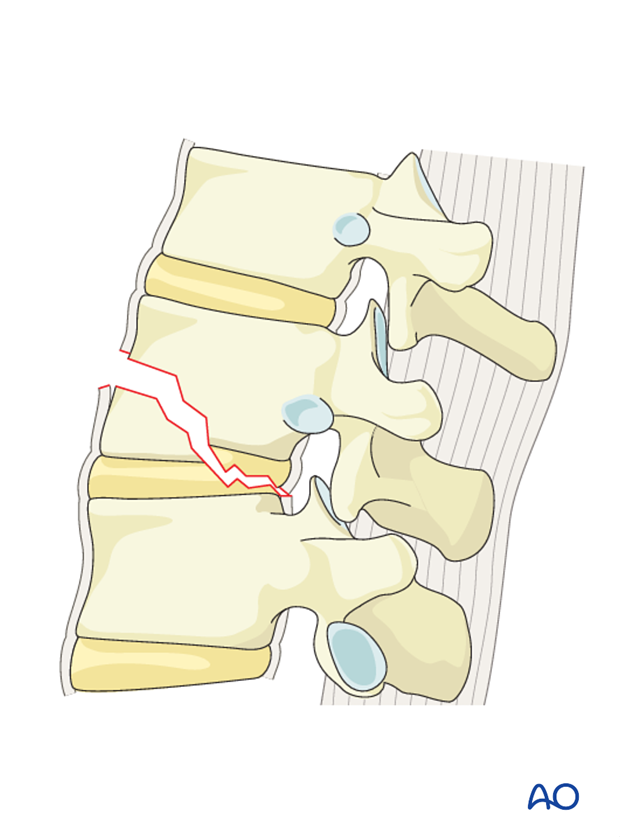
An anterior decompression can be done through a partial or total corpectomy, both including discectomies above and below the fractured vertebra.
If a vertebral body or a disc lesion compresses the spinal cord, it should be removed with the respective decompression technique.
Total corpectomy is indicated principally when there is compromise of neural structures, and a partial corpectomy is an option if the neural structures are not compromised and the goal is to achieve anterior column reconstruction.
Surgical step 1: Discectomy
Discectomy always precedes corpectomy, because it allows the surgeon to visualize the upper and lower limit of the spinal canal.
In the case of a partial corpectomy, discectomy is done for the disc adjacent to the fractured end plate.
For a complete corpectomy, discectomy is done both above and below that fractured vertebra.
The procedure should be done with adequate light and magnification, either loupes or an operating microscope.
Technique
A traumatic disc herniation in the thoracic spine is removed by firstly identifying the rib head.
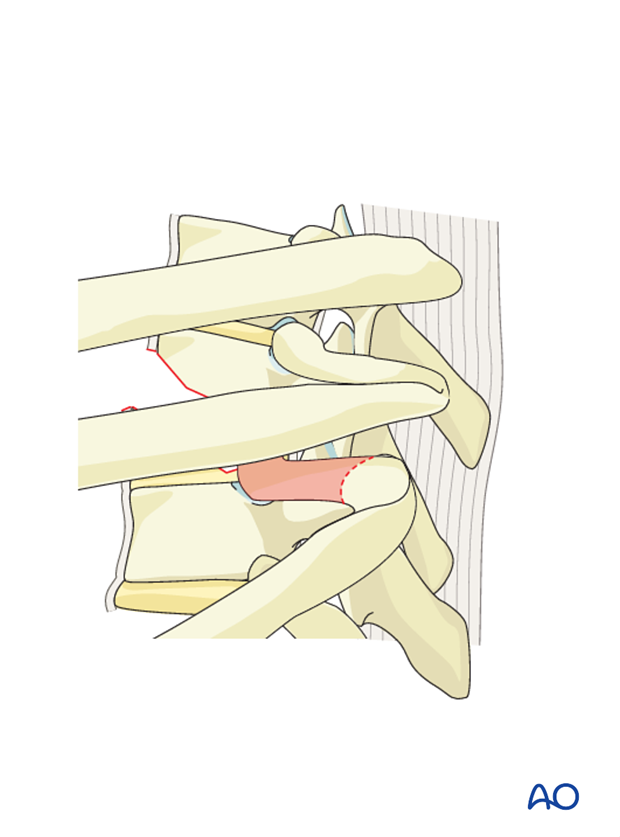
In cases where it is necessary to decompress the spinal cord, it may be necessary to remove the rib head and pedicle to identify the spinal canal.
In this case, the rib head is removed with a burr or osteotome.
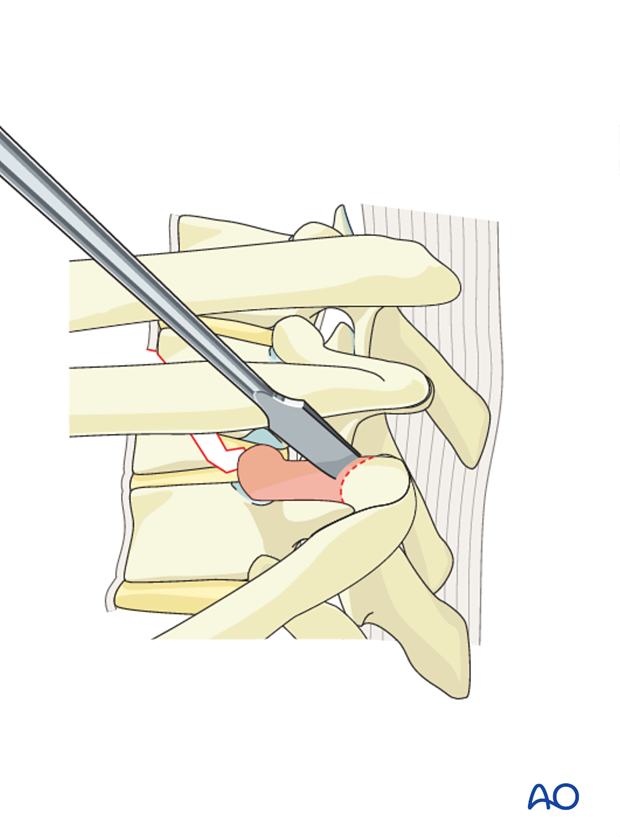
Once the rib head is removed, the bony pedicle below is identified.
The pedicle is removed with a high speed burr and Kerrison rongeur. This allows identification of the exiting nerve root and location of the dural tube.
Attention is now given to the disc itself. A bony opening is created in the shape of a triangle where the larger base is located adjacent to the spinal canal, removing a portion of the respective endplates above and below the disc.

The disc and adjacent endplates are evacuated into the created void followed by the posterior vertebral wall and disc within the spinal canal. This allows minimal if any manipulation of the spinal cord.
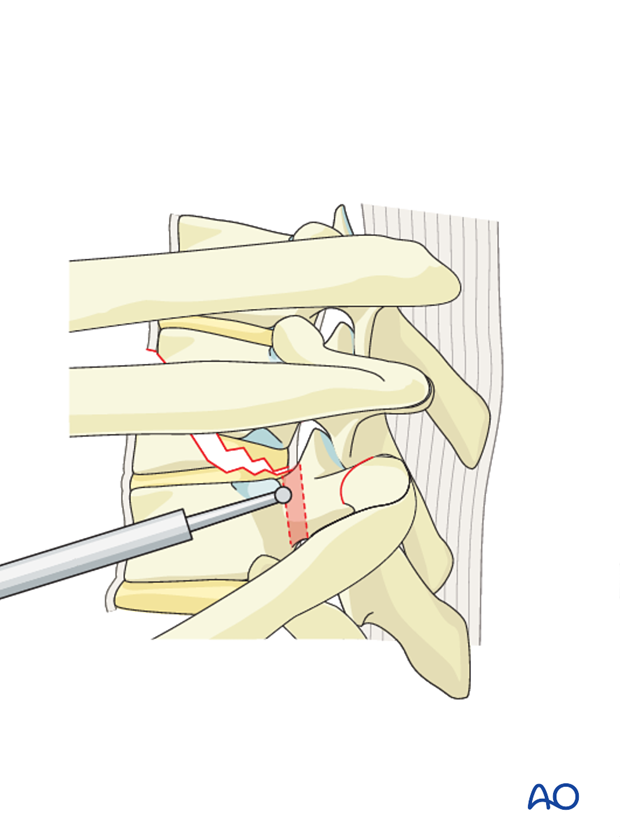
In the thoracolumbar/ lumbar spine, the disc is often removed by incising the anulus fibrosis and using a series of Kerrison rongeurs and curettes back to the posterior anulus and posterior longitudinal ligament.
This is often performed as part of a corpectomy or partial corpectomy in the setting of a traumatic burst fracture.
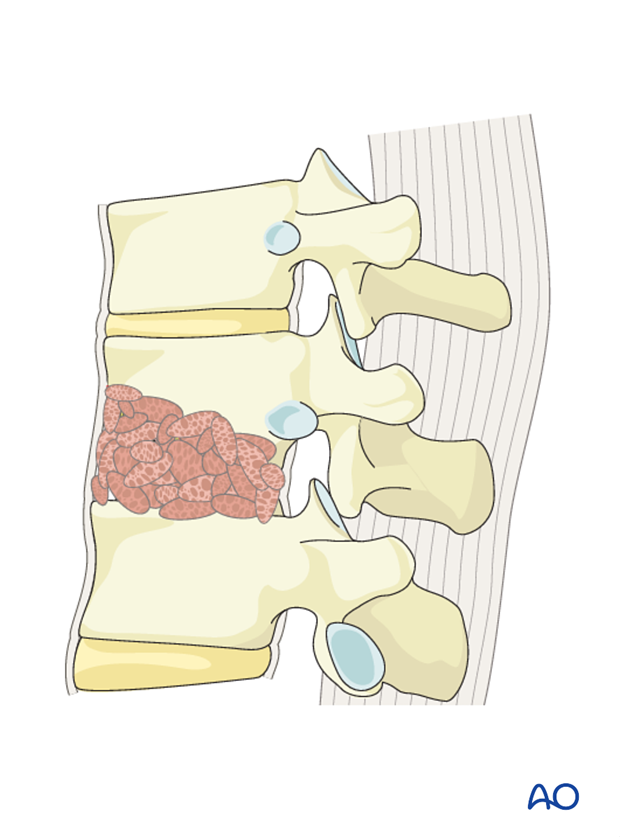
Surgical Step 2 - Corpectomy
In a second surgical step, a total or a partial corpectomy is undertaken.
Total corpectomy
A corpectomy involves removal of the entire vertebral body and adjacent discs.

Technique
Before doing a corpectomy, the segmental vessels have to be identified. Sometimes, the vessels are already disrupted due to trauma.
After identifying the segmental vessels, these should be ligated in the mid vertebral body away from the neural foramen.
Note: There is no segmental artery in L5.

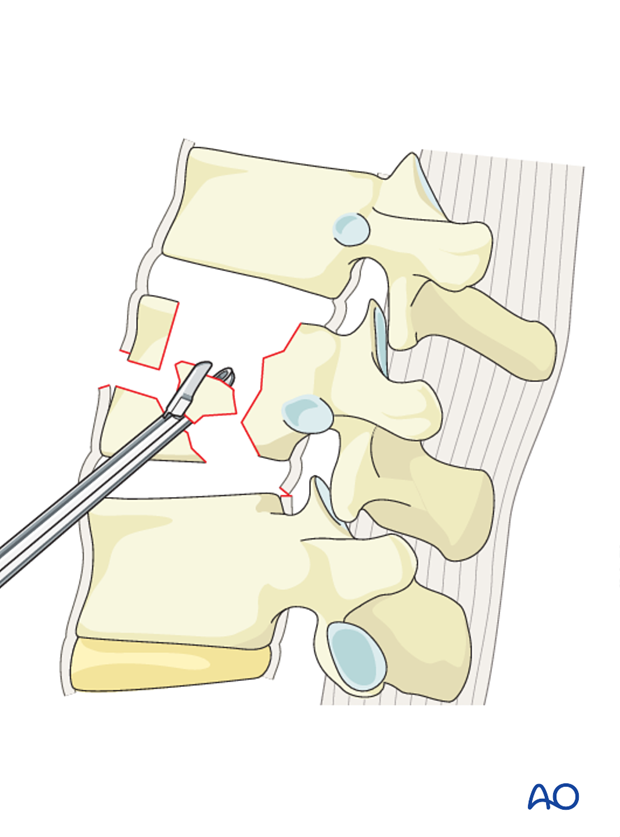
After removal of the rostral and caudal discs as described in the discectomy section, the fractured portion of the vertebral body (but not the posterior third) is removed using a combination of Leksell rongeurs and osteotomes.
A rim of vertebral body is left anteriorly to facilitate fusion.
A burr is used to remove the posterior portion of the vertebral body as the spinal canal is approached.
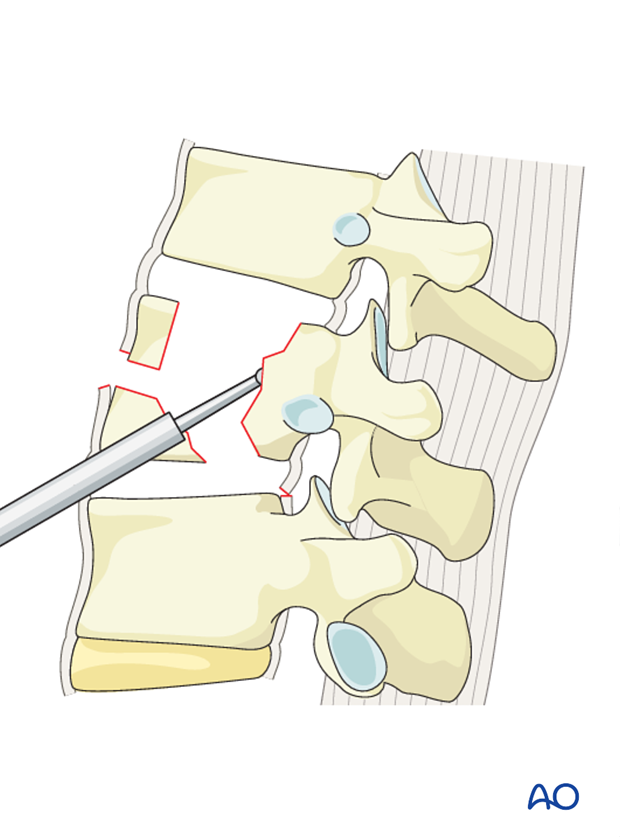
The spinal canal is decompressed by the resection of the posterior wall of the vertebral body.
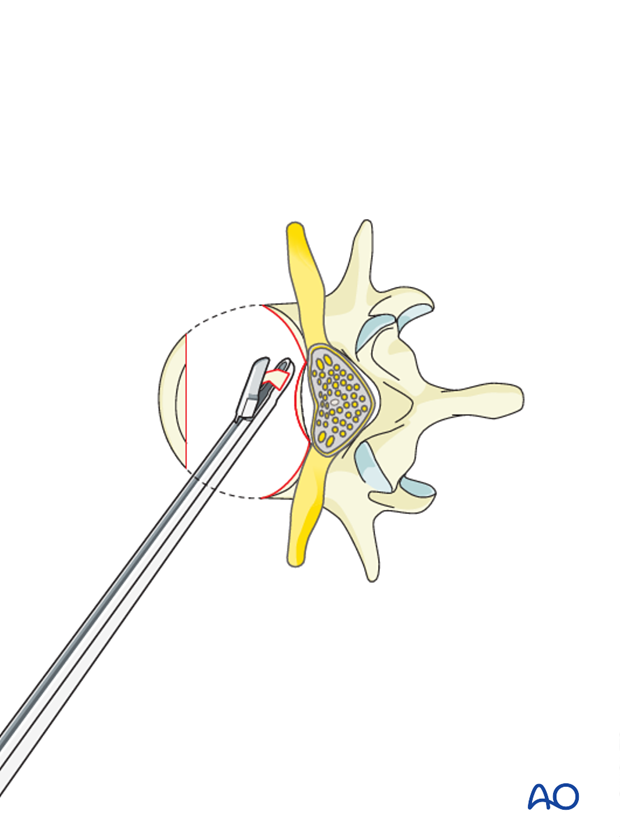
The posterior cortex should be thinned with the burr to an eggshell. Retropulsed bone fragments can be removed with curettes and thin footplate Kerrison punches.
This is optimally done with a high speed burr and curettes under loupe or microscopic magnification.
Pearl: protection of the dura
Care should be taken to protect the dura. Epidural venous bleeding can be troublesome at times, so meticulous hemostasis with bipolar cautery, cottonoid patties, and hemostatic adjuncts can be helpful.
Surgical Step 2 - Corpectomy: Partial corpectomy
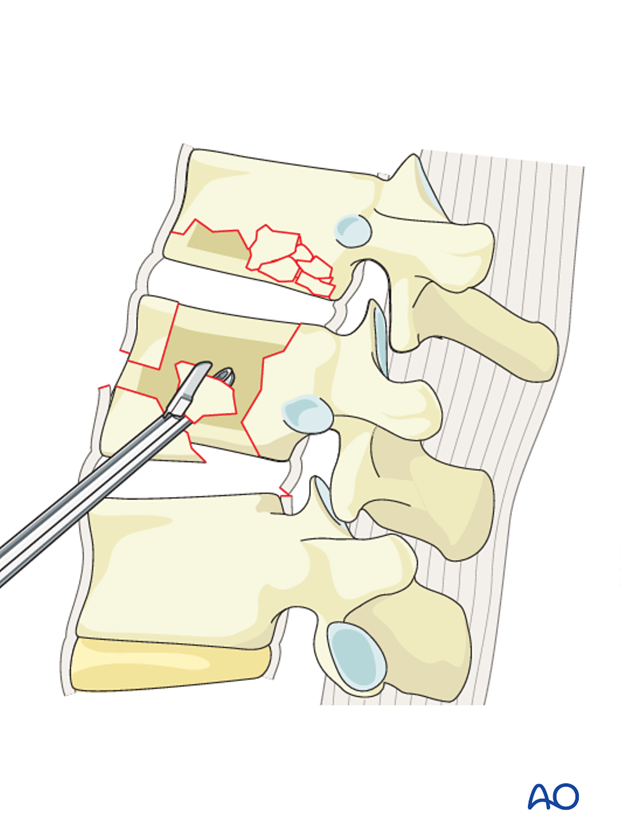
A partial corpectomy involves removal of the fractured superior or inferior vertebral body and adjacent disc.

Technique
Before doing a partial corpectomy, the segmental vessels have to be identified. Sometimes, the vessels are already disrupted due to trauma.
After identifying the segmental vessels, these should be ligated in the mid vertebral body away from the neural foramen.
Note: There is no segmental artery in L5.

After removal of the of the disc adjacent to the fractured endplate as described in the discectomy section, the fractured portion of the vertebral body (but not the posterior third) is removed using a combination of Leksell rongeurs and osteotomes.
A rim of vertebral body is left anteriorly to facilitate fusion.
A burr is used to remove the posterior portion of the vertebral body as the spinal canal is approached.
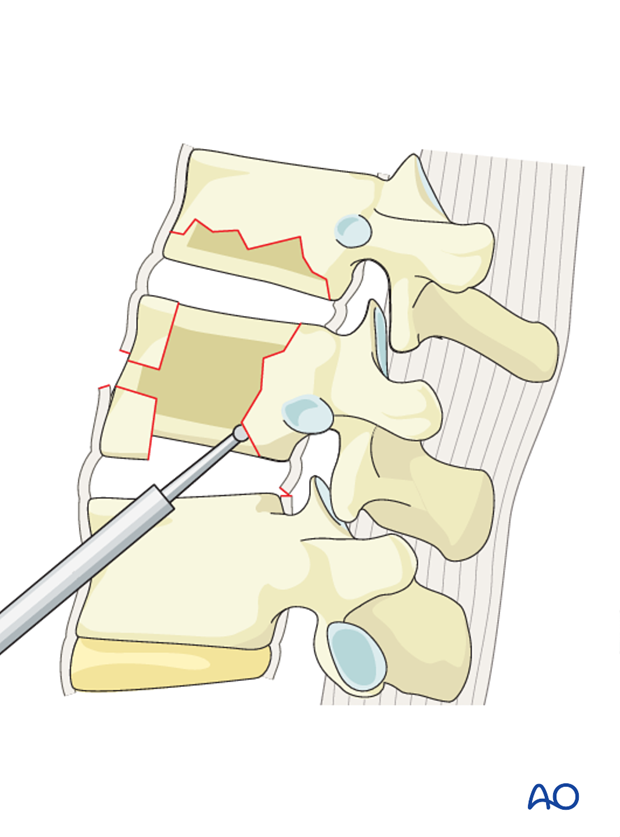
If necessary, the spinal canal is decompressed by the resection of the posterior wall of the vertebral body.
The posterior cortex should be thinned with the burr to an eggshell. Retropulsed bone fragments can be removed with curettes and thin footplate Kerrison punches.
This is optimally done with a high speed burr and curettes under loupe or microscopic magnification.

Pearl: protection of the dura
Care should be taken to protect the dura. Epidural venous bleeding can be troublesome at times, so meticulous hemostasis with bipolar cautery, cottonoid patties, and hemostatic adjuncts can be helpful.
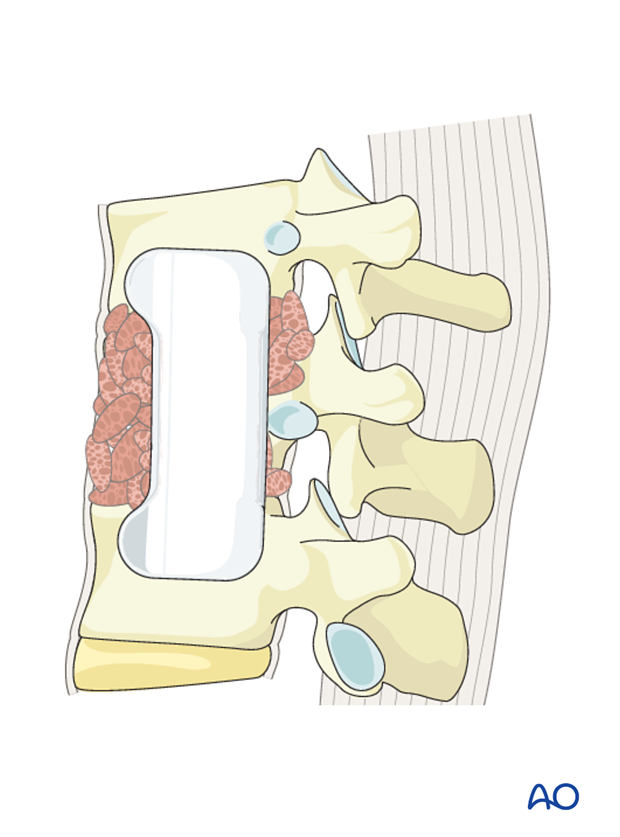
4. Reconstruction
Total corpectomy
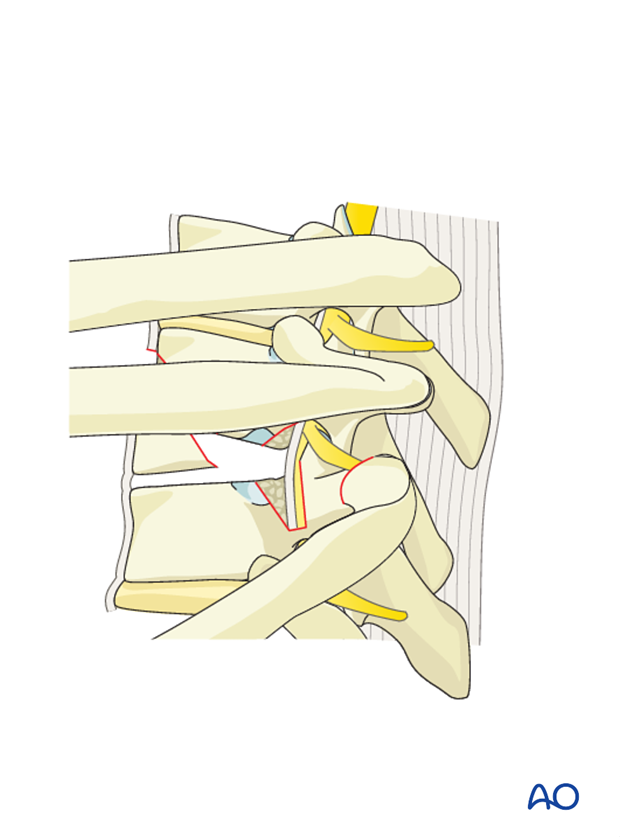
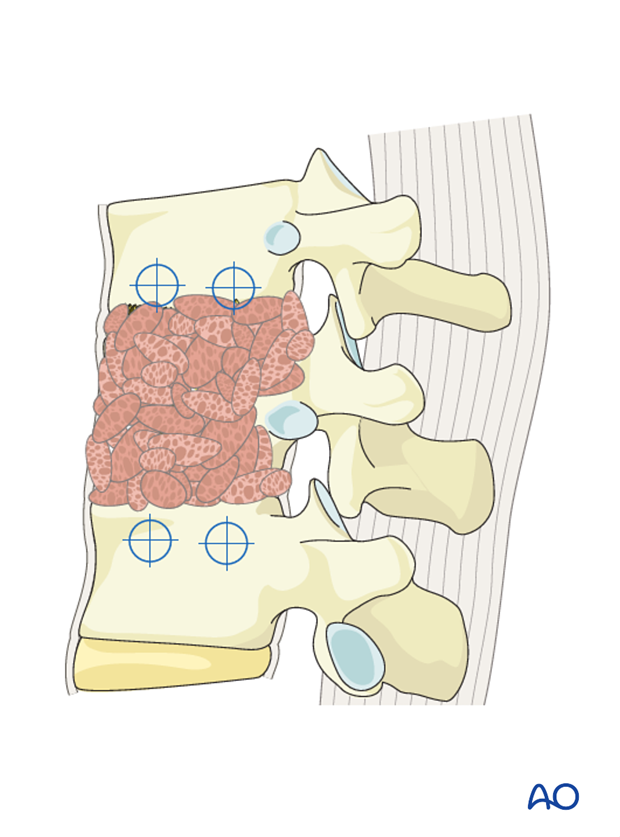
Anterior reconstruction of the disc space or vertebral body following a complete corpectomy can be performed using an autograft or allograft, strut graft, or a synthetic or metallic cage (expandable or non expandable).
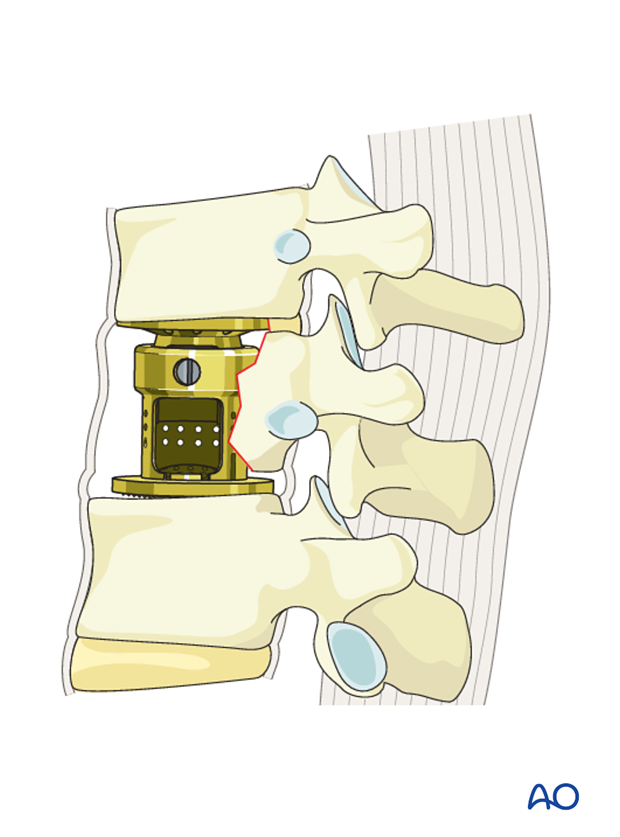
Additional bone grafting can be used from the corpectomized vertebral body and the removed rib.
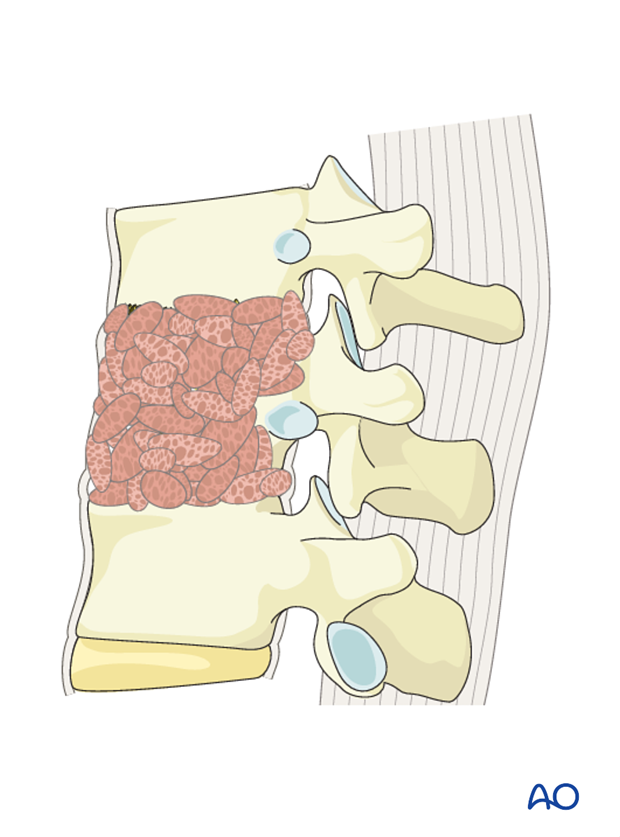
Partial corpectomy
The anterior reconstruction of the vertebral body is performed using a mesh or tricortical iliac crest bone graft.
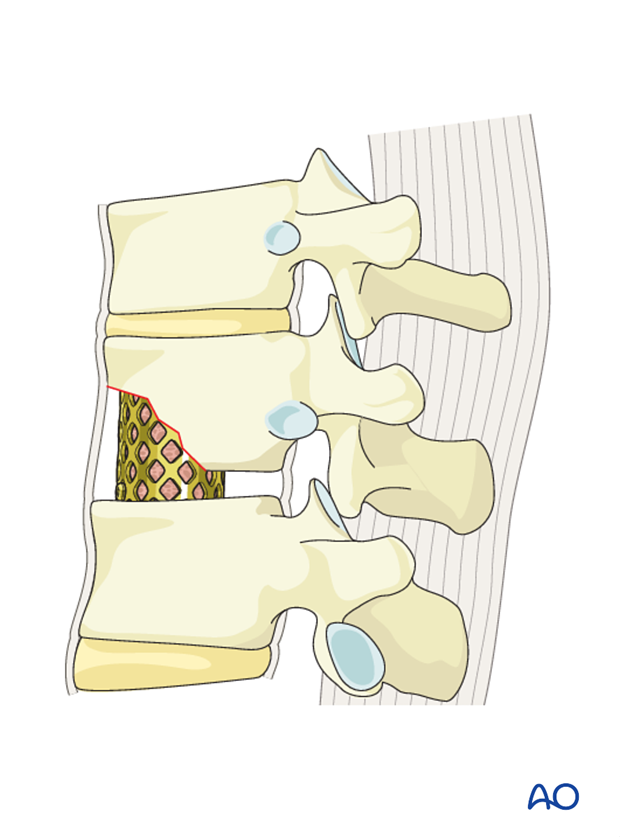
The bone graft stemming from the vertebral body is transplanted to bridge the segment.
5. Stabilization
Introduction
After reconstruction, the construct has to be further stabilized.
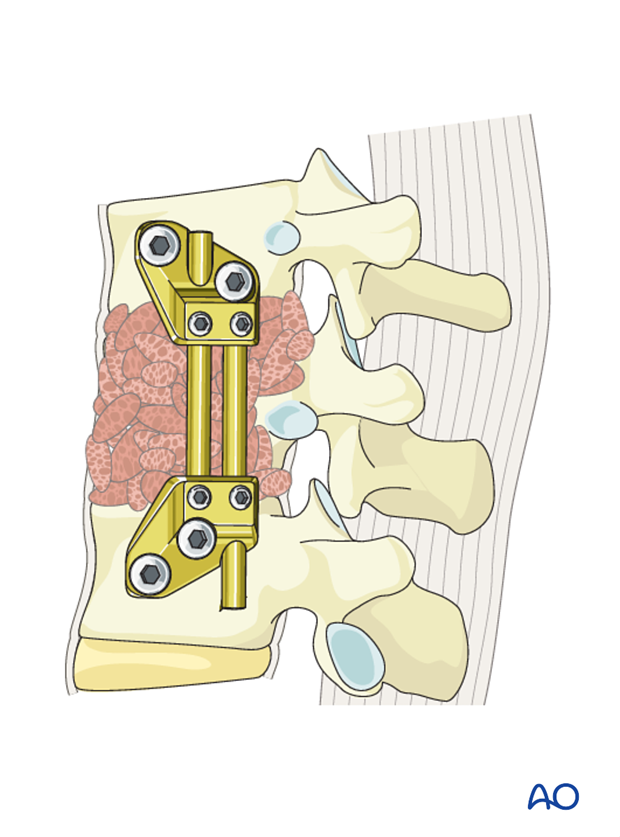
Anterior plating
Various plating systems are available for this purpose eg:
- Screw first systems (typically MIS)
- Plate first systems (typically open systems)
Plate specific reduction options:
- Fixed systems
- Distractible systems
- Lordotic systems.
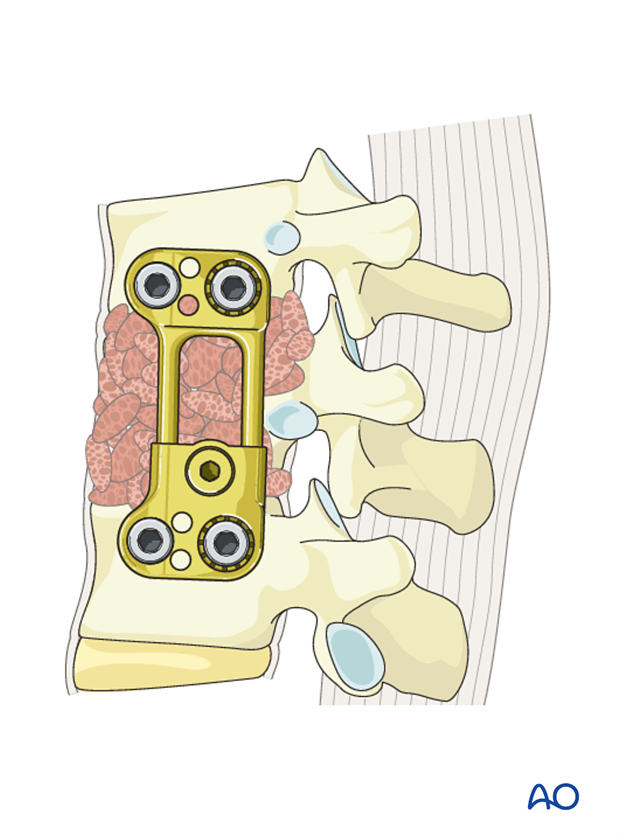
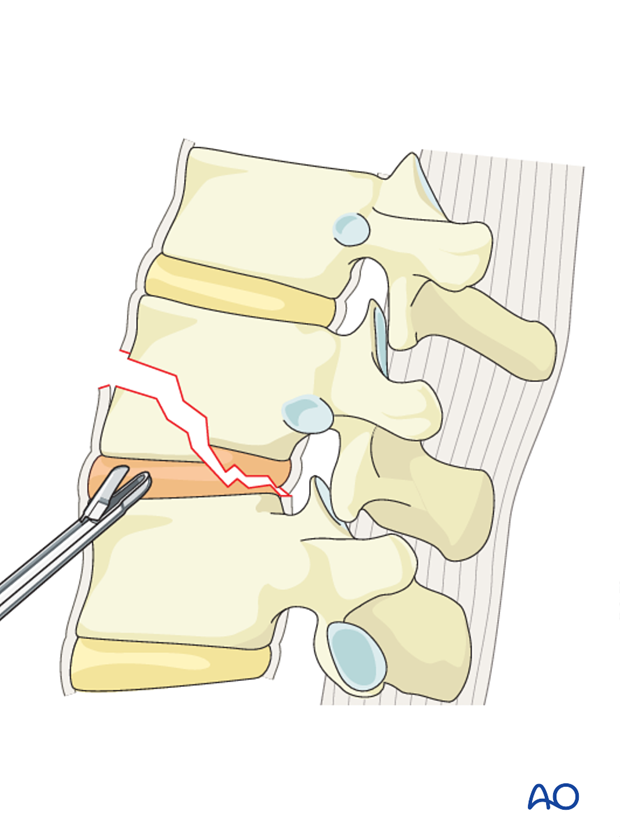
Application of plate instrumentation
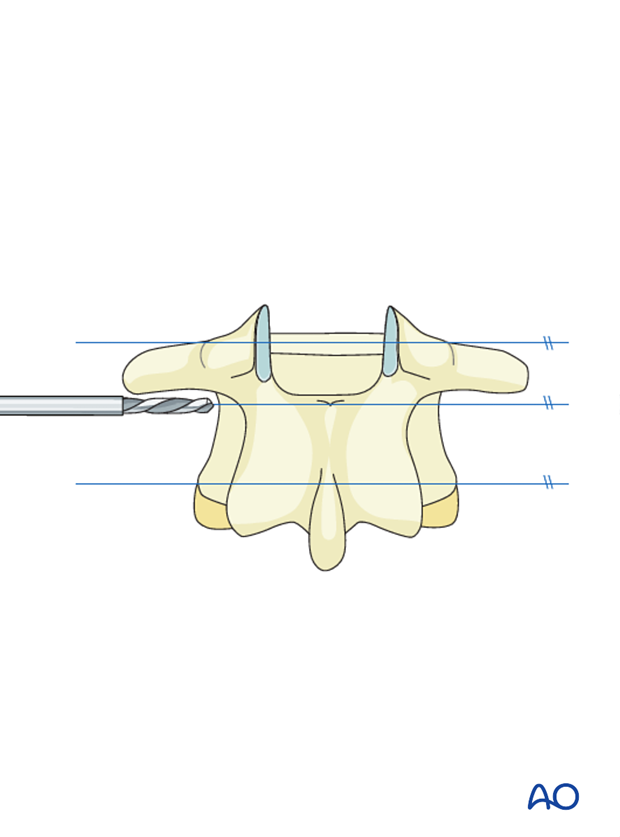
The appropriate size plate is chosen by using a measuring forceps to determine plate length.
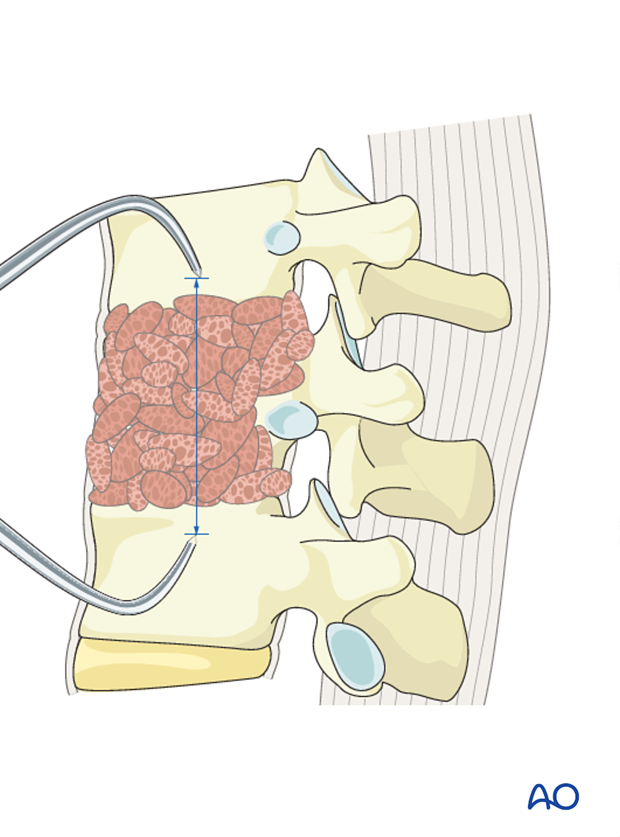
A plating template is then applied to the remaining vertebral bodies to make sure the plate fits flush on the bone.
A drill guide is used to drill holes within the vertebral body.
Pearl: Screw path
Make sure that the screw path is parallel to the vertebral endplates and the screw path does not violate the spinal canal.
The screws are then placed affixing the plate to the vertebral bodies. A variety of plating systems allow for distraction or compression.
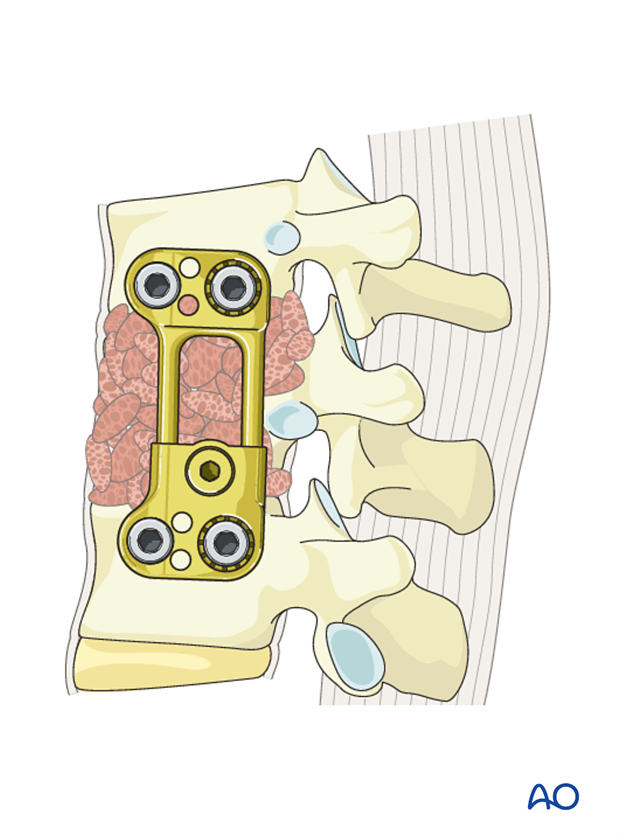
Pearl: Plate position
It is important to make sure the plate is as posterior as possible to avoid impingement on any vascular structure.
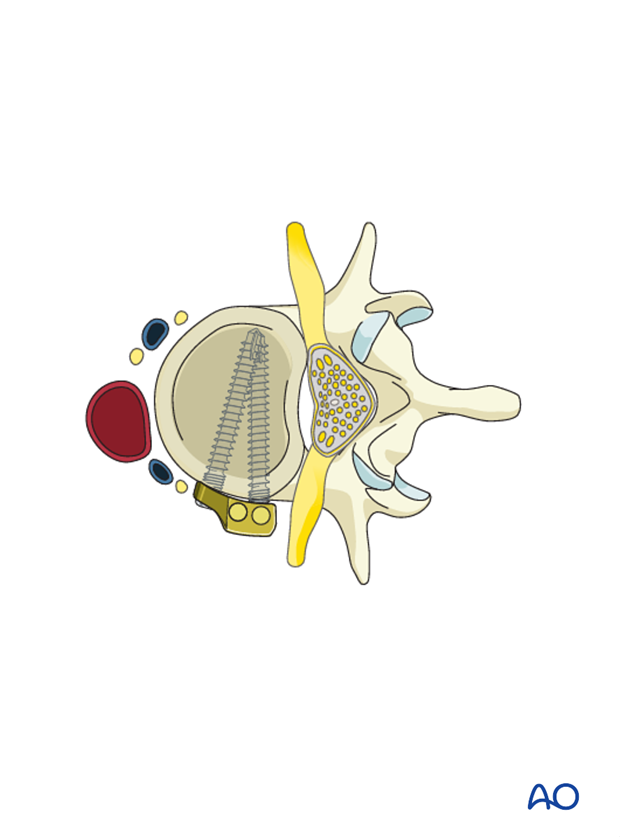
Anterior rod screw system
Another form of anterior instrumentation is using a single rod construct after placing a strut graft with a bone screw above and below the fusion site. Some fixation systems are designed to place two rods in parallel to one another to provide the potential for standalone anterior fixation.
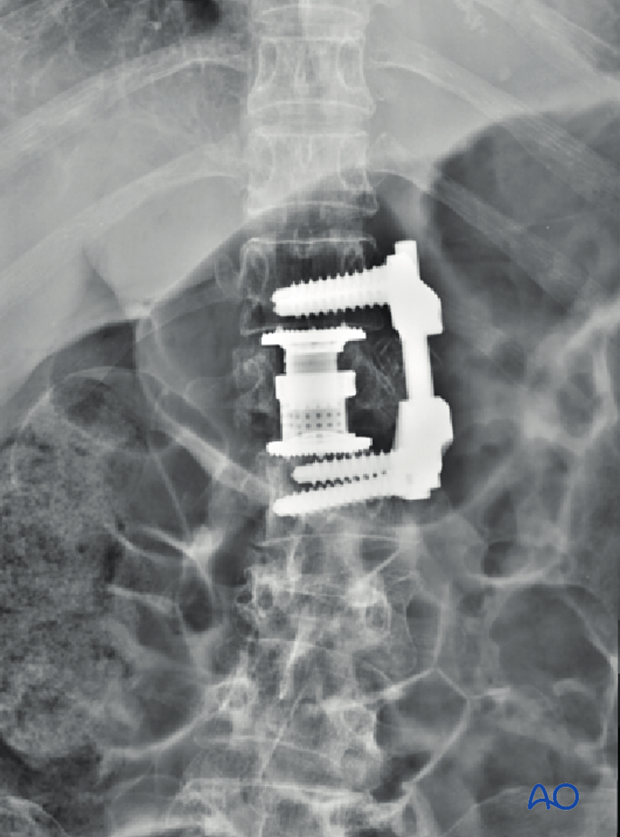
6. Intraoperative imaging
Prior to wound closure, intraoperative imaging is performed to check the adequacy of reduction, position, and length of screws and the overall coronal and sagittal spinal alignment.
7. Aftercare for anterior procedures
Patients are made to sit up in the bed on the first day after surgery. Bracing is optional. Patients with intact neurological status are made to stand and walk on the second day after surgery. Patients can be discharged when medically stable or sent to a rehabilitation center if further care is necessary. This depends on the comfort levels and presence of other associated injuries.
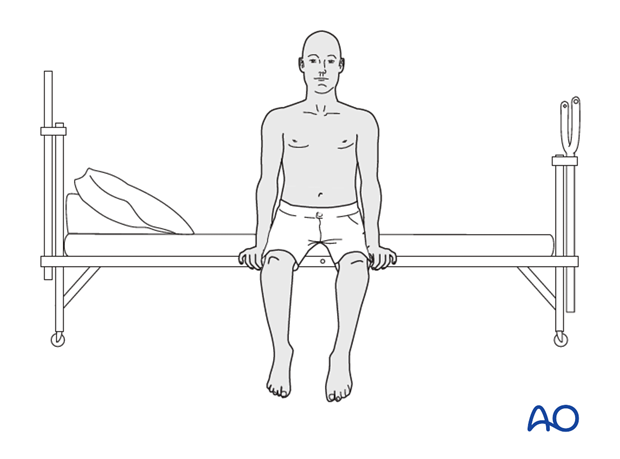
Patients are generally followed with periodical x-rays at 6 weeks, 3 months, 6 months, and 1 year.














