Minimally invasive lumbotomy (L2-L4)
1. Approach
The left-sided approach is more common and therefore described below.
A right sided approach is in general possible, but very rarely used.
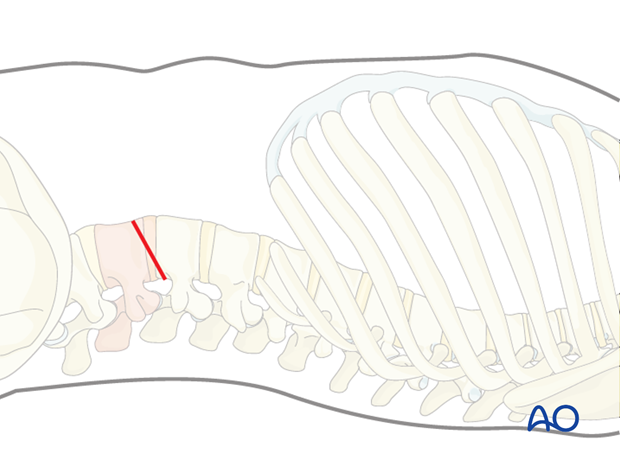
2. Portal site
The exact portal site will depend on the level of the fracture. The disc space L5/S1 cannot be reached with this approach.
For minimally invasive surgery, specific instruments and implants are needed. A self-retaining retractor system is necessary to allow the exposure of the spine.
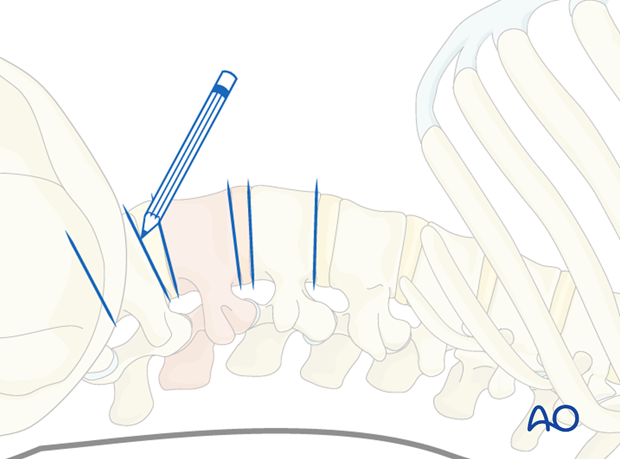
It is necessary to confirm the correct level of the approach with fluoroscopy.
3. Application
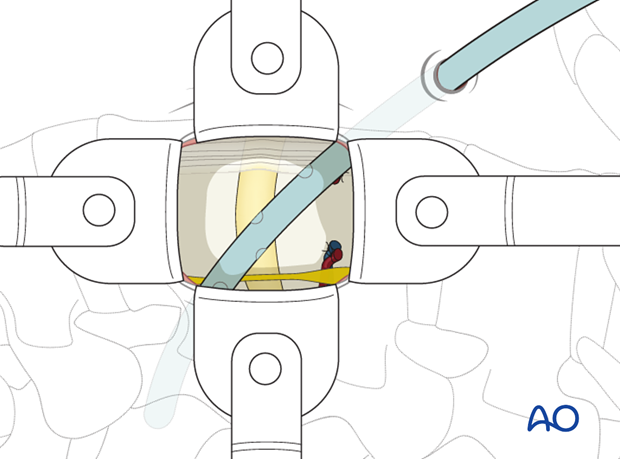
The minimally invasive lumbotomy is ideal for plating. The minimally invasive retroperitoneal approach is excellent for vertebral body replacement.
4. Preparation
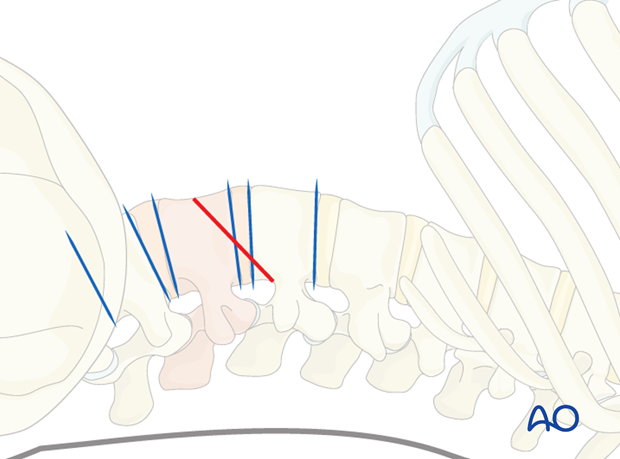
Under fluoroscopic control, the fractured vertebra or injured disc and the adjacent segments are marked on the skin.
If bisegmental stabilization is to be performed, the incision runs from the posterior edge of the lower end plate of the vertebral body above the fracture to the anterior edge of the upper endplate of the fractured vertebra.
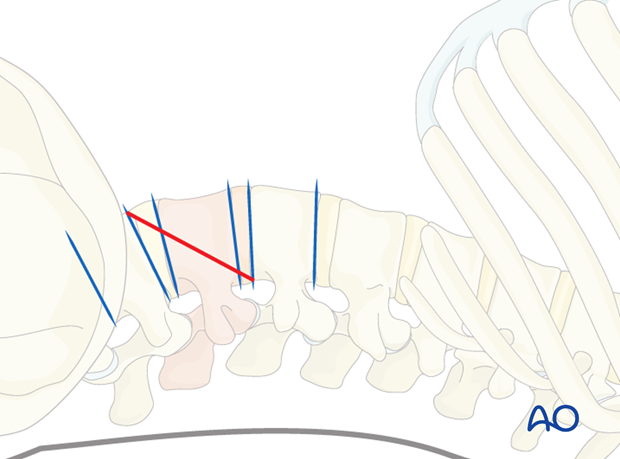
If a monosegmental stabilization is to be performed, the incision runs from the midpoint of the posterior wall of the vertebral body above the fracture to the midpoint of the anterior wall of the vertebral body below the fracture.
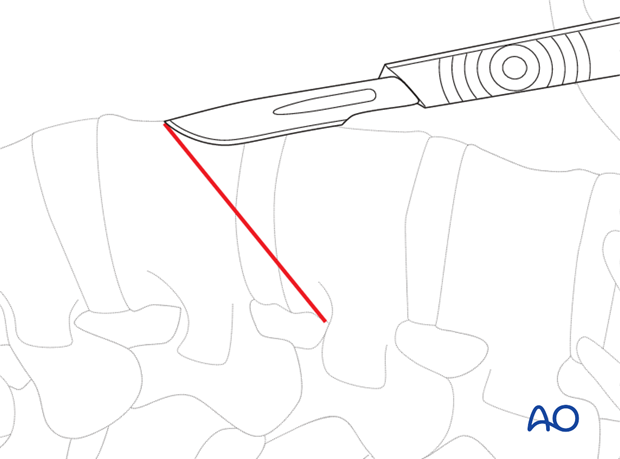
The skin is incised on the mark.
5. Exposure
There are three abdominal wall muscles. The first layer is the external abdominal oblique muscle, the second layer is the internal abdominal oblique muscle, and the third is the transverse abdominal muscle.
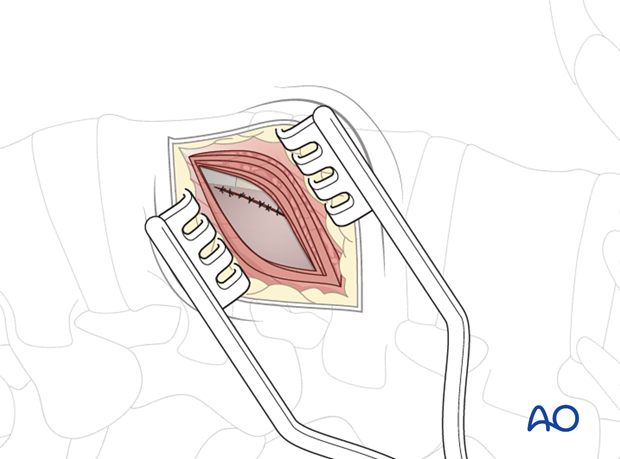
The subcutaneous tissue and the fascia of the obliquus externus muscle are dissected.
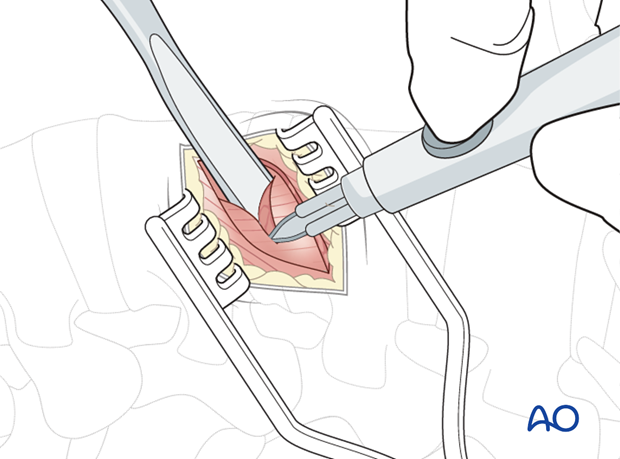
The first muscle layer is incised with cautery and retracted. The second layer is split and retracted.
The transversalis fascia is opened with caution to avoid injury to the peritoneum, which lies in the abdominal cavity.
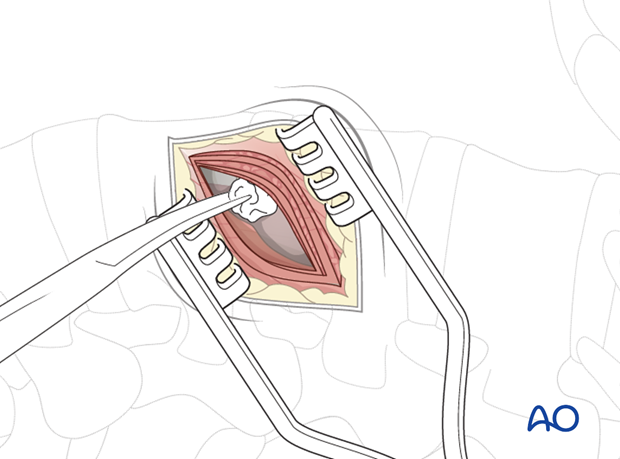
A finger is used to split the muscle and detach it from the peritoneum to facilitate dissection.
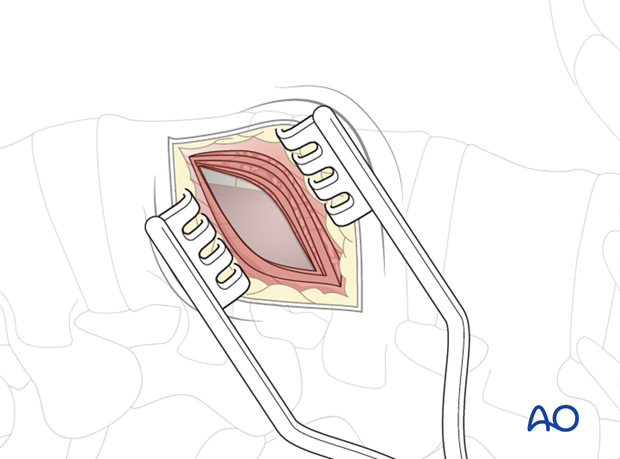
The retroperitoneal fat is a good landmark to detect the retroperitoneal space.
Pitfall: Injured peritoneum
If the peritoneum is injured, organs can be affected or postoperative herniation can occur.
If the peritoneum is violated, it is recommended that it be repaired directly with an absorbable suture and a blunt tapered needle.
The peritoneum has to be shifted away from the lateral abdominal wall until the psoas muscle is exposed.
The psoas muscle is exposed to facilitate posterior retraction.
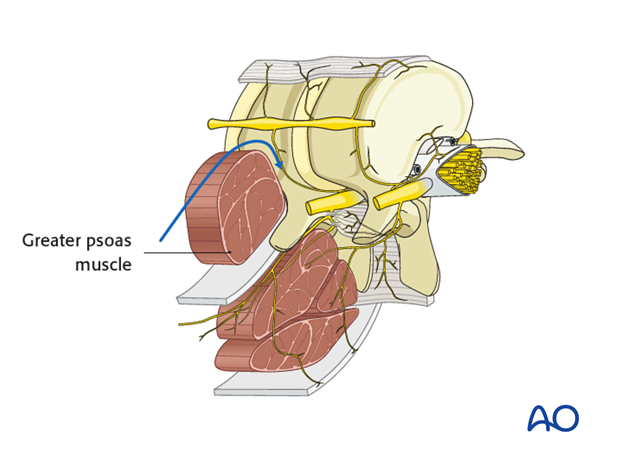
After exposing the psoas muscle, there are two options.
Option 1: The psoas muscle is anteriorly released and retracted posteriorly towards the spinal canal to expose the spine.
Option 2: The psoas muscle is bluntly split longitudinally to expose the spine, which is called transpsoas approach. If this option is used, neuromonitoring is recommended.
Directly postoperatively, many patients will complain about iliopsoas pain due to the mobilization of the psoas muscle. Mostly temporary nerve root lesions are quite common if the transpsoas approach is used.
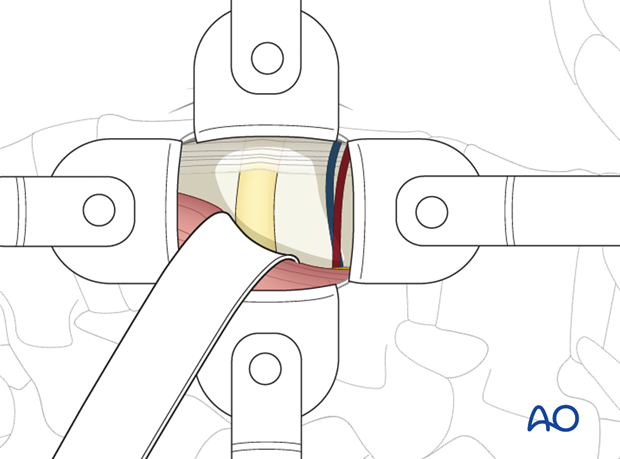
A self-retaining retractor system is necessary to allow the exposure of the spine.
6. Further dissection
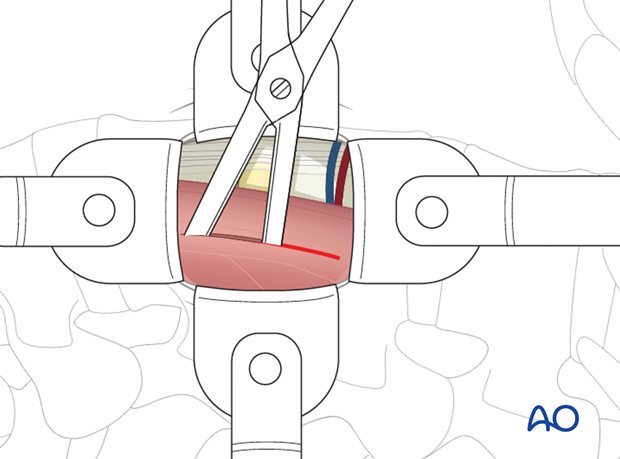
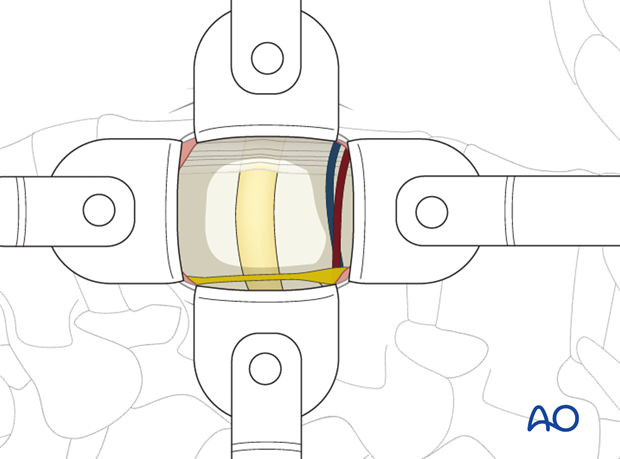
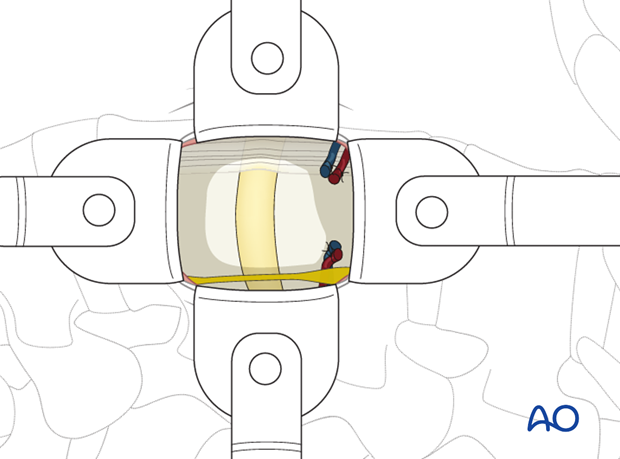
The segmental vessels above and below the fractured vertebra can be isolated, ligated with sutures and clips, and divided.
Next, the segmental vessels over the fractured vertebra can be isolated, ligated, and divided.
For anterior discectomies, these can be spared.
It is mandatory to have a table mounted retraction system to gently retract the psoas muscle, abdominal contents, and great vessels/sympathetic chain.
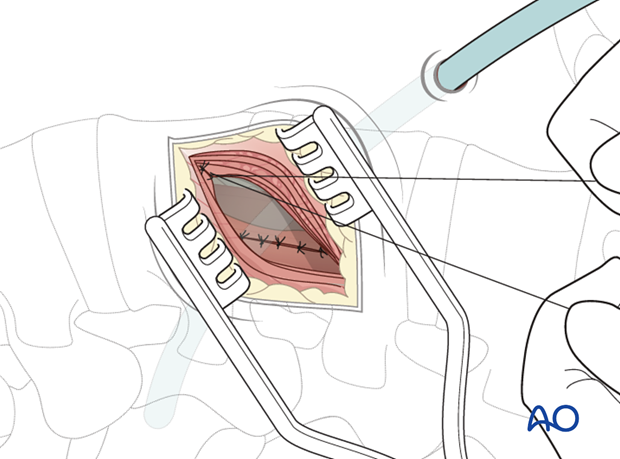
7. Closure
A retroperitoneal drain is inserted.
The wound is then closed in layers.