Minimally invasive left sided thoracic approach (T10-L2)
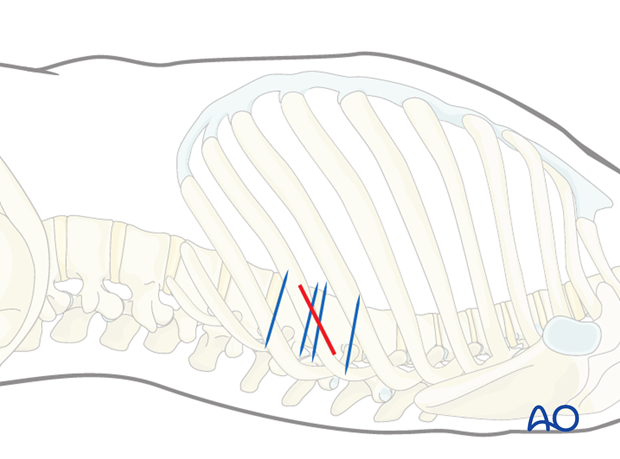
1. Portal site
The exact portal site will depend on the level of the fracture. In general, the right sided approach is for fractures between T4 and T10 and the left sided approach is for T10 to L2, depending on the vascular anatomy (location of the aorta).
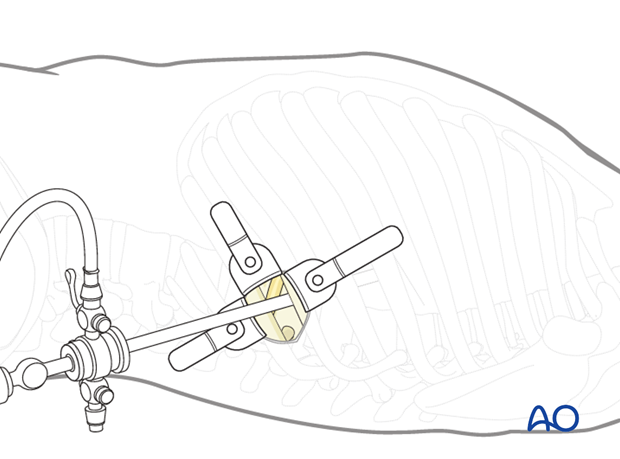
For minimally invasive surgery, specific instruments and implants are needed. A self-retaining retractor system is necessary to allow the exposure of the spine.
It is necessary to confirm the correct level of the approach with fluoroscopy.

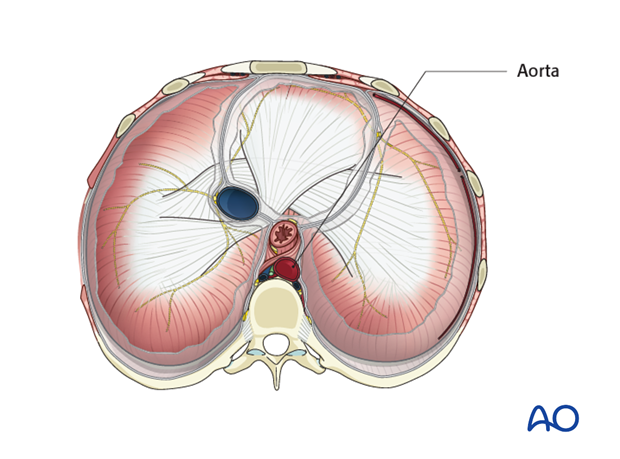
2. Pearl: Location of the aorta
In the lower thoracic spine (T8-T10), right and left sided approaches are possible. A thorough examination of the location of the aorta allows the choice of the optimal approach side.
3. Options
There are two options to carry out a minimally invasive left sided thoracic approach. The minimally invasive thoracoscopically assisted thoracotomy and the fully video assisted thoracoscopy.
The video assisted thoracoscopy (VAT) is predominantly used in noninstrumented cases, while the miniopen thoracoscopically assisted thoracotomy is ideal in instrumented cases.
4. Option 1: Minimally invasive thoracoscopically assisted thoracotomy
First, the minimally invasive thoracoscopically assisted thoracotomy is described.
5. Preparation
Under fluoroscopic control, the fractured vertebra or injured disc and the adjacent segments are marked on the skin of the left thoracic side.
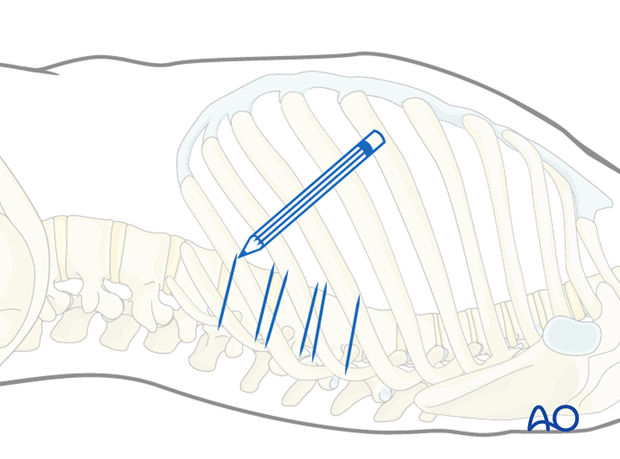
If bisegmental stabilization is to be performed, the incision runs from the posterior edge of the lower end plate of the vertebral body above the fracture to the anterior edge of the upper endplate of the vertebral body below the fracture.
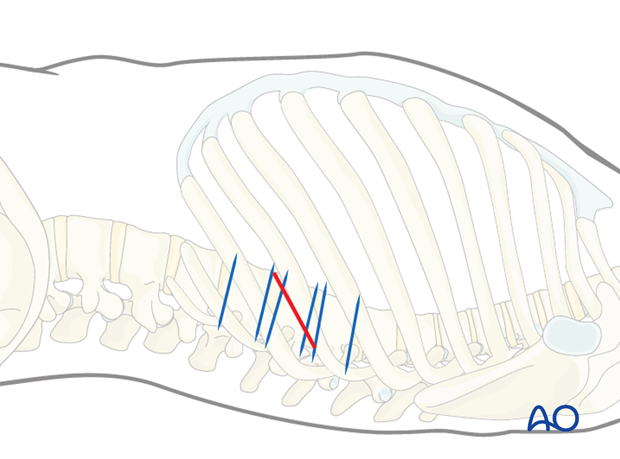
If monosegmental stabilization is to be performed, the incision runs from the midpoint of the posterior wall of the vertebral body above the fracture to the midpoint of the anterior wall of the vertebral body below the fracture.
6. Minithoracotomy
The skin is incised on the mark.
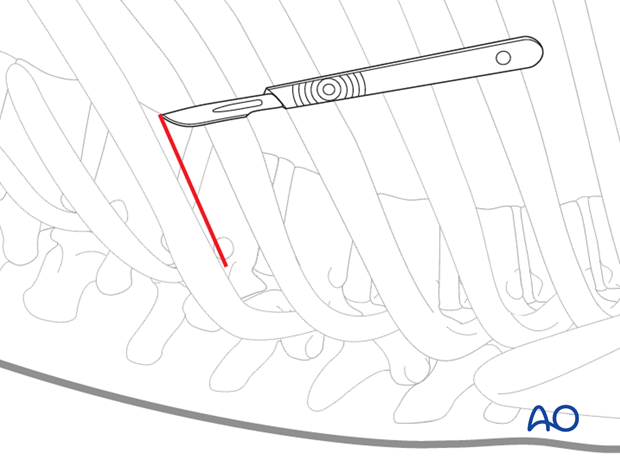
The skin and subcutaneous tissues and overlaying muscles are incised in line with the incision down to the rib to be exposed.
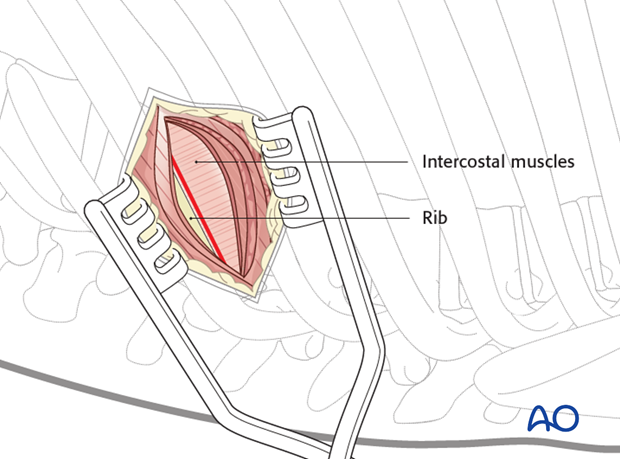
After exposing the rib, the intercostal muscles are dissected from the cranial part of the rib.
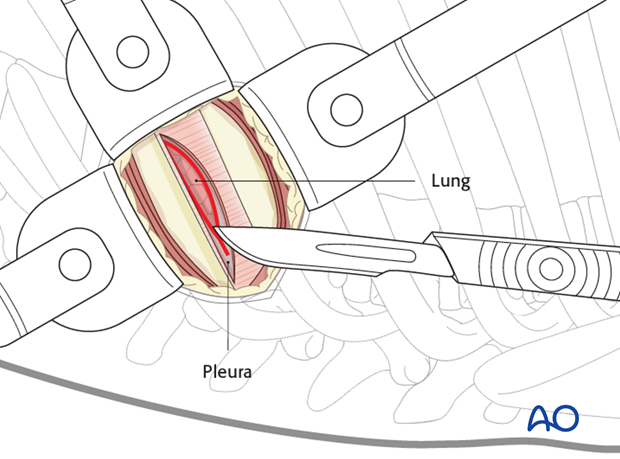
The pleura is then cut to allow entry into the chest without injuring the lung. A rib spreader can be used to gradually open the space created.
7. Additional portals
The thoracoscope is inserted through the minithoracotomy and a VAT is performed of the entire thorax.
This is done to examine the chest cavity for adhesions or anatomical variations prior to preparation of any further portals.
The other portals are placed under thoracoscopic control.
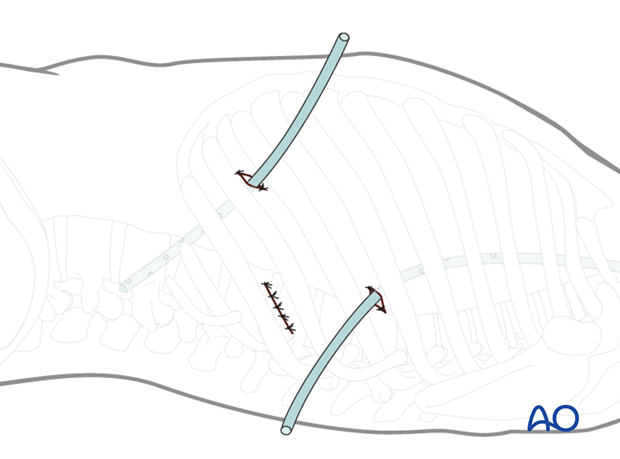
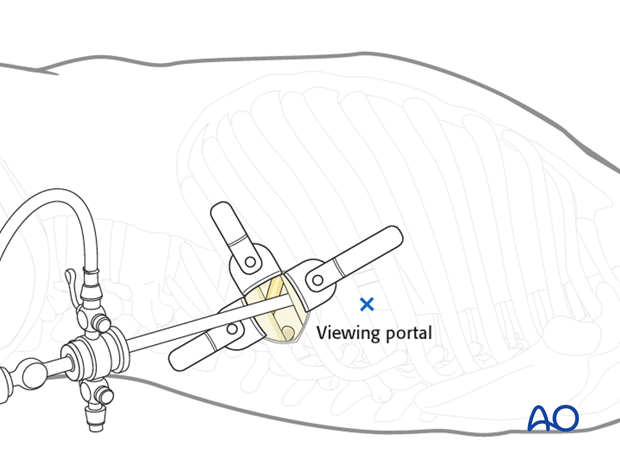
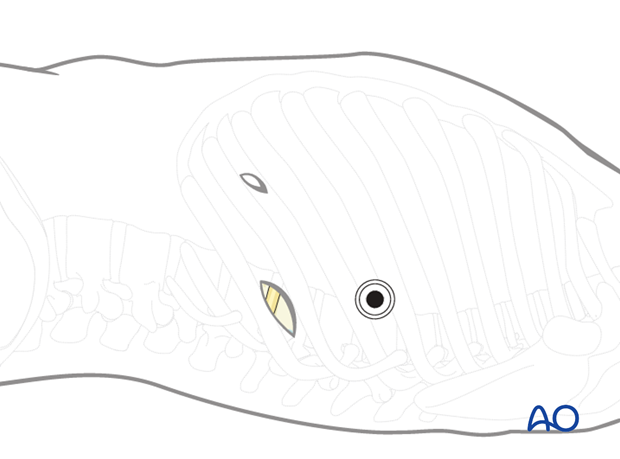
8. Portals
The viewing portal is marked first, two intercostal spaces cranial to the minithoracotomy at the anterior edge of the vertebral body.
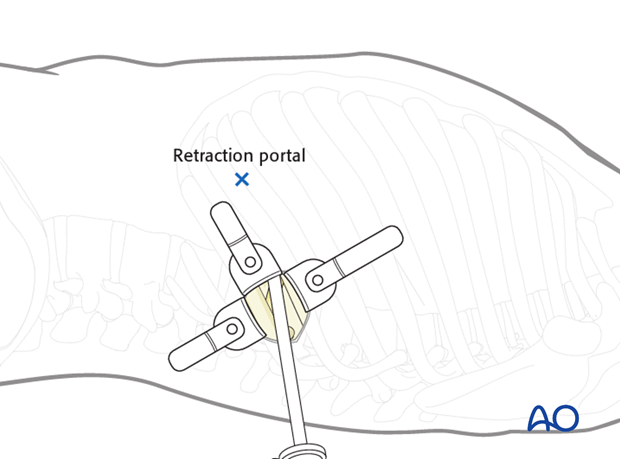
The retraction portal is marked one intercostal space cranial to the minithoracotomy and approximately 10 cm anteriorly.
9. Incisions for the portals
A 20 mm skin incision is made for all portals. The incisions are deepened by sharp dissection to the pleural cavity at the upper rim of the rib to avoid injury to the intercostal vessel and a finger is introduced into the chest cavity to check for adhesions.
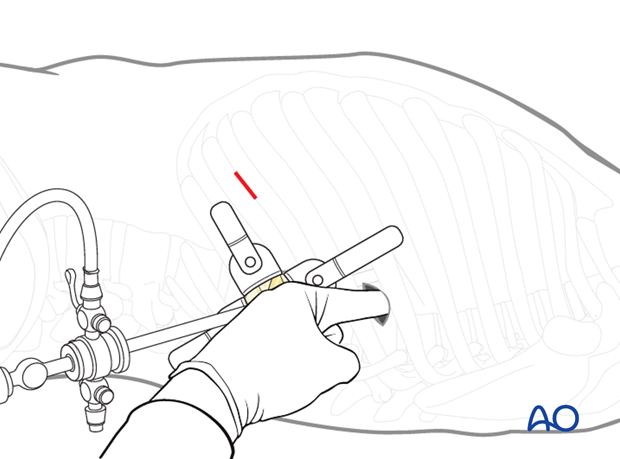
A blunt trocar is introduced under thoracoscopic control.
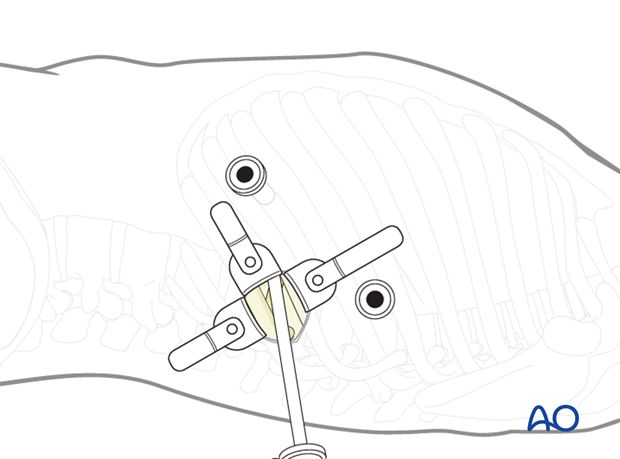
Now, the thoracoscope is retracted from the minithoracotomy and inserted into the viewing portal.
The retractor is inserted through the retractor portal.
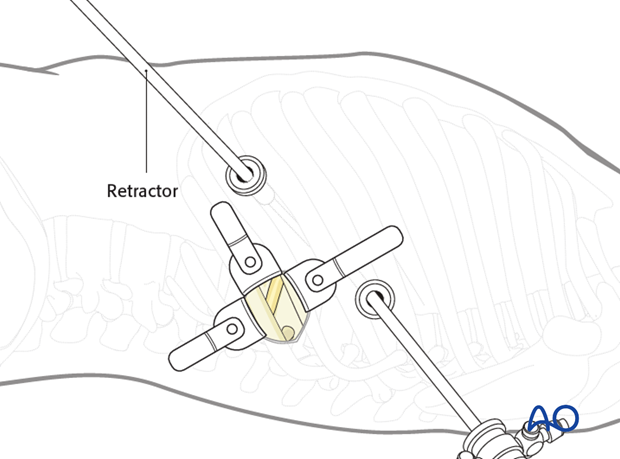
The self-retaining retractor system can now be used to expose the spine.
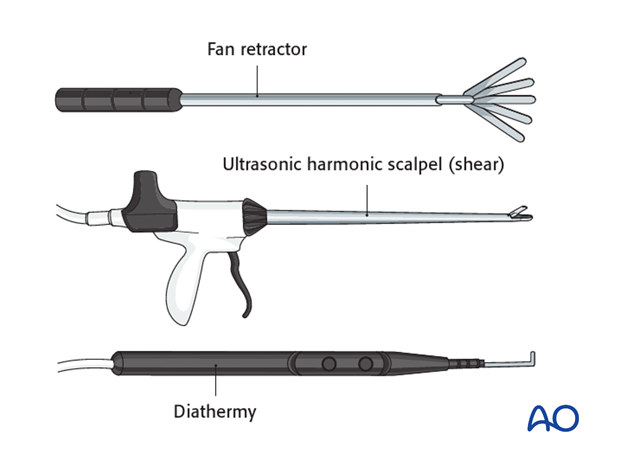
10. Instruments for miniopen and thoracoscopic approaches
Specialized long instruments are needed for dissection. As an example, a fan retractor can be used to carefully hold the lung or diaphragm tissue away from the vertebrae.
An ultrasonic harmonic scalpel or shears are very useful tools for both cutting and coagulating tissues if available. An alternative would be a long hook shaped diathermy tip.
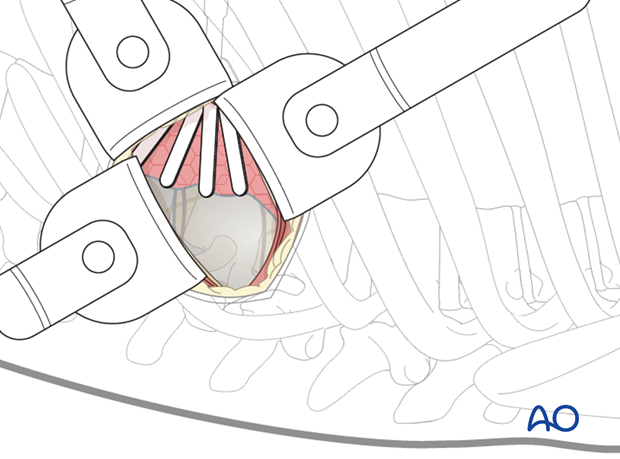
11. Further dissection
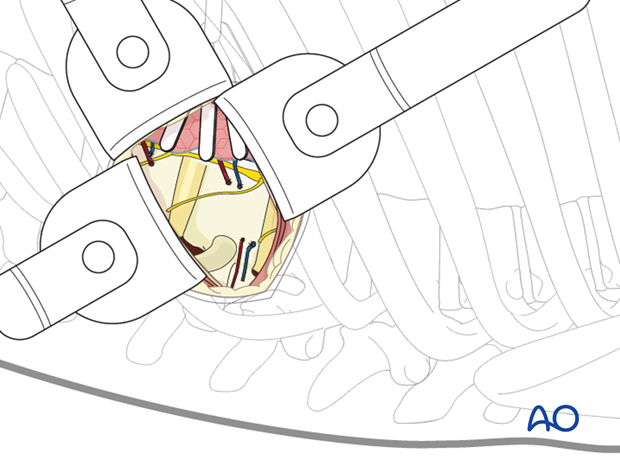
The parietal pleura should be opened longitudinally over the spine at the fracture level and a level above and below. It is easiest to begin the dissection at the discs, which will appear as avascular "hills". The "valleys" are the vertebral bodies, and the segmental vessels are in the midline.
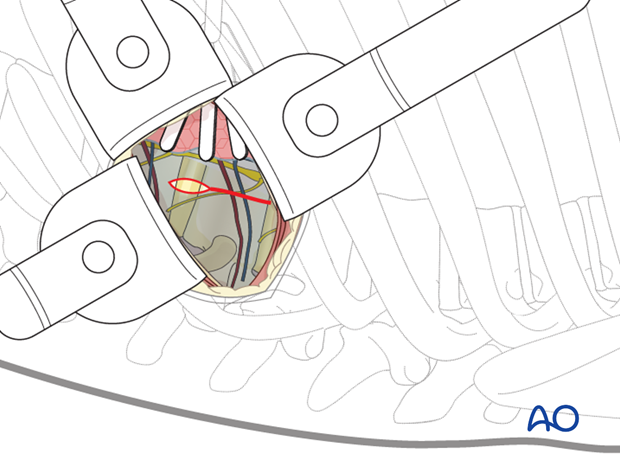
The segmental vessels running along the vertebral bodies are identified. For anterior discectomies, these can be spared. For instrumentation they will need to be coagulated either by harmonic shears or by diathermy.
A subperiosteal exposure is then undertaken to the level of the anterior longitudinal ligaments with protection of the great vessels.
Posteriorly the dissection should expose the heads of the ribs.
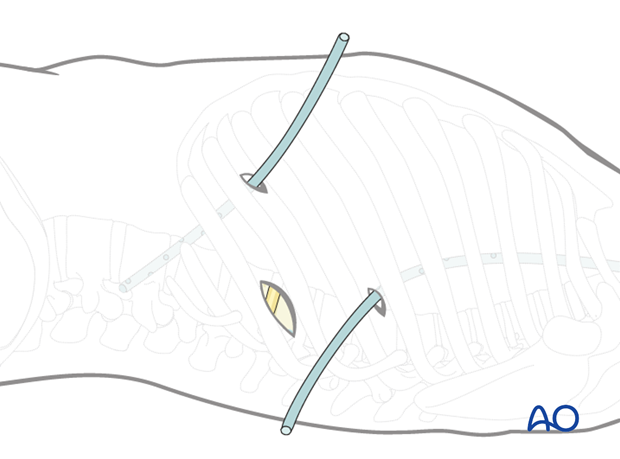
12. Option 2: Fully Video Assisted Thoracoscopy (VAT)
Second, the VAT is described.
For fully thoracoscopic approaches, which are even less invasive, the minithoracotomy can be replaced by two additional portals for thoracoscopic instruments. One portal is located directly above the pathology (A) and the second one in between the viewing and the retraction portal (B).
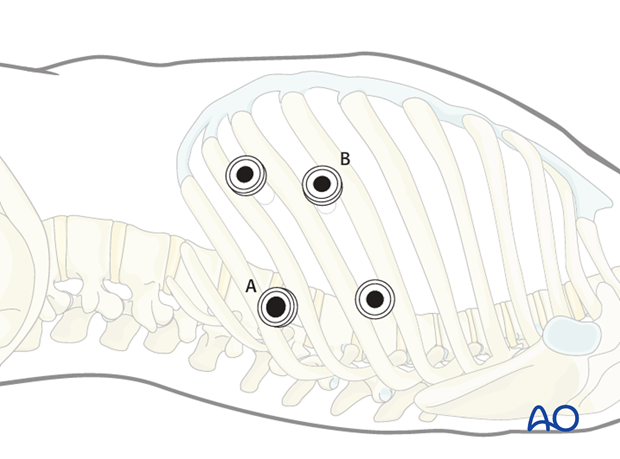
The VAT is predominantly used in noninstrumented cases, while the mini open thoracoscopically assisted thoracotomy is ideal in instrumented cases.
13. Closure
If possible, the parietal pleura should be sutured.
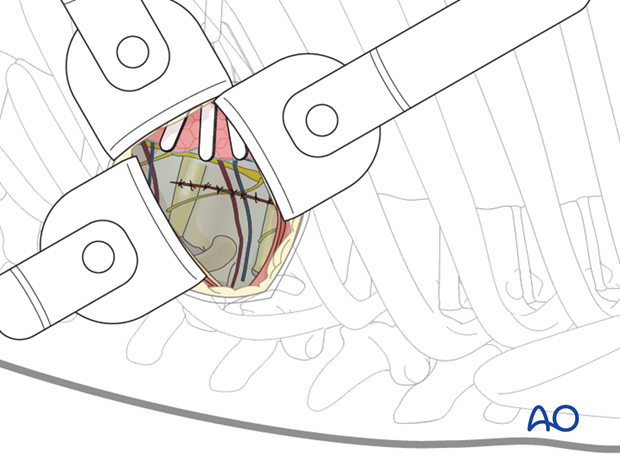
The viewing portal should be removed last to allow a direct inspection of the pleural cavity. The anesthesiologist should be asked to fully inflate the lung, which can be checked with the thoracoscope.
Two chest drains are then inserted. One via the viewing portal, which is directed to the cranial anterior part of the thoracic cavity (pneumothorax drain). The second one is placed in the retraction portal to the caudal posterior part of the thoracic cavity (wound drain).
The portals and the minithoracotomy are then closed in layers.